26 May 2022: Articles 
Anterior Mediastinal Myelolipoma: A Case Report and Review of the Literature
Unusual clinical course
Amnah Hassan AlSaffar1ABCEF*, Ahmed Mohammed AlEssa1ACD, Tarek AlSharkawy1AD, Naela B. Alamoudi2E, Fahd A. Makhdom3EDOI: 10.12659/AJCR.936005
Am J Case Rep 2022; 23:e936005
Abstract
BACKGROUND: Myelolipoma is a benign tumor, commonly found in the supra-renal gland, which is composed of mature fatty tissue admixed with hematopoietic elements. However, there are several extra-adrenal sites reported in the literature and thoracic myelolipoma is an unusual location for extra-adrenal myelolipoma.
CASE REPORT: We present the case of a 71-year-old man previously diagnosed with hypertension who was admitted due to a motor vehicle injury with a lumbar spine fracture. The patient developed non-ST segment elevation myocardial infarction during admission. A coronary angiogram revealed three-vessel disease. Triple coronary artery bypass grafting (CABG) surgery was planned. Upon opening the chest through median sternotomy, a retrosternal adherent mass was incidentally discovered. The mass was excised and histopathological evaluation showed it was myelolipoma in the anterior part of the mediastinum.
CONCLUSIONS: It is well known that myelolipoma occurs in extra-adrenal sites, and is rarely found at unexpected site, as in our case, which was found incidentally at the anterior mediastinum. With an extensive literature review, we found only 1 case located in the anterior mediastinum. It is crucial to know that myelolipoma can occur in the anterior mediastinum to avoid pitfalls with other differential diagnoses, especially when it is found incidentally and requires a frozen section examination, as it is difficult to diagnose through radiologic imaging only because it can overlap with tumors that are rich in either adipose tissue or hematopoietic elements. However, it affects patient management, and patients usually need only follow-up instead of going through invasive procedures for resection of non-functional tumors, especially in older patients or patients with comorbid diseases.
Keywords: Incidental Findings, Mediastinal Neoplasms, Myelolipoma, Thorax, Adipose Tissue, Adrenal Gland Neoplasms, Aged, Diagnosis, Differential, Humans, Male, Mediastinum
Background
Myelolipoma is a benign non-functional tumor. Most of them are asymptomatic and discovered incidentally, either through imaging studies or at autopsy, but whenever the lesion attains a large size, it can be clinically active and present with pain [1]. Rarely, there is an acute presentation secondary to rupture, necessitating surgical intervention [2,3]. While it most commonly occurs in the adrenal gland, it has also been reported at extra-adrenal sites; some of them are in the renal hilum, spleen, presacral region, retroperitoneum, stomach, omen-tum, nasal cavity, liver, testes, and even in the thyroid gland. They have rarely been identified in the thorax [4]. We present a rare case of mediastinal myelolipoma, composed of mature adipose tissue along with mature hematopoietic elements [5].
Case Report
PREOPERATIVE:
We present a case of a 71-year-old man previously diagnosed with hypertension, who was admitted after a motor vehicle injury causing a lumbar spine fracture. He developed non-ST segment elevation MI (NSTEMI) with a high troponin level (1.5 ng/mL) during admission. A coronary angiogram showed severe three-vessel disease. Triple coronary artery bypass grafting (CABG) surgery was planned.
INTRAOPERATIVE:
After opening the chest through median sternotomy, a retrosternal adherent mass was incidentally discovered. It was in the midline, fibrolipomatous in consistency, and measured 5×3 cm. The mass was excised, and a frozen section was done on scene, and it was indefinite and deferred for further pathologic examination on permanent sections. CABG surgery was done afterward.
PATHOLOGICAL FINDINGS:
Macroscopically, the lesion is tan-brown with a smooth outer surface, firm in consistency, and has a hemorrhagic cut surface, measuring 3.2×2.5×0.5 cm. A microscopic examination revealed islands of hematopoietic cells and mature adipose tissue, areas of hemorrhage and necrosis, and fibromyxoid degeneration and reactive bone formation (osseous metaplasia). The peripheral part of the lesion showed mature cartilaginous tissue (Figures 1–6). The diagnosis of myelolipoma was made with a recommendation to examine the patient for extramedullary hematopoiesis, as it is included in the differential diagnosis.
POSTOPERATIVE:
The patient tolerated the procedure well. The total cardiac intensive care unit stay was 4 days, and the total hospital stay was 17 days. The patient was discharged in a stable general condition with uneventful follow-ups.
Discussion
Myelolipoma is a benign tumor. Although it most commonly arises in the adrenal gland, it has been reported in several extra-adrenal sites. It accounts for <4% of primary adrenal gland tumors, with an incidence of 0.4% at autopsy (for extra-adrenal myelolipoma) [6]. It can occur at any age; however, the usual presentation for adrenal myelolipoma is the fifth decade [4]. These tumors can measure 20 cm or greater, with an average size of 5–10 cm [3]. Grossly, it is a well-circumscribed tumor with a yellow to red-brown cut surface, depending on the adipose tissue volume in relation to hematopoietic elements [7]. Findings under the microscope consist mainly of an admixture of mature adipose tissue and trilineage hematopoietic elements resembling bone marrow. Myelolipomas are distinct from actual bone marrow in that no reticular sinusoids or bone spicules are present [6]. It has been associated with Cushing syndrome, congenital adrenal hyperplasia, Addison disease, and long-term exogenous steroid use [7]. Myelolipomas manifest in 4 distinct clinicopathologic patterns: isolated adrenal myelolipoma, adrenal myelolipoma with hemorrhage, extra-adrenal myelolipoma, and myelolipoma associated with other adrenal diseases [9]. The majority of myelolipomas also have non-random chromosome inactivation, suggesting the clonal origin of these tumors [10,11]. As mediastinal myelolipoma does not have any pathognomonic signs or symptoms, it is difficult to definitively diagnose without histopathologic evaluations, although ultrasonography, CT scan, and MRI have become more common as valuable diagnostic tools and to give some clues to the correct diagnosis [12].
In general, the differential diagnosis of mediastinal mass depends on the location.
Our case was located at the anterior mediastinum. The most common differential diagnoses of lesions at this location include thymic carcinoma, thymoma, thyroid neoplasm, germ cell tumor, and lymphoma, but HE features of the lesion raise other differential diagnoses, including extramedullary hematopoiesis, lipoma, liposarcoma, and myeloid sarcoma [9]. Extramedullary hematopoiesis usually occurs as a manifestation of myeloproliferative diseases or is a compensatory phenomenon in various chronic anemias. Extramedullary hematopoiesis is composed predominantly of hematopoietic cells and erythroid hyperplasia without adipose tissue components. Extramedullary hematopoiesis is distinguished from myelolipoma by the presence of diffuse extramedullary hematopoiesis, splenomegaly or other organomegaly, chronic anemia, and marked hyperplasia of the bone marrow [5]. Lipoma is a benign adipocytic tumor composed mainly of mature lobulated fat. It is part of the differential diagnosis when myelolipoma is composed predominantly of fatty tissue; however, extensive sampling can exclude it. Well-differentiated liposarcoma/atypical lipomatous tumor is an adipocytic tumor that shares many radiological characteristics with myelolipoma, which makes it part of the differential diagnosis [9]. However, the cut surface of the well-differentiated liposarcoma is not hemorrhagic. The histological picture has infiltrative growth [13] and is composed of scattered large atypical cells admixed with variable-size adipocytes and several lipoblasts. Again, it does not contain bone marrow elements; however, molecular testing of MDM2 is often positive in well-differentiated liposarcoma and can be used [2,7]. Myeloid sarcoma (also called chloroma) is a malignant soft tissue tumor mainly composed of immature bone marrow elements in contrast to myelolipoma, in which present bone marrow elements are mature. Also, it does not contain fatty tissue [14].
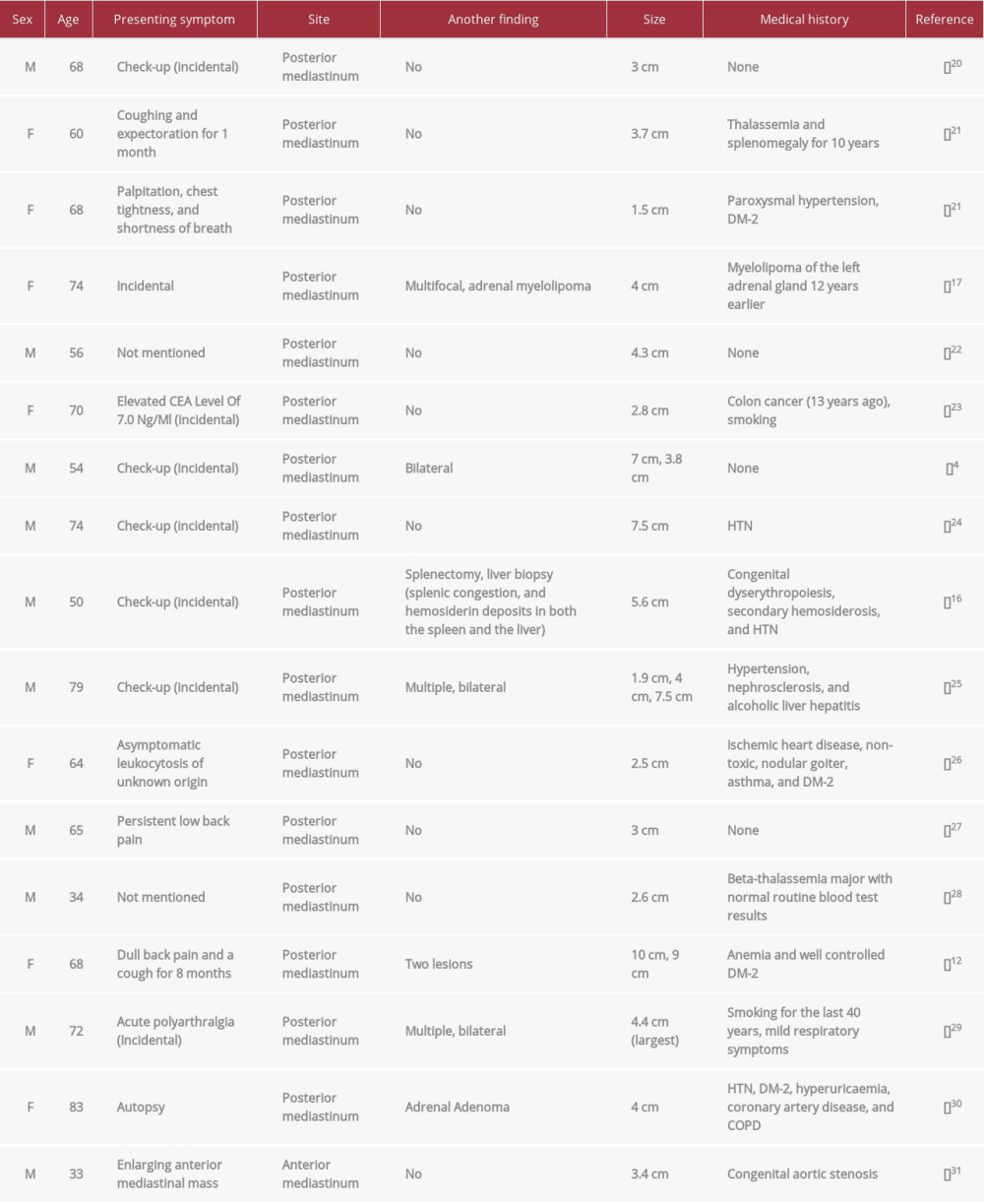
After an extensive review of the literature, we found 39 published cases of extra-adrenal myelolipomas, including 22 males and 17 females, with a range of age from 18 to 91 years old, of which 16 cases were in the posterior mediastinum and only 1 case was in the anterior mediastinum. Depending on the tumor’s location, presenting symptoms are variable; 11 of them were incidental findings and 3 were found at autopsy [15,16]. No common diseases are associated with it other than DM, HTN, and coronary artery disease. There is a case of retroperitoneal myelolipoma coincident with gastric spindle cell neoplasm [9], a case of the posterior mediastinum with a history of adrenal myelolipoma 12 years earlier [17], a patient with the synchronous occurrence of hepatic myelolipoma and 2 hepato-cellular carcinomas [18], and a pelvic myelolipoma infiltrated by CLL/SLL [19]. Table 1 is a demographic table that shows and summarizes the clinical characteristics of these patients with anterior and posterior mediastinal location.
Conclusions
Myelolipoma is an uncommon benign tumor that most commonly occurs in the adrenal gland and is also identified in extra-adrenal sites, including the liver, spleen, kidney, presacral region, retroperitoneum, and mediastinum. It is asymptomatic and diagnosed incidentally through radiological study. Macroscopically, it consists of a well-circumscribed, round-oval mass with a yellow to red-brown cut surface. Microscopically it is characterized by mature adipose tissue along with hematopoietic cells elements. However, the variable proportions of adipocytic tissue, hematopoietic elements, and hemorrhage can make the radiographic diagnosis more challenging and can be non-specific, especially at extra-adrenal sites. Myelolipoma shows typical macroscopic and microscopic findings, so knowing that myelolipoma can occur in extra-adrenal sites is crucial, as it can occur at unexpected sites, considering its differential diagnosis.
Figures
References:
1.. Yugandhar S, Sureka SK, Yadav P, Lal H, A rare case of extra-adrenal bilateral perirenal and periureteric myelolipoma: BMJ Case Rep, 2017; 2017; bcr2017221846
2.. Aguilera NS, Auerbach A, Extra-adrenal myelolipoma presenting in the spleen: A report of two cases: Hum Pathol Case Rep, 2016; 6; 8-12
3.. Mariappan MR, Fadare O, Ocal IT, Pathologic quiz case: A 74-year-old man with an incidental retroperitoneal: Tumour found at autopsy: Arch Pathol Lab Med, 2004; 128(5); 591-92
4.. Shen C, Han Z, Che G, A bilateral neoplasm in chest: A case report and literature review: BMC Surg, 2014; 14(1); 14-42
5.. Talwalkar SS, Shaheen SP, Extra-adrenal myelolipoma in the renal hilum: A case report and review of the literature: Arch Pathol Lab Med, 2006; 130(7); 1049-52
6.. Xuefeng T, Rui C, Jianping X, Mingfu Y, Myelolipoma of the kidney: A seldom site for a rare extra-adrenal tumor: Journal of Medical Colleges of PLA, 2010; 25(5); 317-320
7.. Baker KS, Lee D, Huang M, Gould ES, Presacral myelolipoma: A case report and review of imaging findings: J Radiol Case Rep, 2012; 6(6); 1-9
8.. Sohoni CA, Extra-adrenal myelolipoma: A rare entity in paediatric age group: APSP J Case Rep, 2013; 4(3); 36
9.. Yildiz BD, Giant extra-adrenal retroperitoneal myelolipoma with incidental gastric mesenchymal neoplasias: Int Surg, 2015; 100(6); 1018-20
10.. Elena Bishop, Eble JN, Cheng L, Adrenal myelolipomas show nonrandom X-chromosome inactivation in hematopoietic elements and fat: Support for a clonal origin of myelolipomas: Am J Surg Pathol, 2006; 30(7); 838-43
11.. Sato K, Ueda Y, Katsuda S, Tsuchihara K, Myelolipoma of the lung: A case report and brief review: J Clin Pathol, 2007; 60(6); 728-30
12.. Geng C, Liu N, Yang G, Chen W, Primary mediastinal myelolipoma: A case report and review of the literature: Oncol Lett J, 2013; 5(3); 862-64
13.. Leite MI, Gonçalves A, Ferreira AC, An unusual fat containing presacral tumor in an elderly patient: J Radiol Case Rep, 2016; 2014; 1-6
14.. Zhou J, Bell D, Medeiros J, Myeloid sarcoma of the head and neck region: Arch Pathol Lab Med, 2013; 137(11); 1560-68
15.. Mašić S, Vučić M, Seiwerth S, Pulmonary myelolipoma containing osseous tissue: An unexpected finding at autopsy: Respir Med Case Rep, 2017; 22; 254-56
16.. Oliveira CC, Junior GF, Camolese VH, Myelolipoma of the posterior mediastinum in a patient with chronic dyserythropoietic anemia: Autops Case Rep, 2016; 6(3); 35-39
17.. Haro A, Fujishita T, Nishikawa H, A rare case of gradual enlargement of a multifocal myelolipoma of the posterior mediastinum for 12 years after surgical resection of an adrenal myelolipoma: Int J Surg Case Rep, 2018; 51; 400-3
18.. Xu SY, Xie HY, Zhou L, Synchronous occurrence of a hepatic myelolipoma and two hepatocellular carcinomas: World J. Gastroenterol, 2016; 22(43); 9654
19.. Arora K, Sidhu J, Extra-adrenal myelolipoma containing small lymphocytic lymphoma/chronic lymphocytic leukemia: A case report and review of the literature: Case Rep Hematol, 2016; 2016; 1-6
20.. Ema T, Kawano R, Myelolipoma of the posterior mediastinum: Report of a case: Gen Thorac Cardiovasc Surg, 2013; 62(4); 241-43
21.. Xiong Y, Wang Y, Lin Y, Primary myelolipoma in posterior mediastinum: J Thorac Dis, 2014; 6(9); 181-87
22.. Himuro N, Minakata T, Oshima Y, Video-assisted thoracic surgery for primary myelolipoma of the posterior mediastinum: J. Cardiothorac Surg, 2016; 11(1); 1
23.. Hosaka T, Hata Y, Makino T, Mediastinal myelolipoma showing gradual enlargement over 9 years: A case report: J Cardiothorac Surg, 2016; 11; 91
24.. Shi Q, Pan S, Bao Y, Primary mediastinal myelolipoma: A case report and literature review: J Thorac Dis, 2017; 9(3); 219-25
25.. Nakagawa M, Kohno T, Mun M, Yoshiya T, Bilateral video-assisted thoracoscopic surgery resection for multiple mediastinal myelolipoma: Report of a case: Korean J Thorac Cardiovasc Surg, 2014; 47(2); 189-92
26.. Fonda P, de Santiago E, Guijarro M, Gamallo C, Mediastinal myelolipoma with leukocytosis: BMJ Case Rep, 2013; 2013; bcr2013010349
27.. Ventura L, Martella EM, Rusca M, Ampollini L, Posterior mediastinal myelolipoma resected by video-assisted thoracic surgery: J. Minim Access Surg, 2019; 15(1); 65-67
28.. Muriana P, Negri G, An unusual case of a posterior mediastinal myelolipoma in a patient with Mediterranean anemia: Pan Afr Med J, 2018; 31; 58
29.. Qin D, Ren X, Zheng S, Bi H, An unusual diagnosis of paravertebral lesions: Mediastinal myelolipoma: Int J Med Res, 2020; 48(7); 300060520936972
30.. Schittenhelm J, Jacob SN, Rutczynska J, Extra adrenal paravertebral myelolipoma mimicking a thoracic schwannoma: BMJ Case Rep, 2009; 2009; bcr0720080561
31.. Mehta C, Raparia K, Bharat A, Anterior mediastinal myelolipoma: Ann Thorac Surg, 2017; 103(1); 81
Figures
In Press
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942864
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250