14 November 2022: Articles 
Should a Living Donor Renal Graft be Removed Due To Prolonged Delayed Function? A Case Report
Unusual clinical course, Challenging differential diagnosis, Unusual or unexpected effect of treatment
Ahmed Salem Al-Thahir1EF, Ali Abdullah Al-Yami1AD, Emadeldeen Saeed1F, Rafat Zahid1AD, Hamad Mohd Al-Bahili1AD, Ioannis Theodoropoulos1ABCD*DOI: 10.12659/AJCR.936921
Am J Case Rep 2022; 23:e936921
Abstract
BACKGROUND: Delayed graft function (DGF) is defined as failure of the transplanted kidney to function in the early post-transplant period. DGF is a rare complication after living donor kidney transplant and is most common after deceased donor kidney transplant, probably due to prolonged warm and cold ischemia times during retrieval. Most cases of DGF resolve spontaneously within days to weeks. There are very few reported cases in the literature of DGF lasting over 4 weeks. We present a case that resolved after 55 days. The recipient subsequently achieved normal renal function.
CASE REPORT: Our patient was a 52-year-old man with end-stage renal disease who underwent a second living donor renal transplant. The donor was his son, with whom he had 1 antigen mismatch. Postoperative day 1, the patient developed anuria and failed to improve with fluids and diuretics. Investigations ruled out common causes of renal dysfunction (rejection, ischemia), but failed to disclose the cause of this condition. After an extended period of watchful waiting, the graft function returned, reaching normal creatinine and urine output levels.
CONCLUSIONS: DGF after living donor kidney transplantation is rare, and few cases lasting more than a month have been reported. Before diagnosing DGF, other causes of renal dysfunction (rejection, ischemia, medication adverse effects) must be ruled out. In the absence of these, expectant management is appropriate and full graft recovery can be expected, even with anuria and hemodialysis.
Keywords: Kidney Transplantation, Delayed Graft Function, Living Donors, case reports, Male, Humans, Middle Aged, Graft Survival, Graft Rejection, Anuria, Time Factors, Tissue Donors, Kidney, Risk Factors
Background
Delayed graft function (DGF) is a rare complication [1,2] after living donor kidney transplant (LDKT) compared with in deceased donor kidney transplant (DDKT), mostly due to the limited injury to the graft during warm ischemia and cold ischemia time. Although the exact cause of DGF usually remains obscure, the treatment is mostly nonspecific, with the elimination of other diagnoses (most notably rejection), discontinuation of nephrotoxic medication, and supportive care with dialysis. Most cases of DGF are expected to resolve within 28 days, with chances of full recovery decreasing as this time frame increases [3]. We present a case of DGF after LDKT that resolved after 55 days in a recipient with low immunologic risk who underwent a second transplant. He was able to achieve complete recovery despite the prolonged duration of the complication.
Case Report
Our patient was a 52-year-old man, weighing 76 kg, with end-stage renal disease. His past medical history included hyper-tension and hepatitis C virus infection (genotype 3) for which he was treated with dasabuvir for 3 months, then the combination of glecaprevir and pibrentasvir for another 3 months, with sustained complete viral response and normal hepatic function. He had undergone a living non-related renal transplant in 2006. The graft failed in 2015 due to chronic rejection, and the patient had anuria on hemodialysis via his upper extremity fistula ever since.
The patient was admitted electively for LDKT. The donor was his son, and the crossmatch by complement-dependent cytotoxicity showed T cells and B cells were both <2%, whereas crossmatch by IgG flow cytometry showed T cells <39% and B cells <54%, and both were considered negative.
Human leukocyte antigen (HLA) matching was done and showed a match for A24, B8, B15, Cw4, Cw7, DR3, and DQ2, and a mismatch for only DR4. Basiliximab was used for induction immunosuppression. The graft had 2 arteries, which were reconstructed in a pantaloon fashion, and a solitary vein. It was implanted on the left external iliac vessels, which displayed minimal atherosclerotic changes. A stented uretero-vesical anastomosis was created using the Lich-Gregoir technique, as per our department’s protocol. There were no complications during the implantation, with a warm ischemia time of 33 s, blood loss of 300 cc, and graft urine production of 80 cc. An intraoperative ultrasound showed good perfusion of the transplanted kidney, with a resistive index of the main renal artery of 0.7. The donor procedure was unremarkable as well, with the graft being exposed to 1 min 45 s of warm ischemia time.
The patient remained hypertensive (170/80 mmHg) overnight, with a good urine output ranging from 100 to 1500 cc/h. His urine output tapered to zero in the early morning hours and failed to improve with fluid boluses and diuretics. At this point, he had fluid overload and required hemodialysis. A repeated ultrasound was unremarkable. His creatinine levels on the first 3 days after surgery were 501, 525, and 598 mcmol/L, respectively.
On postoperative day (POD) 3, no improvement in the renal function was noted, and the patient was taken to the operating room for exploration following a slight increase in the resistive index, to 0.85 (with the rest of the vasculature remaining patent) on repeat ultrasound, raising concerns for early out-flow obstruction. The graft was intact and only biopsies were taken, which showed dense acute tubular necrosis, without signs of rejection or ischemia. On electron microscopy, mild glomerular membrane thickening and foot process effacement were reported, without deposits or multilayering.
Acute tubular necrosis was confirmed by renogram, which showed decreased perfusion but no excretion of radioactive material. At this point, the induction immunosuppression was changed to anti-thymocyte globulin, with a total dose of 450 mg (6 mg/kg). Daily dosing was adjusted based on CD 3 level. Regarding the rest of his immunosuppression regiment, mycophenolate mofetil was started immediately after the transplant at a dose of 1000 mg twice a day, while tacrolimus was initiated on POD 45 at 3.5 mg per day, and its level was intentionally kept <6 to minimize nephrotoxicity.
Over the next 4 weeks, the patient continued to have anuria and required regular hemodialysis every 2 to 3 days. Hospital-acquired pneumonia was diagnosed based on diffuse patchy infiltrates in his chest X-ray and mild dyspnea requiring oxygen supplementation via nasal canula. He was successfully treated with empiric antibiotics after immunosuppression had been temporarily minimized.
A repeated complement-dependent cytotoxicity and flow cytometry crossmatch on POD 21 did not reveal any donor-specific antibodies, while repeat ultrasounds were significant only for slightly elevated resistive indexes (0.85). Panel-reactive antibodies class I and class II were repeated on 2 occasions, with results of 2% and 21%, respectively, without donor-specific antibodies.
Starting on POD 34, the patient’s urine output started improving, ranging from 500 to 1000 cc per day. Hemodialysis was less frequently required (1–2 times/week), but his creatinine level continued to rise between them.
On POD 36, another biopsy was obtained, which showed moderate acute tubular injury, improved since the previous result. There was a single ischemic glomerulus, without signs of acute antibody or cellular mediated rejection. At this point, the patient was on anti-thymocyte globulin and mycopheno-late mofetil with a CD 3 level of 17.
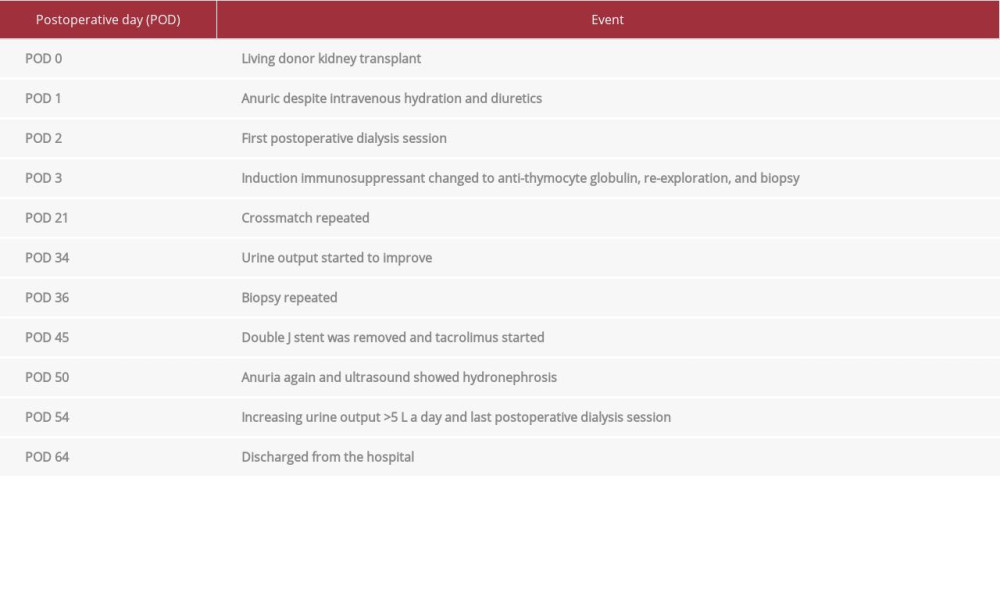
Thirteen days later, (POD 50), he developed anuria again. Ultrasound showed hydronephrosis of the graft, without obvious obstructive cause, which promptly resolved after urinary catheter insertion. Diuretics were started, but an additional dialysis session was required on POD 54. The patient’s urine output increased to >5 L per day, and the diuretics were stopped on POD 56. A follow-up ultrasound was done, which confirmed complete resolution of the hydronephrosis. The urinary catheter was removed, and the urine output remained high until his discharge on POD 64. His creatinine level gradually decreased in that period, from 386 to 159 mcmol/L. The patient continued to follow up with our outpatient clinic. On his most recent follow-up in the clinic, a year after the transplant, his creatinine level was 112 mcmol/L. Table 1 summarizes his course.
Discussion
DGF is the failure of the transplanted kidney to work in the early postoperative period [4]. Although several definitions of DGF exist, the one most widely used is the need for dialysis in the first week after transplantation [5]. This is commonly accompanied by a decline in urine output and an increase in serum creatinine level. Confusion can arise in cases that require dialysis, despite a well-functioning graft, making the diagnosis of DGF based on the above criteria inaccurate [4,6–9].
It is important to rule out conditions, such as antibody-mediated rejection, cortical necrosis/infarction, endothelial damage, acute calcineurin inhibitor toxicity, thrombotic microangiopathy, drug-induced interstitial nephritis, and recurrence of primary disease or primary non-function, as they have a similar presentation, but different management [10,11].
In our patient, DGF was diagnosed based on an abrupt decline in urine output and need of dialysis on the second postoperative day. The aforementioned conditions were ruled out histologically on 2 occasions.
DGF is more frequently diagnosed in deceased donor renal transplantation, with an incidence ranging from 23% to 50% [12–14], compared with 1.6% to 18.3% in LDKT. This is usually attributed to the decreased ischemic injury during the more controlled living donor nephrectomy [1,2,15,16], particularly in countries where LDKT is performed more commonly than DDKT (83% vs 17%) [17]. The reported incidence of DGF in a single-center study was 3.9% and 15.5% for LDKT and DDKT, respectively [18].
The 2 most consistent contributors of DGF are older donor age (45±10.6 years) and longer cold ischemia time (>20 h) [19]. None of these risk factors were present in our case, as donor age was 30 years and cold ischemia time was 92 min.
Nogueira et al reported multiple factors associated with DGF after laparoscopic donor nephrectomy, including higher numbers of HLA mismatch, longer warm ischemia time during organ procurement, and a non-related donor [20]. Higher donor body mass index (>27) and right donor nephrectomy [21] have also been associated with higher rates of DGF, but did not apply to our donor-recipient pair since the donor was the son, had only 1 HLA antigen mismatch and the WIT was only 1 min 45 s.
Hypertension in the recipient and a previous kidney transplant, on the other hand, do not appear to increase the risk of DGF [20]. Similarly, tacrolimus was not started until POD 45 and therefore could not be responsible for the graft dysfunction. Rejection and other microangiopathic conditions were ruled out on 2 occasions with renal biopsy, as was ureteric obstruction, with the help of ultrasound.
DGF usually resolves spontaneously within a few days to weeks [22]; however, extreme cases with a prolonged course have been described. The longest case included a graft that remained inert for 5 months [23]; however, unlike our patient, who had complete anuria until POD 34, this graft produced 170 mL per day of urine at POD 2 and incrementally increased to 1000 mL per day.
This case report had several limitations, including inability to generalize, difficulty to establish a cause-effect relationship, risk of overinterpretation, publication bias, and a retrospective design. Indeed, the reason leading to the recipient’s prolonged acute tubular necrosis was never disclosed, despite extensive diagnostics. This is a common clinical situation, however, and supports our argument for continuing expectant management of these patients even if the exact cause of the complication has not been disclosed. It is crucial, though, that other treatable conditions, such as rejection, ischemia, and nephrotoxic medication adverse effects, have been ruled out. If that is the case, the graft has a very good chance of full recovery.
Conclusions
DGF is a rare complication of LDKT and prolonged courses are even more uncommon. Although our patient did not have the longest recovery described in the literature, he had the longest anuric phase. Despite that, he was able to make a full recovery and achieve normal levels of creatinine. We therefore recommend expectant management in such patients, as renal function is likely to recover provided that no other ischemic or immunological factors are present.
References:
1.. Sharma AK, Tolani SL, Rathi GL, Evaluation of factors causing delayed graft function in live related donor renal transplantation: Saudi J Kidney Dis Transpl, 2010; 21(2); 242-45
2.. Park HS, Hong YA, Kim HG, Delayed graft function in living-donor renal transplantation: 10-year experience: Transplant Proc, 2012; 44(1); 43-46
3.. Budhiraja P, Reddy KS, Butterfield RJ, Duration of delayed graft function and its impact on graft outcomes in deceased donor kidney transplantation: BMC Nephrol, 2022; 23(1); 154
4.. Yarlagadda SG, Coca SG, Garg AX, Marked variation in the definition and diagnosis of delayed graft function: A systematic review: Nephrol Dial Transplant, 2008; 23(9); 2995-3003
5.. Mallon DH, Summers DM, Bradley JA, Pettigrew GJ, Defining delayed graft function after renal transplantation: Simplest is best: Transplantation, 2013; 96(10); 885-89
6.. Shoskes DA, Shahed AR, Kim S, Delayed graft function: Influence on outcome and strategies for prevention: Urol Clin North Am, 2001; 28(4); 721-32
7.. Peeters P, Terryn W, Vanholder R, Lameire N, Delayed graft function in renal transplantation: Curr Opin Crit Care, 2004; 10(6); 489-98
8.. Herrera J, Rodriguez-Iturbe B, Stimulation of tubular secretion of creatinine in health and in conditions associated with reduced nephron mass. Evidence for a tubular functional reserve: Nephrol Dial Transplant, 1998; 13(3); 623-29
9.. Bosch JP, Renal reserve: A functional view of glomerular filtration rate: Semin Nephrol, 1995; 15(5); 381-85
10.. Moreso F, Seron D, Gil-Vernet S, Donor age and delayed graft function as predictors of renal allograft survival in rejection-free patients: Nephrol Dial Transplant, 1999; 14(4); 930-35
11.. Avihingsanon Y, Ma N, Pavlakis M, On the intraoperative molecular status of renal allografts after vascular reperfusion and clinical outcomes: J Am Soc Nephrol, 2005; 16(6); 1542-48
12.. Yarlagadda SG, Coca SG, Formica RN, Association between delayed graft function and allograft and patient survival: A systematic review and meta-analysis: Nephrol Dial Transplant, 2009; 24(3); 1039-47
13.. Tapiawala SN, Tinckam KJ, Cardella CJ, Delayed graft function and the risk for death with a functioning graft: J Am Soc Nephrol, 2010; 21(1); 153-61
14.. Arora D, Hooda A, Jairam A, SP747: Delayed graft function in live related renal transplant: Nephrol Dial Transplant, 2017; 32(Suppl. 3); iii395
15.. Senel FM, Karakayali H, Moray G, Haberal M, Delayed graft function: Predictive factors and impact on outcome in living-related kidney transplantations: Ren Fail, 1998; 20(4); 589-95
16.. Kwon OJ, Ha MK, Kwak JY, Lee HW, The impact of delayed graft function on graft survival in living donor kidney transplantation: Transplant Proc, 2003; 35(1); 92-93
17.. Ghods AJ, Current status of organ transplant in Islamic countries: Exp Clin Transplant, 2015; 13(Suppl. 1); 13-17
18.. Almisfer AK, Qasim SS, Alqahtani MA, Incidence rate and predictors of delayed graft function among adult kidney transplant recipients at a tertiary care hospital in Riyadh, Saudi Arabia: Cureus, 2021; 13(5); e14985
19.. Sáinz MM, Toro JC, Poblete HB, Incidence and factors associated with delayed graft function in renal transplantation at Carlos Van Buren Hospital, January 2000 to June 2008: Transplant Proc, 2009; 41(6); 2655-58
20.. Nogueira JM, Haririan A, Jacobs SC, The detrimental effect of poor early graft function after laparoscopic live donor nephrectomy on graft outcomes: Am J Transplant, 2009; 9(2); 337-47
21.. Damodaran S, Bullock B, Ekwenna O, Risk factors for delayed graft function and their impact on graft outcomes in live donor kidney transplantation: Int Urol Nephrol, 2021; 53(3); 439-46
22.. Hellegering J, Visser J, Kloke HJ, Poor early graft function impairs long-term outcome in living donor kidney transplantation: World J Urol, 2013; 31(4); 901-6
23.. Schulz T, Pries A, Kapischke M, Delayed graft function 5 months after living donor kidney transplantation: Am J Case Rep, 2016; 17; 120-23
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250