08 May 2022: Articles 
and Bacteremia in a Patient with Acute Obstructive Suppurative Cholangitis: A Case Report and Review of the Literature
Mistake in diagnosis, Diagnostic / therapeutic accidents, Management of emergency care, Unexpected drug reaction, Rare disease, Clinical situation which can not be reproduced for ethical reasons
Pan Zhang1ACG*, Na Jiang1B, Limin Xu1C, Zhenhua Shen1F, Xinghui Liu1D, Xiaoyan Cai2GDOI: 10.12659/AJCR.936329
Am J Case Rep 2022; 23:e936329
Abstract
BACKGROUND: Clostridium perfringens (CP), one of several clostridial species gram-positive bacteria, is a major cause of animal necrosis enteritis and traumatic gangrene. In some reports, CP can cause acute emphysematous cholecystitis in patients with biliary tract infections. However, C. perfringens combined with other aerobic bacteria (eg, E. coli) in bloodstream co-infection is extremely rare and often fatal. Herein, we present a case of co-infection to underscore this unusual situation so that clinicians can adequately evaluate and treat patients in time.
CASE REPORT: A 74-year-old man presented to the Emergency Department half a day after the onset of acute abdominal pain accompanied by nausea, vomiting, and chills. The patient was admitted, following development of jaundice, chills, high fever, confusion, and shock. Computed tomography (CT) revealed that the patient had cholangiectasis with acute obstructive suppurative cholangitis (AOSC). We subsequently performed percutaneous transhepatic gallbladder drainage surgery combined with antibiotics, including ceftriaxone, levofloxacin, and metronidazole. C. perfringens and Escherichia coli infections were identified by in vitro blood culture. Fortunately, the patient responded favorably to treatment in our hospital and was cured within 1 week.
CONCLUSIONS: We report a rare case of C. perfringens and E. coli bloodstream co-infection in a patient with AOSC. We suggest that anaerobic and aerobic co-infection should be considered in future clinical diagnoses. Effective antibiotic treatment combined with surgical drainage is crucial if mixed infection occurs.
Keywords: Clostridium Infections, coinfection, Microbiology, Bacterial Infections, Escherichia coli Infections, Anti-Bacterial Agents, Bacteremia, Chills, Cholangitis, Clostridium perfringens, Escherichia coli, Humans, Sepsis, Suppuration
Background
Rare cases of
Herein, we present a case report of a patient with acute obstructive suppurative cholangitis with
Case Report
On 30 Oct 2017, a 74-year-old man presented to the Emergency Department of Shanghai Pudong New Area Gongli Hospital after he had begun to experience abdominal pain for half a day. He was febrile (38.7°C) and had a pulse rate of 113 times/min, breathing rate of 20 times/min, and blood pressure of 112/69 mmHg. A repeat computed tomography (CT) scan of the abdomen was obtained, which showed a significant gallbladder enlargement and dilated common bile duct, indicating the possibility of bile duct calculus (Figure 1A, 1B). A blood test demonstrated a high count of WBC and neutrophils, as well as an abnormal liver function index (Table 1). Above all, the patient was diagnosed with a biliary tract infection and was taken to the Department of Gastroenterology. After clinical admission, the patient completed relevant examinations and fasting. A total of 4 bilateral blood culture flasks (aerobic culture and anaerobic culture) were sent to the Clinical Bacteriology Department for examination. The treatment course was carefully determined and administered, which include the anti-infective drugs ceftazidime and levofloxacin. However, the symptoms worsened, including persistent abdominal pain, jaundice, chills, and confusion, the temperature rose to 40.4°C, heart rate of 100 beats/min, and blood pressure of 95/50 mmHg. Due to concern about septic shock and acute obstructive suppurative cholangitis, the patient was immediately transferred to the Department of Surgery at 8 PM. The antibiotic treatment regimen was adjusted to ceftriaxone and metronidazole sodium chloride injection. The patient underwent percutaneous transhepatic gallbladder drainage the next day, and his body temperature dropped to 36.5°C and remained normal for 72 h. On 1 Nov, the patient underwent magnetic resonance cholangiogram cryptography (MRCP), which showed the gallbladder was contracted and there were fewer common bile duct calculi (Figure 1C, 1D).
Both anaerobic and aerobic flasks cultivational tests were positive after 12 h of incubation. The specific identification steps were performed. Gas was detected in the anaerobic flask, and direct image microscopic examination found coarse gram-positive bacilli, implying the possibility of anaerobic bacilli infection and the clinician was notified immediately (Figure 2A, 2B). Bacterial colonies with off-white, oblique, and hemolysis rings were detected on the plate after 24 h of anaerobic culture. Staining of colony smears showed blunt-rounded gram-positive bacilli (Figure 2C). The colonies were selected and subsequently identified as
On 4 Nov, the patient continued to improve and was discharged from the hospital. A review CT after 1 week showed improved outcomes (Figure 1E, 1F). Three months later, the patient underwent the surgical combined treatment of cholecystectomy and choledochotomy by choledochoscopy with T-tube drainage.
We searched the literature for all cases of
Discussion
Therefore, it is necessary to establish effective guidelines for the treatment of
The biliary tract infections, including cholecystitis and cholangitis, are usually secondary to predisposing factors leading to bacteremia or sepsis. In clinical practice, some biliary tract microbial agents are gram-negative bacteria, as well as fungi. A previous study showed that 60.9% of patients have bacterial infections, of which
In the present case, the patient was diagnosed with acute obstructive suppurative cholangitis based on clinical symptoms and imaging. Subsequently, the patient received relevant assessment after admission and we adjusted treatment strategies according to the clinical report. Fortunately, the patient did not have serious clinical outcomes, although he also had clinical symptoms such as high fever and cognitive deficits. A positive clinical response often depends on timely and effective treatment. The bloodstream infectious source is most likely via a damaged biliary tract caused by inflammation. Although the causes and mechanisms of this bloodstream mixed infection are still unclear, a possible explanation is a decreased ratio of oxygen in the blood due to
Limitations of this case report include the absence of anaerobic culture of gallbladder drainage fluid, leading to the inability to identify the source of bloodstream infection, and insufficient evidence of
Conclusions
We presented a rare case suggesting that bloodstream infection by
Figures
References:
1.. Kiu R, Hall LJ: Emerg Microbes Infect, 2018; 7; 1-15
2.. Simon TG, Bradley J, Jones A, Carino G: J Intensive Care Med, 2014; 29; 327-33
3.. McIlwaine K, Leach MTJ: Br J Haematol, 2013; 163; 549
4.. Kurasawa M, Nishikido T, Koike J, Gas-forming liver abscess associated with rapid hemolysis in a diabetic patient: World J Diabetes, 2014; 5; 224-29
5.. Castro R, Mendes J, Amaral L: J Surg Case Rep, 2017; 6; rjx116
6.. Kiu R, Hall LJ: Emerg Microbes Infect, 2018; 7; 141
7.. Law S-T, Lee MK: World J Hepatol, 2012; 4; 252-55
8.. Ballal M, Shenoy PA, Gabriel SR, Biliary tract infections and their microbiological spectrum – a study from coastal region of Southern India: Revista Infection, 2019; 23; 253-58
9.. Tally FP, Gorbach SL, Therapy of mixed anaerobic-aerobic infections: Am J Med, 1985; 78; 145-53
10.. Jasnosz KM, Shakir AM, Perper JA: Am J Forensic Med Pathol, 1993; 14; 151-54
11.. Uojima H, Onoue M, Hidaka H: J Med Case Rep, 2019; 13; 125
12.. Bari K, Aslanian HR, Pollak J, Emphysematous cholecystitis resulting in secondary biliary cirrhosis: A rare complication of endoscopic retrograde cholangiopancreatography: ACG Case Rep J, 2013; 1; 51-54
13.. Chinen K: Autops Case Rep, 2020; 10; e2020185
14.. Zapata PE, Penide EA, Guillén AB: Rev Esp Anestesiol Reanim, 2010; 57; 314-16
15.. Tsai IK, Yen MY, Ho IC: Scand J Infect Dis, 1989; 21; 467-71
16.. Van Bunderen CC, Bomers MK, Wesdorp E: Neth J Med, 2010; 68; 343-46
17.. Bush GW, Clements RH, Phillips M, Kent RB: Am Surg, 1996; 62(4); 326-27
18.. Wild W, Bormann F, Sweiti H: Case Rep Med, 2018; 2018; 4278904
19.. Koole SN, Lohman BG, van Unen JM: Acta Chir Belg, 2016; 116(1); 54-57
20.. Azimirad M, Yadegar A, Asadzadeh Aghdaei H, Kelly CR: J Crohns Colitis, 2019; 13(7); 960-61
21.. Walker HN, Liew KC, Adams V: Med J Aust, 2020; 213(3); 114-15
22.. Sarvari KP, Vasas B, Kiss I: Anaerobe, 2016; 40; 31-34
23.. Hagiya H, Naito H, Sugiyama J: Intern Med, 2012; 51(20); 2973-76
24.. España Fuente L, Soto Mesa D, Fernández Díez A: Rev Esp Anestesiol Reanim, 2011; 58(2); 129-31
25.. Eltawansy SA, Merchant C, Atluri P, Dwivedi S: Am J Case Rep, 2015; 16; 182-86
26.. De Zylva J, Padley J, Badbess R, Dedigama M, Multiorgan failure following gastroenteritis: A case report: J Med Case Rep, 2020; 14(1); 74
27.. Kirchhoff P, Müller V, Petrowsky H, Clavien PA: Surgery, 2007; 141(3); 411-12
28.. Miyahara H, Shida D, Matsunaga H, Emphysematous cholecystitis with massive gas in the abdominal cavity: World J Gastroenterol, 2013; 19(4); 604-6
29.. Wuorela M, Räihä I: Scand J Gastroenterol, 2000; 35(5); 559-60
30.. Zeng S, Tsia Hin Fong CJ, Acute hemorrhagic necrotizing enteritis: A case report and review of the literature: Ann Palliat Med, 2021; 10(5); 5853-61
31.. Bouras G, Lunca S, Vix M, Marescaux J, A case of emphysematous cholecystitis managed by laparoscopic surgery: JSLS, 2005; 9(4); 478-80
32.. Takemura K, Sekoguchi S, Yamane S: Nihon Shokakibyo Gakkai Zasshi, 2018; 115(6); 554-62
33.. Alsammani MA, Ahmed SR, Alsheeha MA: J Obstet Gynaecol Res, 2012; 38; 1024-27
34.. Wang X, Ren W, Nie Y: Vet J, 2013; 197; 812-16
35.. Ribeiro MG, Lara GHB, Bicudo SD: Arq Bras Med Vet. Zootec, 2007; 59; 810-12
36.. Diniz AN, Silva ROS, Oliveira Junior CA: Anaerobe, 2016; 38; 94-96
37.. Dahl SS, Thorsteinsson M, Lambine TL, Penninga L: BMJ Case Rep, 2020; 13; e238896
Figures
Tables
 Table 1.. Summary of the laboratory data.
Table 1.. Summary of the laboratory data.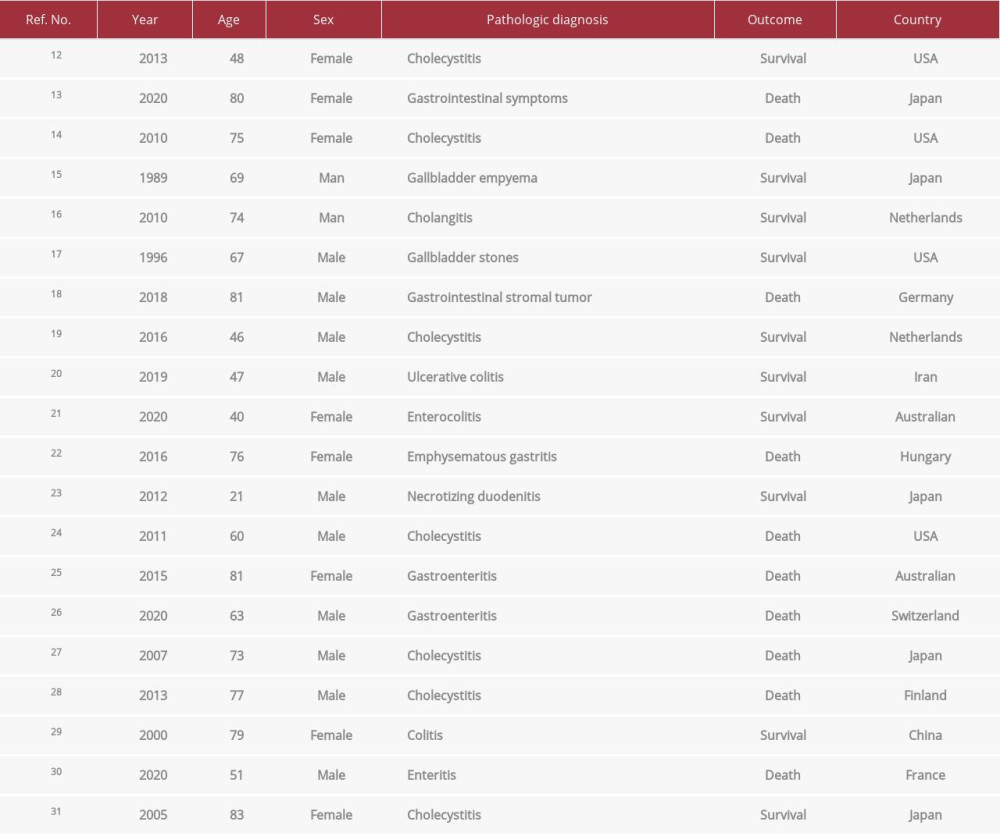 Table 2.. Cases of C. perfringens bloodstream infection in humans with gastrointestinal disease.
Table 2.. Cases of C. perfringens bloodstream infection in humans with gastrointestinal disease.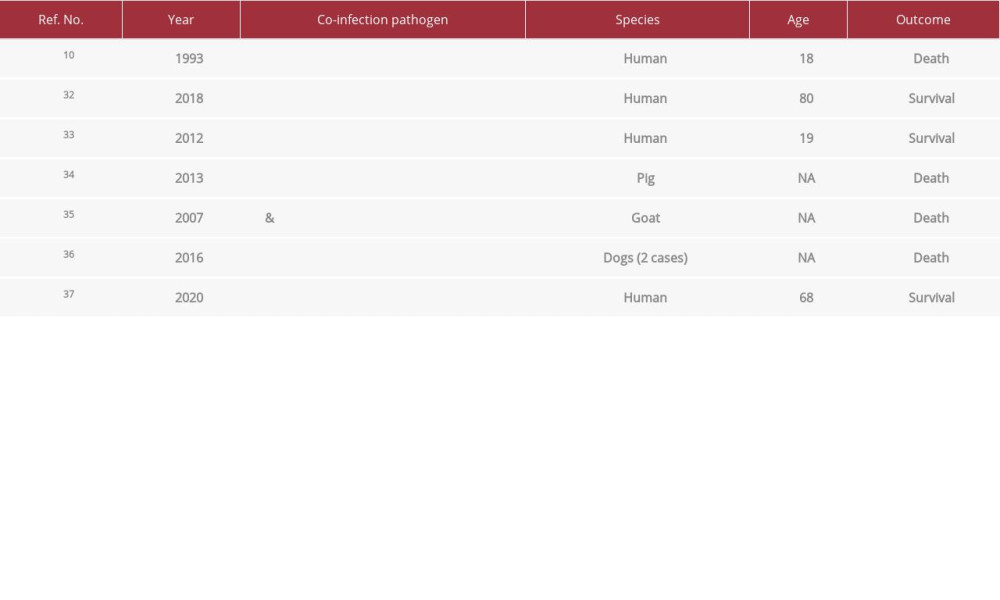 Table 3.. Cases of Clostridium perfringens co-infection pathogens.
Table 3.. Cases of Clostridium perfringens co-infection pathogens. Table 1.. Summary of the laboratory data.
Table 1.. Summary of the laboratory data.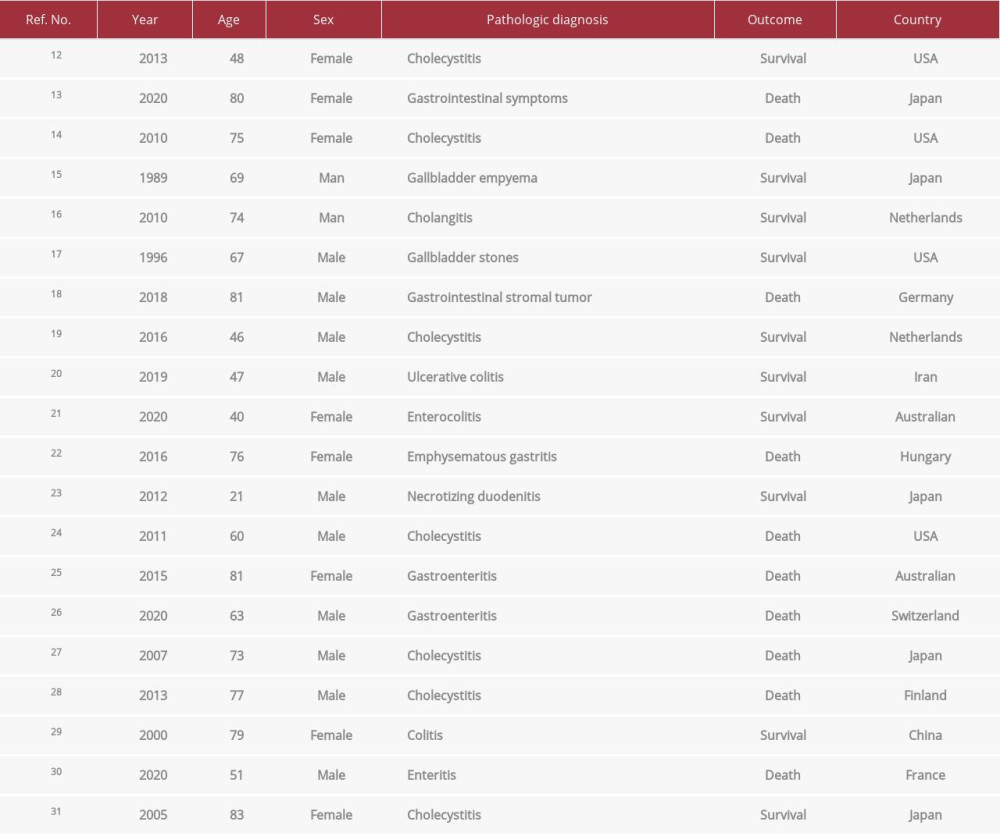 Table 2.. Cases of C. perfringens bloodstream infection in humans with gastrointestinal disease.
Table 2.. Cases of C. perfringens bloodstream infection in humans with gastrointestinal disease.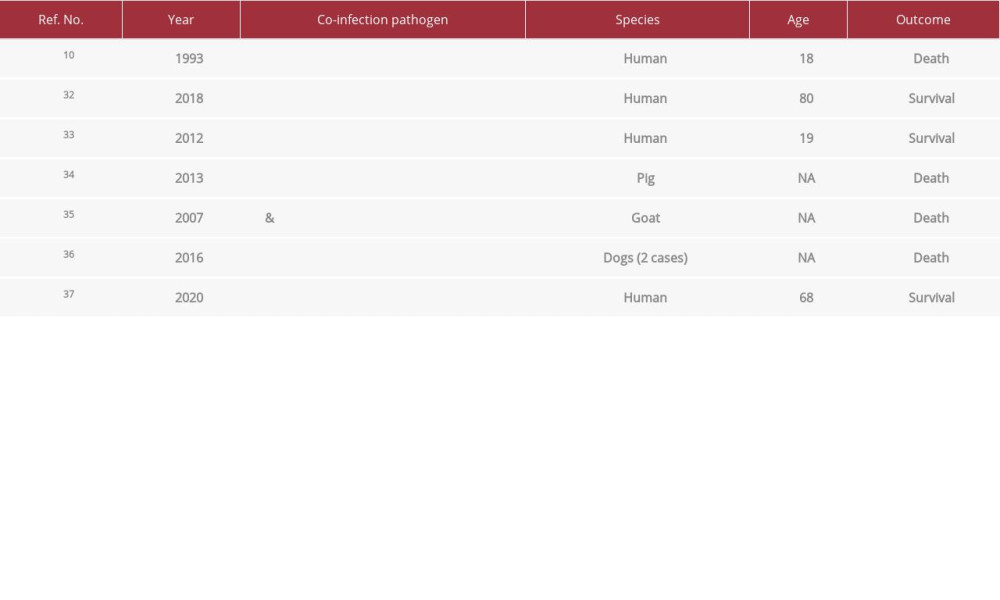 Table 3.. Cases of Clostridium perfringens co-infection pathogens.
Table 3.. Cases of Clostridium perfringens co-infection pathogens. In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943420
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942824
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








