Latest Articles
19 Apr 2024 : Case report 
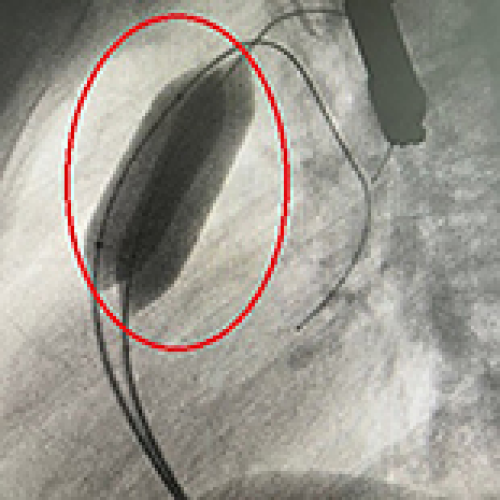
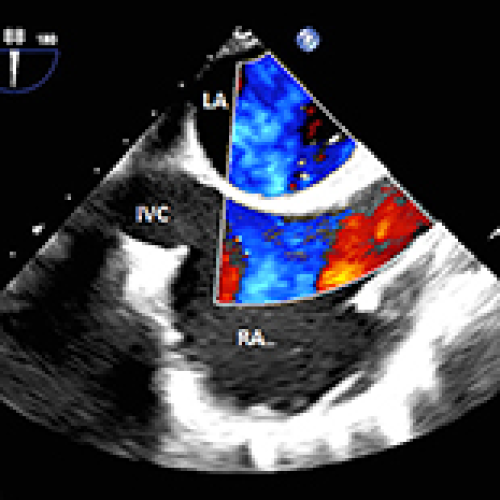
Simultaneous Transcatheter Closure of a Ventricular Septal Defect and Pulmonary Valvuloplasty: A Case Report
Baraa Alghalyini ![]() , Abdul Rehman Zia Zaidi
, Abdul Rehman Zia Zaidi
DOI: 10.12659/AJCR.942032
Am J Case Rep 2024; 25:e942032
19 Apr 2024 :
Case report 
Simultaneous Transcatheter Closure of a Ventricular Septal Defect and Pulmonary Valvuloplasty: A Case Report
Baraa Alghalyini ![]() , Abdul Rehman Zia Zaidi
, Abdul Rehman Zia Zaidi
DOI: 10.12659/AJCR.942032
Am J Case Rep 2024; 25:e942032
18 Apr 2024 : Case report 
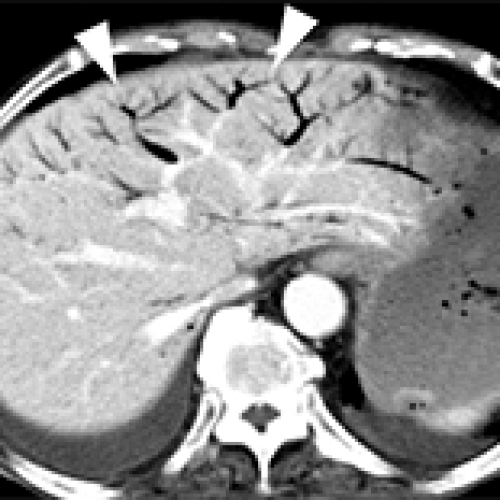
Potential Indicators of Intestinal Necrosis in Portal Venous Gas: A Case Report of an 82-Year-Old Woman on Long-Term Hemodialysis with Ascites and Pneumatosis Coli
Yoshio Hisata, Naoko E. Katsuki
DOI: 10.12659/AJCR.942966
Am J Case Rep 2024; 25:e942966
18 Apr 2024 : Case report 
Potential Indicators of Intestinal Necrosis in Portal Venous Gas: A Case Report of an 82-Year-Old Woman on Long-Term Hemodialysis with Ascites and Pneumatosis Coli
Yoshio Hisata, Naoko E. Katsuki
DOI: 10.12659/AJCR.942966
Am J Case Rep 2024; 25:e942966
18 Apr 2024 : Case report 
Transformation of Severe Aplastic Anemia into Donor Cell Leukemia after Allogeneic Hematopoietic Stem Cell Transplantation: A Rare Case Report
Qianqian Wang, Hong Xu
DOI: 10.12659/AJCR.943801
Am J Case Rep 2024; 25:e943801
18 Apr 2024 : Case report 
Transformation of Severe Aplastic Anemia into Donor Cell Leukemia after Allogeneic Hematopoietic Stem Cell Transplantation: A Rare Case Report
Qianqian Wang, Hong Xu
DOI: 10.12659/AJCR.943801
Am J Case Rep 2024; 25:e943801
17 Apr 2024 : Case report 
Successful Treatment Strategy for Duplicate Inferior Vena Cava and Deep Venous Thrombosis: Filter Placement and Thrombolysis Approach
DOI: 10.12659/AJCR.942578
Am J Case Rep 2024; 25:e942578
17 Apr 2024 : Case report 
Successful Treatment Strategy for Duplicate Inferior Vena Cava and Deep Venous Thrombosis: Filter Placement and Thrombolysis Approach
DOI: 10.12659/AJCR.942578
Am J Case Rep 2024; 25:e942578
17 Apr 2024 : Case report 
Intrapulmonary Shunting and Paradoxical Air Embolism in Liver Transplantation: A Case Report
Bradly Brown, Peter E. Frasco
DOI: 10.12659/AJCR.943042
Am J Case Rep 2024; 25:e943042
17 Apr 2024 : Case report 
Intrapulmonary Shunting and Paradoxical Air Embolism in Liver Transplantation: A Case Report
Bradly Brown, Peter E. Frasco
DOI: 10.12659/AJCR.943042
Am J Case Rep 2024; 25:e943042
16 Apr 2024 : Case report 
Nivolumab-Induced Cytokine Release Syndrome: A Case Report and Literature Review
Francis Ntwali, Quentin Gilliaux
DOI: 10.12659/AJCR.941835
Am J Case Rep 2024; 25:e941835
16 Apr 2024 : Case report 
Nivolumab-Induced Cytokine Release Syndrome: A Case Report and Literature Review
Francis Ntwali, Quentin Gilliaux
DOI: 10.12659/AJCR.941835
Am J Case Rep 2024; 25:e941835
16 Apr 2024 : Case report 
Unintentional Plastic Blister Ingestion Leading to Intestinal Perforation: A Report of Two Cases
Juli Celina Medina Gontier, Lea Wienandts
DOI: 10.12659/AJCR.943514
Am J Case Rep 2024; 25:e943514
16 Apr 2024 : Case report 
Unintentional Plastic Blister Ingestion Leading to Intestinal Perforation: A Report of Two Cases
Juli Celina Medina Gontier, Lea Wienandts
DOI: 10.12659/AJCR.943514
Am J Case Rep 2024; 25:e943514

15 Apr 2024 : Case report 
Complicated Treatment Course of Severe Asymptomatic Hypertriglyceridemia: A Case Report and Literature Review
Ahmad Wasfi Haddad ![]() , Mohammad N. Kloub
, Mohammad N. Kloub
DOI: 10.12659/AJCR.943858
Am J Case Rep 2024; 25:e943858

15 Apr 2024 : Case report 
Complicated Treatment Course of Severe Asymptomatic Hypertriglyceridemia: A Case Report and Literature Review
Ahmad Wasfi Haddad ![]() , Mohammad N. Kloub
, Mohammad N. Kloub
DOI: 10.12659/AJCR.943858
Am J Case Rep 2024; 25:e943858

15 Apr 2024 : Case report 
A 25-Year-Old Man with a History of Substance Abuse Presenting with Pneumomediastinum Due to Methamphetamine Vapor Inhalation
Anahita Shahnazi, Keenan Bayrakdar
DOI: 10.12659/AJCR.941509
Am J Case Rep 2024; 25:e941509

15 Apr 2024 : Case report 
A 25-Year-Old Man with a History of Substance Abuse Presenting with Pneumomediastinum Due to Methamphetamine Vapor Inhalation
Anahita Shahnazi, Keenan Bayrakdar
DOI: 10.12659/AJCR.941509
Am J Case Rep 2024; 25:e941509
14 Apr 2024 : Case report 
Pancreatolithiasis: Does Management Depend on Clinical Manifestations?
Daniel Paramythiotis, Eleni Karlafti
DOI: 10.12659/AJCR.942725
Am J Case Rep 2024; 25:e942725
14 Apr 2024 : Case report 
Pancreatolithiasis: Does Management Depend on Clinical Manifestations?
Daniel Paramythiotis, Eleni Karlafti
DOI: 10.12659/AJCR.942725
Am J Case Rep 2024; 25:e942725

13 Apr 2024 : Case report 
Successful Superficial Blood Sampling to Localize a Fibroblast Growth Factor-23-Producing Tumor
Junjiro Rikitake, Kenji Ashida ![]()
DOI: 10.12659/AJCR.943152
Am J Case Rep 2024; 25:e943152

13 Apr 2024 : Case report 
Successful Superficial Blood Sampling to Localize a Fibroblast Growth Factor-23-Producing Tumor
Junjiro Rikitake, Kenji Ashida ![]()
DOI: 10.12659/AJCR.943152
Am J Case Rep 2024; 25:e943152
12 Apr 2024 : Case report 
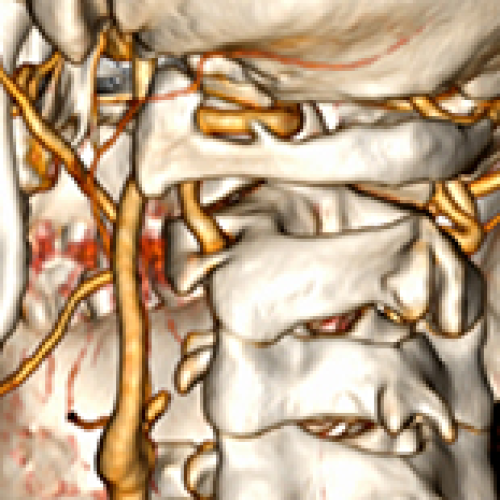
Bilateral Bow Hunter Syndrome Associated with Loss of Cervical Physiological Curvature
Shengwu Wang, Youcai Bi
DOI: 10.12659/AJCR.942609
Am J Case Rep 2024; 25:e942609

12 Apr 2024 : Case report 
Bilateral Bow Hunter Syndrome Associated with Loss of Cervical Physiological Curvature
Shengwu Wang, Youcai Bi
DOI: 10.12659/AJCR.942609
Am J Case Rep 2024; 25:e942609
11 Apr 2024 : Case report 
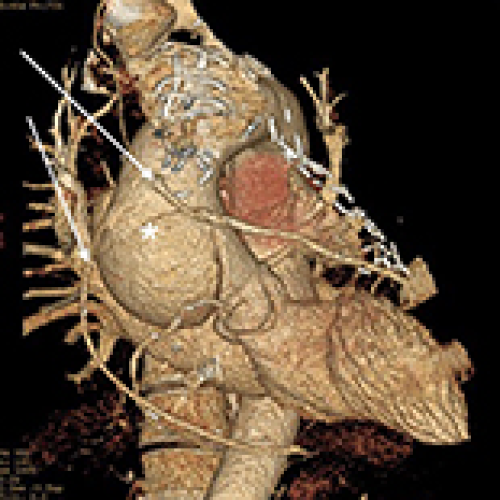
Type A aortic dissection after Coronary Artery Bypass Grafting
DOI: 10.12659/AJCR.942673
Am J Case Rep 2024; 25:e942673

11 Apr 2024 : Case report 
Type A aortic dissection after Coronary Artery Bypass Grafting
DOI: 10.12659/AJCR.942673
Am J Case Rep 2024; 25:e942673
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








