16 July 2022: Articles 
Endoscopic Mucosal Incision to Remove a Fish Bone Completely Embedded Under the Esophageal Mucosa: A Case Report and Literature Review
Unusual clinical course
Yudai Koito1E*, Takeharu Asano1F, Satohiro MatsumotoDOI: 10.12659/AJCR.936773
Am J Case Rep 2022; 23:e936773
Abstract
BACKGROUND: Esophageal foreign bodies are known to cause esophageal perforation, penetration, and mediastinitis if left untreated. Therefore, it is desirable to remove them immediately upon being diagnosed. While endoscopic removal is the first choice for removing esophageal foreign bodies, surgical procedures are required when endoscopic removal is not possible due to the shape of the foreign bodies, or if they are completely embedded within or outside the esophageal wall.
CASE REPORT: An 83-year-old woman experienced pain in her throat after eating grilled fish. She visited our hospital the following day. Computed tomography (CT) confirmed a linear foreign body had likely become completely embedded inside the cervical esophageal wall. Upper gastrointestinal endoscopy was performed under general anesthesia, but the foreign body was not visible. Thereafter, endoscopic mucosal incision was performed and the malpositioned fish bone was finally found. We were able to remove it with gripping forceps. The procedure was completed with the mucosal incision site left open, as there was no obvious damage to the muscle layer. Postoperative CT also confirmed the full removal of the fish bone as well as the lack of any perforation. Following surgery, she underwent 2 days of fasting before re-starting meals. She was discharged uneventfully from the hospital on the seventh hospital day.
CONCLUSIONS: Even when the foreign body is not visible via endoscopy, it can still be removed by endoscopic mucosal incision based on the CT and endoscopic findings. We summarized 10 similar cases and discussed the efficacy of endoscopic removal of foreign bodies buried under the esophageal mucosa.
Keywords: Endoscopy, Digestive System, Esophageal Diseases, Foreign Bodies, Animals, Endoscopy, Gastrointestinal, esophageal mucosa, Esophageal Perforation, Female, Humans
Background
Esophageal foreign bodies, such as fish bones or dentures, are known to cause esophageal perforation, penetration, and mediastinitis if left untreated [1]. Therefore, it is desirable to remove them immediately upon being diagnosed. While endoscopic removal is the first choice for removing esophageal foreign bodies, surgical procedures are required when endoscopic removal is not possible due to the shape of the foreign bodies, or if they are completely embedded within or outside the esophageal wall [2].
With the development of esophageal endoscopic submucosal dissection (ESD) technique in recent years, it has become possible to remove esophageal foreign bodies that are completely embedded in the esophageal wall by performing endoscopic mucosal incision. We herein report on a case in which a fish bone was able to be removed by an esophageal mucosal incision despite the fish bone having become completely embedded in the esophageal wall. The removal of a foreign body buried in the esophageal wall by performing endoscopic mucosal incision has been documented by several reports. However, no report has ever summarized the efficacy of this approach. We summarize these case reports and examine the efficacy of removing an esophageal foreign body buried under the esophageal mucosa. We thus consider this report valuable.
Case Report
DEVELOPMENT AFTER HOSPITAL ADMISSION:
Regarding treatment, after consultations with surgeons, endos-copy was scheduled to be performed under general anesthesia for the following reasons: the fish bone was in the cervical esophagus; it would be difficult to treat in the event of poor sedation; it was likely that the fish bone had become completely embedded, in which case, mucosal incision would be needed; and if the fish bone could not be found by mucosal incision, transition to a surgical procedure was to be performed. Upon providing a sufficient explanation to the patient and her family and obtaining her informed consent, upper gastrointestinal (GI) endoscopy was performed under general anesthesia.
Although the fish bone was not visible in the pharynx, larynx, or cervical esophagus, erosion, redness, and edema were confirmed in the cervical esophageal mucosa (Figure 2A). In addition to the CT findings, there was also a site into which the fish bone had apparently penetrated, resulting in a diagnosis of a completely embedded fish bone under the esophageal mucosa. Subsequently, a search was conducted for the fish bone by performing endoscopic mucosal incision. Using MucoUp® (Boston Scientific Japan, Tokyo, Japan), a bulge was created in the cervical esophageal mucosa at 1 cm on the oral side from the site at which the bone was thought to have migrated, and a lateral incision of approximately 10 mm was made in the mucosa using a 1.5-mm dual knife (KD-650Q; Olympus Medical Systems, Tokyo, Japan). The submucosal layer was thick and friable and recognition of the layers was therefore more difficult than with normal endoscopic submucosal dissection, so we proceeded with dissection while paying close attention to the muscle layer. After beginning the dissection, a white moving foreign body was discovered (Figure 2B). At that point, it was gripped and pulled out with forceps (Figure 2C). The procedure was completed with the mucosal incision site left open, as there was no bleeding or obvious damage of the muscle layer. The removed fish bone was approximately 30 mm in length (Figure 2D), and the operation time was 35 min. Postoperative CT also confirmed the full removal of the fish bone as well as the lack of any perforation.
Following surgery, she underwent 2 days of fasting before restarting meals. She was discharged from the hospital on the seventh hospital day.
Discussion
Food masses, fish bones, dentures, and PTP preparations are several common sources of esophageal foreign bodies. While food masses are common in the United States and Europe, fish bones are the most frequent cause in Asia [2]. About 80–90% of foreign bodies that are ingested will be naturally excreted without complications. However, 10–20% require endoscopic removal, with 1% requiring surgical intervention [3,4]. Even after the fish bone has passed through the esophagus, the terminal ileum, ileocecum, the rectosigmoidal region, and the cecum are common sites of fish bone retention in the gastrointestinal tract due to the anatomical features. Occasionally, intestinal perforation occurs at these sites [5].
Symptoms of esophageal foreign bodies include a foreign body sensation, sore throat, pain when swallowing, dysphagia, and vomiting. When the esophageal foreign body is located at the oral side of the upper esophagus, the site of the symptoms and the position at which the foreign body is stuck tend to correspond. However, if it is at the anus side of the upper esophagus, these factors typically do not correspond [2]. Furthermore, the symptoms last for a few hours after the esophageal foreign bodies pass through the esophagus or after performing endoscopic removal. Therefore, it is best to avoid making a diagnosis based simply on the medical history and symptoms [4]. CT is useful for diagnosing fish bones as well as confirming the site, with a sensitivity of 90–100% and specificity of 93.7–100% [6–10]. However, plain X-ray often has difficulty in making an accurate identification, with a reported sensitivity of 32–39% and specificity of 72–91% [7–11].
It is recommended that esophageal foreign bodies be removed within 24 h of being diagnosed, with a delay in treatment potentially leading to an increased risk of complications. It is also recommended that sharp objects, such as denture bridges and batteries, be removed within 2–6 h of diagnosis [4]. Endoscopic removal, direct endoscopic removal, and surgical removal are performed for the removal of esophageal foreign bodies. Endoscopic removal is the first choice since it is the most minimally invasive and simple procedure. However, if endoscopic removal is difficult to perform, direct endoscopic removal or surgical removal should be performed. Since general anesthesia is mandatory for direct endoscopic removal and surgical removal, coming with a risk of complications, such as recurrent laryngeal nerve damage, empyema and mediastinal infections, endoscopic removal should be considered whenever possible [12].
In this particular case, since the pain in her throat had continued for more than 12 h and CT confirmed a fish bone within the esophageal wall in the cervical region, we diagnosed her as having a fish bone completely embedded in the esophageal wall. The fish bone may have become completely embedded because the patient swallowed white rice without chewing after the bone had already penetrated the esophageal wall. In Japan, there is a custom of swallowing white rice without chewing as a folk remedy when fish bones get stuck in the pharynx or esophagus. However, the custom is not medically recommended, as it carries a risk of causing embedment, esophageal ulcer, or abscess, as in some case reports [13,14]
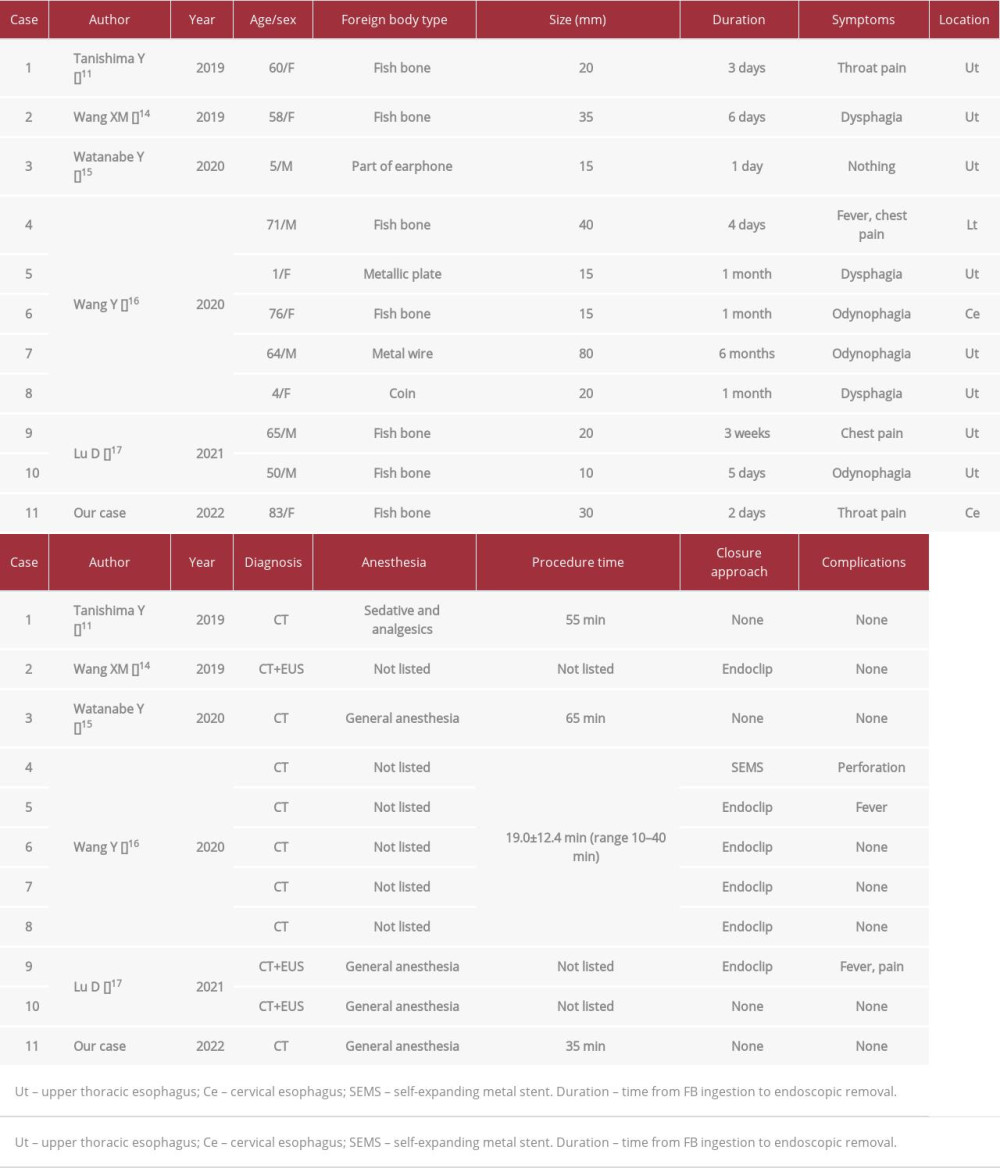
Since 2019, 10 cases have been reported of endoscopic mucosal incision to remove a foreign body that had become completely embedded under the esophageal mucosa [12,15–18]. We summarized 11 cases, including our case, in Table 1. Since esophageal foreign bodies can cause perforations, penetration, or mediastinal abscess if left untreated, it is desirable to remove them immediately after making a diagnosis. However, only 6 cases were treated within 1 week after the symptoms appeared, while the remaining 5 cases were treated after symptoms had lasted more than 3 weeks. The longest period was 6 months before being treated. The longer the treatment interval, the more likely it is that removal will be difficult, as the mucosa and submucosa will be continuously inflamed and finally replaced with granulation tissue due to the foreign body reaction [19]. All cases were diagnosed as esophageal foreign bodies by the CT findings, with penetrated and embedded sites confirmed by endoscopic findings in some cases. Foreign bodies were found relatively easily by mucosal incision. However, in Case 2, the fish bone moved under the mucous membrane to approximately 7 cm on the anus side from the site of penetration. Attention is required since a foreign body may not necessarily be embedded near the site of penetration. In Cases 2, 9, and 10, the positions of foreign bodies were confirmed by endoscopic ultrasonography (EUS) prior to mucosal incision, which is effective in determining the position at which to start the mucosal incision. Since the site was in the cervical esophagus in this case, EUS prior to mucosal incision was not carried out. However, considering that the incision was made under general anesthesia, we could have considered performing EUS. Regarding the method of anesthesia, procedures were carried out under general anesthesia in 4 cases to make it easy to treat and handle unexpected complications during the treatment. In 1 case, the procedure was carried out under sedatives and painkillers. There was no description regarding the method of anesthesia in 6 cases. In all cases, the incision was started slightly from the oral side of the foreign body’s puncture site. This is because the puncture site is edematous or fibrotic, and if the incision is started at the puncture site, it may be difficult to approach the submucosal layer. In all cases, the puncture site was identified. When the puncture site cannot be identified, EUS is helpful, and MucoUp® or glycerin is injected into the oral-most side of the foreign body using an EUS scope to facilitate determination of the incision starting site. Regarding wound closure following the removal of foreign bodies, closure with endoclips was performed in many cases and wound closure may be recommended. In our case, the esophageal breakage was located in the cervical esophagus, its size was small, and there was no obvious damage to the muscle layer upon making a mucosal incision.
We then did not perform wound closure, resulting in a good clinical course. Regarding complications, there was only 1 case of perforation due to the treatment and 2 cases of postoperative fever, with no cases resulting in stenosis or additional surgery. In Case 4, a SEMS was inserted because perforation was grossly evident. In the other cases, postoperative CT was not performed, so it was not possible to prove the presence of perforation, but intraoperative and postoperative findings indicated that there was no perforation. Postoperative antibiotics were used in Cases 2, 5, and 9 but not in the other cases. If a postoperative fever or an elevated white blood cell count or C-reactive protein level occurs, antibiotics should be used to prevent mediastinitis.
This method is considered to be an effective treatment for cases of esophageal foreign bodies that had become completely embedded. However, it does not apply to cases in which it is clear that a completely embedded foreign body has damaged the muscle layer, those in which a foreign body perforates outside the esophageal wall, and those in which the aorta or trachea are damaged; these can be diagnosed with preoperative CT. In addition, we need to keep in mind the possibility that foreign bodies may not be discovered even if a mucosal incision is performed. Moreover, it is desirable that this treatment be performed by an endoscopist who is familiar with ESD procedures under an adequate medical system.
Conclusions
Since esophageal foreign bodies can cause perforation, penetration, or mediastinitis if left untreated, it is desirable to remove them immediately upon being diagnosed. There is a possibility that foreign bodies that have become completely malpositioned in the esophageal wall can be removed by endoscopic mucosal incision. Endoscopic removal should be performed under a system in which an accurate localized diagnosis with CT and EUS is possible and transition to a surgical procedure can be easily made.
Figures
References:
1.. Eisen GM, Baron TH, Dominitz JA, Guideline for the management of ingested foreign bodies: Gastrointest Endosc, 2002; 55; 802-6
2.. Kim HU, Oroesophageal fish bone foreign body: Clin Endosc, 2016; 49; 318-26
3.. Dray X, Cattan P, Foreign bodies and caustic lesions: Best Pract Res Clin Gastroenterol, 2013; 27; 679-89
4.. Birk M, Bauerfeind P, Deprez PH, Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline: Endoscopy, 2016; 48; 489-96
5.. Dung LT, Duc NM, My TT, Cecum perforation due to a fish bone: Oxf Med Case Reports, 2021; 5; 174-76
6.. Luk WH, Fan WC, Chan RY, Foreign body ingestion: Comparison of diagnostic accuracy of computed tomography versus endoscopy: J Laryngol Otol, 2009; 123; 535-40
7.. Lue AJ, Fang WD, Manolidis S, Use of plain radiography and computed tomography to identify FB foreign bodies: Otolaryngol Head Neck Surg, 2000; 123; 435-38
8.. Liew CJ, Poh AC, Tan TY, Finding nemo: Imaging findings, pitfalls, and complications of ingested fish bones in the alimentary canal: Emerg Radiol, 2013; 20; 311-22
9.. Watanabe K, Kikuchi T, Katori Y, The usefulness of computed tomography in the diagnosis of impacted FBs in the esophagus: J Laryngol Otol, 1998; 112; 360-64
10.. Eliashar R, Dano I, Dangoor E, Computed tomography diagnosis of esophageal bone impaction: A prospective study: Ann Otol Rhinol Laryngol, 1999; 108; 708-10
11.. Ngan JH, Fok PJ, Lai EC, A prospective study on fish bone ingestion: Experience of 358 patients. Ann Surg, 1990; 211; 459-62
12.. Tanishima Y, Haruka K, Nakayoshi T, [Endoscopic removal of a fish bone that had become lodged in the esophageal submucosa by endoscopic mucosal incision.]: Gastroenterological Endoscopy, 2019; 61(2); 151-55 [in Japanese]
13.. Nakaji K, Nakae Y, Suzumura S, [Esophageal ulcer caused by accidentally swallowing a fish bone with rice.]: The Journal of the Wakayama Medical Society, 2008; 59(3); 116-18 [in Japanese]
14.. Sakata Masayuki, Harada Shotaro, Nagai Miki, [A case of deep neck abscess following a folk remedy for fish bone migration.]: The Journal of Japan Society for Infection and Aerosol in Otorhinolaryngology, 2017; 5(2); 106-9 [in Japanese]
15.. Wang XM, Yu S, Chen X, Successful endoscopic extraction of a proximal esophageal foreign body following accurate localization using endoscopic ultrasound: A case report: World J Clin Cases, 2019; 7(10); 1230-33
16.. Watanabe Y, Ukiyama E, Abe N, Takeuchi H, Ohki A, Extraction of buried and covered foreign body in esophagus using endoscopic submucosal dissection devices: Pediatr Int, 2020; 62(3); 401-2
17.. Wang Y, Liu Z-Q, Xu X-Y, Endoscopic removal of entirely embedded esophagus-penetrating foreign bodies (with video): J Gastroenterol Hepatol, 2021; 36(7); 1899-904
18.. Lu D, Lv L, Gu Q, Extraction of fish bones embedded in the esophagus via endoscopic submucosal dissection: Two case reports and literature review: Front Med (Lausanne), 2021; 8; 746720
19.. Kikuchi K, Tsurumaru D, Hiraka K, Unusual presentation of an esophageal foreign body granuloma caused by a fish bone: Usefulness of multi-detector computed tomography: Jpn J Radiol, 2011; 29; 63-66
Figures
In Press
04 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943514
04 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.941835
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943042
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942578
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250