09 August 2022: Articles 
Septic Shock Induced by Acute Pyelonephritis Resulting from Kidney Stones Treated by Double-J Ureteral Stents in a Pregnant Woman: A Case Report and Literature Review
Unusual clinical course, Challenging differential diagnosis, Unusual or unexpected effect of treatment, Educational Purpose (only if useful for a systematic review or synthesis)
Man ZhangDOI: 10.12659/AJCR.936967
Am J Case Rep 2022; 23:e936967
Abstract
BACKGROUND: Bacteriuria occurs in many pregnant women which may result in symptomatic urinary tract infection (UTI), including acute pyelonephritis (APN), which can lead to septic shock. However, there was no standard protocol of managing pregnant women with APN about the regimen, timing, length of antibiotic appliance as well as the indication of implanting double-J ureteral stents in those with kidney stones.
CASE REPORT: A 26-year-old pregnant woman (G1P0, 27 weeks plus 3 days) presented to our hospital on account of fever and pain in the flanks and was admitted on account of suspected UTI due to bacteriuria and elevated inflammatory markers. Elevated WBC count of 18.26×10⁹/L, PCT of 2.75, CRP of 198 mg/L, existence of kidney stones, renal and perirenal inflammation were observed. Cefoperazone sodium sulbactam sodium was given. The patient experienced septic shock on day 2 with a low blood pressure of 81/52 mmHg. Double-J ureteral stents were implanted due to upper urinary tract obstruction on day 3 with continuous use of meropenem based on urine culture and antibiotic sensitivity results. From day 7, the antibiotics were changed to cefoperazone-sulbactam. The patient’s laboratory results (biochemistry, PCT, and CRP) all gradually went to normal, and she was discharged on day 15.
CONCLUSIONS: We learned that urine culture and antibiotic sensitivity examination were suggested after bacteriuria was observed in pregnant women to guide further treatment. Once APN was suspected, antibiotic therapy should be commenced and early-stage drainage by double-J ureteral stents could be considered if warranted in appropriate patients.
Keywords: Anti-Bacterial Agents, Bacteriuria, Pyelonephritis, Sepsis, Stents, Adult, Female, Humans, Kidney Calculi, Pregnancy, Pregnant Women, Shock, Septic
Background
The majority of non-obstetric antepartum hospitalization during pregnancy resulted from urinary tract infection (UTI), including acute cystitis (AC), acute pyelonephritis (APN), etc [1]. Particularly, AC and APN have a higher prevalence in pregnant women than in the general population [2]. Some of the pregnant women with UTI have no obvious manifestations while others may have polyuria, frequent urination, painful micturition, suprapubic pain, etc. Among all symptoms and clinical signs, asymptomatic bacteriuria (ASB) had a higher prevalence rate of 2–7% in pregnant women, the diagnosis of which was based on laboratory test of urine bacteria (presence of ≥105 bacteria per millimeter of urine).
Differential diagnosis between APN and lower urinary tract infection is crucial in pregnant women with bacteriuria, since previous reports have acknowledged more severe maternal and fetal morbidity and mortality, as well as prepartum birth and low birth wight (LBW) in APN [3]. In addition, complications like anemia, acute hypoxic respiratory failure, acute kidney injury, and septicemia are also more common in pregnant women with APN. However, most pregnant women with tendency to develop APN are not likely to manifest obvious symptoms in the early stage but can have a devastating condition once the symptoms occur [4]. As a result, looking for more reliable and precise early-stage indicators is of paramount importance in reducing severity and maternal as well as fetal mortality. Recently, procalcitonin (PCT), the existence of leukocytosis, thrombocytosis, etc have been regarded as emerging prognostic predictors, although the exact accuracy and prognostic value have not been fully elucidated [5].
A small fraction of pregnant women with APN who are not able to get recognized during early stage can develop sepsis manifested by high fever, decreased blood pressure, impairment of consciousness, etc, which is a life-threatening condition often needing decisive delivery. Septic shock is one of the 4 main causes of obstetric adverse events, which include septic shock, abortion, hemorrhage, and hypertensive disorders [6]. However, the standard treating protocol has not been clearly elucidated. APN-related sepsis maintains the characteristics of insidious onset, rapid development, complexity of pathogen, difficulty of choosing appropriate antibiotics, and high mortality. The pathogenesis leading to APN varies, including pathogen uplink infection, renal calculi, congenital anatomical abnormalities, which make the treatment even more complicated [7]. Meanwhile, the types of pathogens may vary, especially in severe cases like those with sepsis, including
Meanwhile, in pregnant women of APN with concomitant upper urinary tract obstruction by kidney stones, the indication and timing of implanting double-J ureteral stents to promote drainage have not been fully recognized. Therefore, discussing the whole-length management of APN-related septic shock, including the choice of antibiotics, necessity of double-J ureteral stents implantation in patients with kidney stones is mandatory in treating septic shock resulting from APN and kidney stones during pregnancy.
Hereby, we present a patient who had APN-related septic shock with kidney stones during pregnancy and received double-J ureteral stents implantation plus combined antibiotic therapy and eventually recovered without urgent delivery.
Case Report
A 26-year-old pregnant woman (G1P0, 27 weeks plus 3 days) was admitted to our hospital due to fever, slight pain of the lumbar region, micturition pain, frequent micturition, urgent urination for 30 days. Before admission to our hospital, she was treated at a county hospital where bacteriuria was diagnosed. The detailed therapeutics was unclear except that she had taken cephalosporin orally for 8 days. She claimed that the symptoms were not obviously relieved after such treatment. Physical examination indicated high fever of 39.5°C, pan-abdominal pain (tenderness and rebound tenderness), pain in the renal region, swelling of both the low extremities. Vaginal bleeding and exudate were not observed. Blood routine examination on day 1 showed high WBC count, particularly neutrophils, and severe anemia. The detailed values of the blood routine examination were shown in Table 1. Biochemical examination on day 1 showed an elevation of total bilirubin (TBIL), direct bilirubin (DBIL) and low albumin level. The patient did not have acute fatty liver of pregnancy. The detailed values of biochemical examination were shown in Table 2. C-reactive protein (CRP) was 198 mg/L, PCT was 3.65, erythrocyte sedimentation rate (ESR) was 153 mm/h. Urine routine examination showed the existence of WBC (3+). Coagulation routine examination results were shown in Table 3. Abdominal magnetic resonance imaging (MRI) (Figure 1) showed that the kidneys were slightly enlarged with abnormal signals in both kidneys and perirenal cavity along with thickening of renal fascia. Abdominal MRI also showed expansion of renal pelvis and the upper segment of ureters and the possibility of kidney or peri-renal abscess. In addition, peritonitis was also considered since there was signal enhancement of the major omentum and related fat space. Abdominal ultrasound (Figure 2) on admission showed several small stones in the renal calices (the biggest one of 0.8×0.9 cm). Abdominal ultrasound also revealed hydro-nephrosis. Intravenous cefoperazone sodium sulbactam sodium was arranged every 8 hours to combat infection. Human serum albumin was used to supplement protein. Blood trans-fusion was prescribed to relieve anemia. To reduce the risk of resistant bacteria or even multiple-resistance bacteria, we arranged urine culture and antibiotic sensitivity examinations.
However, on the morning of day 2, the patient manifested impaired consciousness and could not express herself clearly. Her blood pressure dropped to 81/52 mmHg and heart rate was 87 per minute. Considering the blood pressure, overall state, and laboratory tests results, septic shock was diagnosed. She had a regular and normal heart rhythm and auscultations of the heart valves were normal. Immediate fluid infusion and symptomatic treatment were done along with deep vein catheterization to monitor central venous pressure (CVP). Antibiotics were changed to meropenem (1.0g ivgtt q8h). To prevent other unpredictable risks, the patient was transferred to ICU department for further treatment. Her blood pressure has not elevated to normal despite the fluid transfusion and antibiotic treatment. Given that the infection was not easily relieved by conventional antibiotics due to kidney stones and the fact that the patient had upper urinary tract obstruction shown by hydronephrosis, we decided to implant double-J ureteral stents to promote drainage in order to relieve inflammation. During the procedure, we found erythema and hyperemia at the tri-gone of bladder. Flow of urine from the ureteral orifices was observed. After the implantation of double-J ureteral stents, we observed outflow of turbid urine with white floccule. Urine culture result came out and showed the main type of bacteria was
Discussion
UTI in pregnant women is a unique and complicated situation, which is responsible for adverse maternal and fetal events, like preterm birth, septicemia, respiratory failure, etc. The patients may present with asymptomatic bacteriuria if the bacteria are restricted in the urine but may present with obvious symptoms when bacterial invasion into the renal parenchyma and urinary tract occurs, after which the patients can have either cystitis or APN [8]. Although APN can lead to severe cases of sepsis, patients in the early stage are mostly asymptomatic and the disease onset is relatively insidious. Several studies have made similar conclusions that a delay in both diagnosis and aggressive therapy could lead to acute respiratory distress syndrome which requires mechanical ventilation, higher morbidity of maternal anemia relying on blood trans-fusion and compromised renal function relying on dialysis [9]. Therefore, identification and recognition of APN during early stage is crucial and makes it possible for timely and precise intervention, including enhancing fetal lung maturity and protecting fetal brain development. Previous reports have demonstrated that remarkable change of inflammatory indicators in the maternal plasma could be of benefit for early identification, like WBC count, CRP level. Another study pointed out that CRP, ESR, WBC count, neutrophil count and ratio were efficient biomarkers to predict the existence or escalation of UTI, including cystitis and APN [10]. More importantly, PCT was believed to maintain the potential to differentially diagnose cystitis and APN [8]. A systematic review and meta-analysis found a pooled sensitivity of 0.86 and specificity of 0.74 in differentiating APN from other forms of UTI in children with the help of PCT, the effect of which was superior to CRP and EST [11]. Therefore, we thought it worthy to investigate the potential of PCT to particularly differentiate APN to facilitate early intervention in pregnant women. In addition, recognition of risk factors for APN, like kidney stones, previous history of APN or UTI, anatomical abnormality of the urinary tract was necessary.
In recent years, several studies have been carried out to investigate the most common pathogens related to APN to promote standard antibiotic medication [12]. Among these studies,
In the case we described, double-J ureteral stents implantation was also applied besides the use of combined antibiotic therapy. As is known, kidney stones are among the risk factors for APN during pregnancy and can lead to a series of other complications like hydronephrosis [15]. Since double-J ureteral stents are commonly used in patients with kidney stones without pregnancy, whether prompt appliance of double-J ureteral stents was also beneficial in pregnant women of APN with concomitant kidney stones was of heated discussion. Through our experience, early appliance of double-J ureteral stents could alleviate inflammatory activation and retard disease progression by facilitating drainage. However, a clinical study found out early appliance of double-J ureteral stents implantation did not necessarily bring benefits of reducing complications and optimizing outcomes of mothers and children while it could shorten the duration of hospital stays [16].
If not managed properly, APN can trigger septic shock manifested by hemodynamic instability, low blood pressure, and more complications. Some scholars pointed out that presepsin (PSEP) and PCT were independent predictors of septic shock following APN with concomitant kidney stones [17]. Meanwhile, a study pointed out that application of quick Sequential Organ
Failure Assessment (qSOFA) had good accuracy in predicting ICU admission and in-hospital mortality. Particularly, having a qSOFA score over 2 was a significant predictor for ICU admission and in-hospital mortality. Moreover, another study concluded that older age, elevated serum creatinine, presence of multiple resistant bacteria, and concomitant diabetes mellitus were independent predictors of worse outcomes [18].
Our patient had bacteriuria for 1 month and had received low-dose oral antibiotics and she did not feel improvement. Although she was given continuous intravenous antibiotic medication since admission due to APN with concomitant kidney stones, she still had septic shock onset because the overwhelming infection had been ongoing for 30 days. We thought it might be necessary to facilitate drainage and alleviate obstruction since conventional antibiotic therapy alone did not appear to be effective. Luckily, the patient’s status started to improve after implantation of double-J ureteral stents. Most importantly, ultrasonic finding of several stones in the bladder after implantation of double-J ureteral stents suggested that its implantation was of paramount significance in alleviating obstruction and removing small stones. Therefore, the combination of drainage and antibiotic therapy may be of paramount importance.
Conclusions
From this patient, we learned that attention should be paid to symptomatic or asymptomatic bacteriuria in pregnant women, in which a urine culture and antibiotic sensitivity examination were recommended. Still, risk factors for UTI and APN should be screened and several serum indicators like PCT should be tested. Combined regimens of antibiotics should be initiated promptly to prevent disease escalation, and serum indicators should be tested to predict the possibility of developing sepsis. Double-J ureteral stents implantation should be considered when APN resulting from kidney stones or other causes of obstructions is discovered, and multidisciplinary and comprehensive care should be provided in cases of septic shock.
Figures
Tables
Table 1.. Core parameters of the blood routine examination (plus CRP) on day 1 and day 8.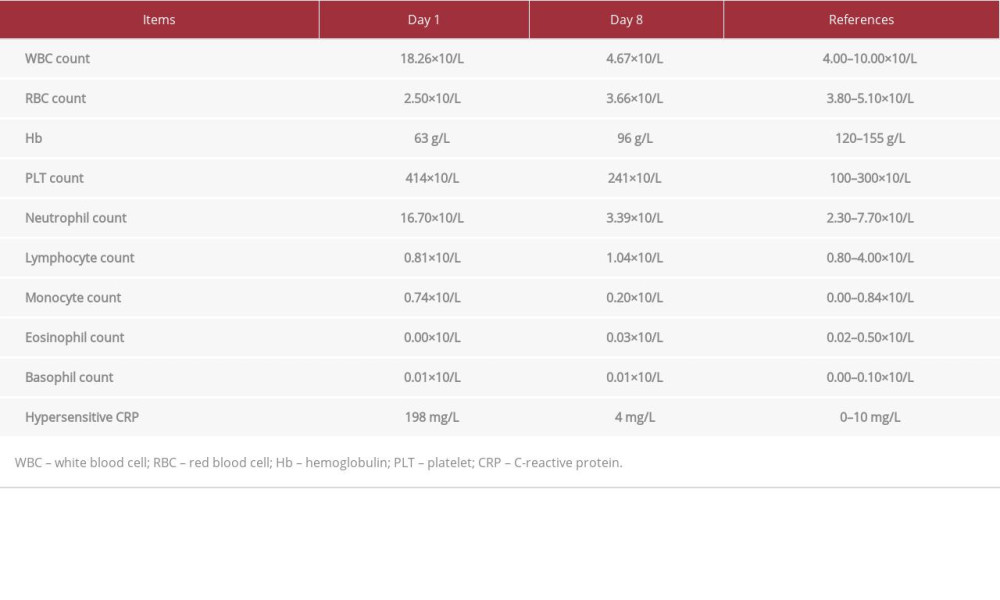 Table 2.. Core parameters of the biochemical examination on day 1 and day 8.
Table 2.. Core parameters of the biochemical examination on day 1 and day 8.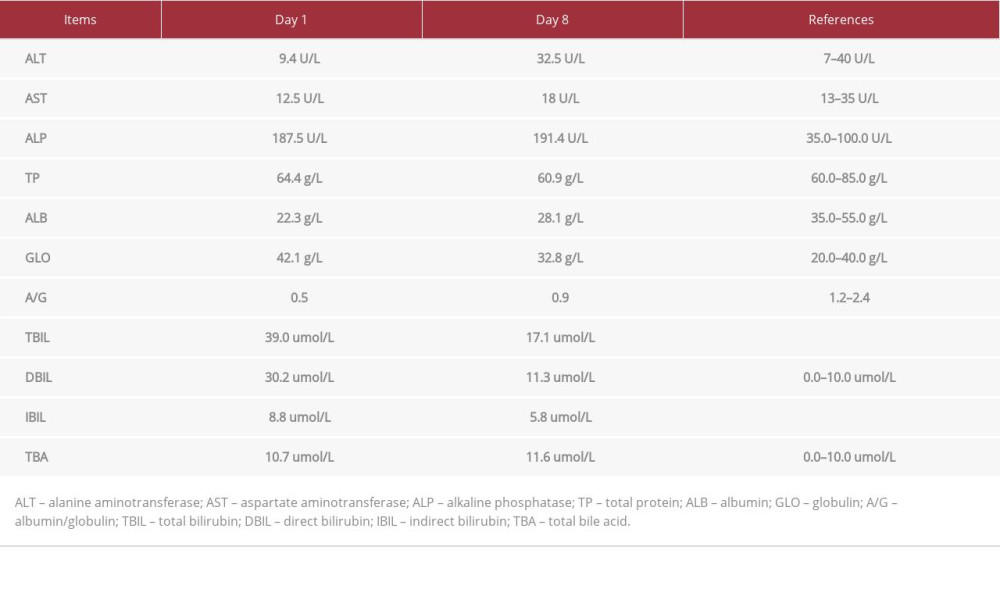 Table 3.. Core parameters of the coagulation routine examination on day 1 and day 8.
Table 3.. Core parameters of the coagulation routine examination on day 1 and day 8.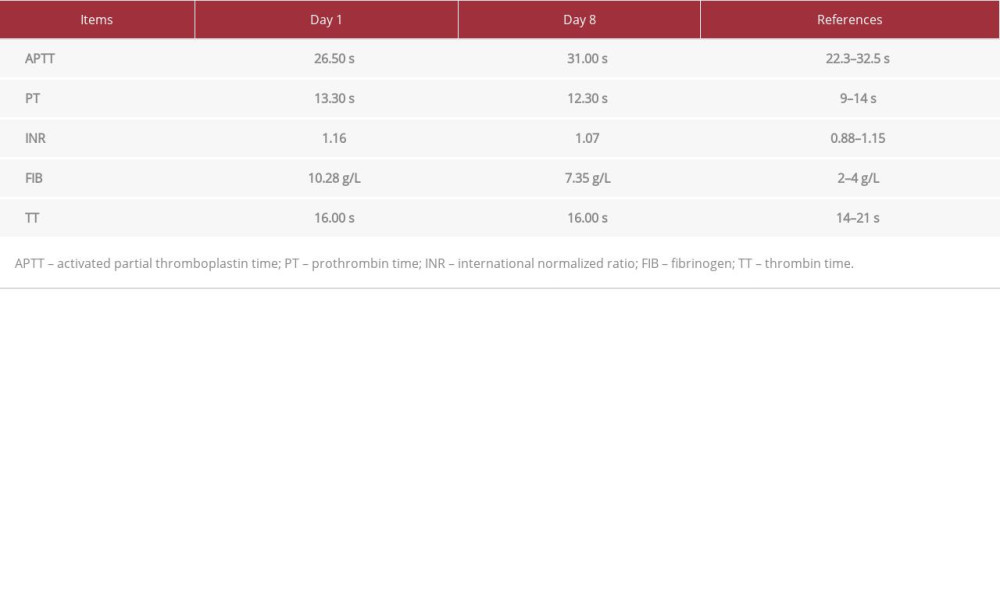 Table 4.. Antibiotic sensitivity examination.
Table 4.. Antibiotic sensitivity examination.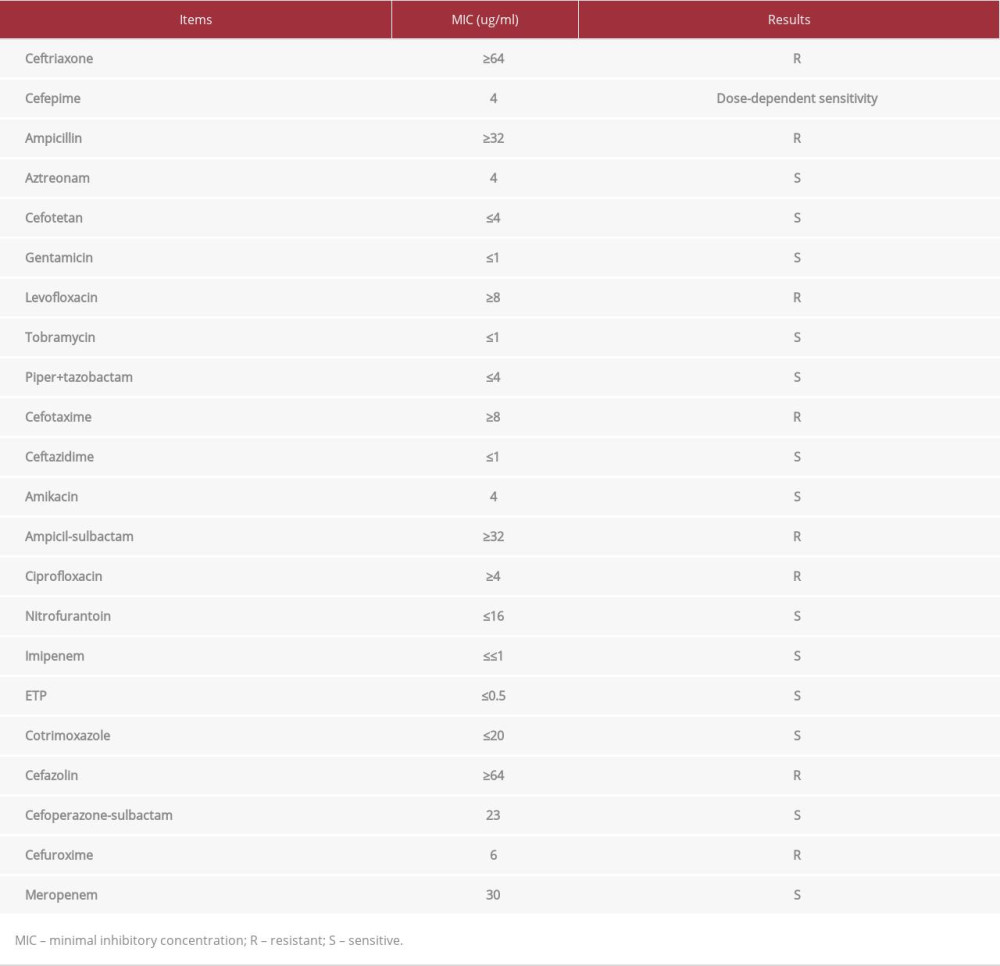
References:
1.. Balachandran L, Jacob L, Al Awadhi R, Urinary tract infection in pregnancy and its effects on maternal and perinatal outcome: A retrospective study: Cureus, 2022; 14(1); e21500
2.. Bey E, Perrouin-Verbe B, Reiss B, Outcomes of pregnancy and delivery in women with continent lower urinary tract reconstruction: Systematic review of the literature: Int Urogynecol J, 2021; 32(7); 1707-17
3.. Saffarini JH, Ahmad QT, Samara AM, Assessment of lower urinary tract symptoms during pregnancy: An observational cross-sectional study from Palestine: BMC Pregnancy Childbirth, 2021; 21(1); 84
4.. Ghouri F, Hollywood A, Antibiotic prescribing in primary care for urinary tract infections (UTIs) in pregnancy: An audit study: Med Sci (Basel), 2020; 8(3); 40
5.. Huang SY, Hsiao CH, Zhang XQ, Serum procalcitonin to differentiate acute antepartum pyelonephritis from asymptomatic bacteriuria and acute cystitis during pregnancy: A multicenter prospective observational study: Int J Gynaecol Obstet, 2022; 158(1); 64-69
6.. Khatri A, Naeger Murphy N, Wiest P: Antimicrob Agents Chemother, 2015; 59(8); 4375-78
7.. Mital R, Forster M, Alloghbi A, A case of a false-positive urine pregnancy test and delayed diagnosis of obstructive pyelonephritis: Am J Case Rep, 2020; 21; e920440
8.. Blauvelt CA, Nguyen KC, Cassidy AG, Perinatal outcomes among patients with sepsis during pregnancy: JAMA Netw Open, 2021; 4(9); e2124109
9.. Agarwal R, Goyal P, Mohta M, Comparison of sequential organ failure assessment (SOFA) and sepsis in obstetrics score (SOS) in women with pregnancy-associated sepsis with respect to critical care admission and mortality: A prospective observational study: J Obstet Gynaecol India, 2021; 71(1); 45-51
10.. Werter DE, Kazemier BM, Schneeberger C, Risk indicators for urinary tract infections in low risk pregnancy and the subsequent risk of preterm birth: Antibiotics (Basel), 2021; 10(9); 1055
11.. Whittington JR, Simmons PM, Eltahawy EA, Bladder stone in pregnancy: A case report and review of the literature: Am J Case Rep, 2018; 19; 1546-49
12.. Langermans LM, Cools W, Van Limbergen I, Optimal timing to screen for asymptomatic bacteriuria during pregnancy: first vs: second trimester. J Perinat Med, 2021; 49(5); 539-45
13.. Shaikh KJ, Osio VA, Leeflang MM, Procalcitonin, C-reactive protein, and erythrocyte sedimentation rate for the diagnosis of acute pyelonephritis in children: Cochrane Database Syst Rev, 2020; 9(9); CD009185
14.. Smaill FM, Vazquez JC, Antibiotics for asymptomatic bacteriuria in pregnancy: Cochrane Database Syst Rev, 2019; 2019(11); CD000490
15.. Perlitz Y, Saffoury E, Shabso N, Maternal and neonatal outcome of asymptomatic bacteriuria at term pregnancy: Pathog Dis, 2019; 77(5); ftz046
16.. Greve VH, Greve T, Helmig RB, Bacteriuria in pregnancy in a danish contemporary cohort of women: Infect Dis Obstet Gynecol, 2020; 2020; 8398537
17.. Koningstein FN, Schneeberger C, van der Ven AJ, Is asymptomatic bacteriuria associated with short cervical length in women with a singleton pregnancy, a secondary analysis of two national cohort studies with small embedded randomized controlled trials: Eur J Obstet Gynecol Reprod Biol, 2020; 248; 172-76
18.. Zhou Q, Chen WQ, Xie XS, Maternal and neonatal outcomes of pregnancy complicated by urolithiasis: a systematic review and meta-analysis: J Nephrol, 2021; 34(5); 1569-80
Figures
Tables
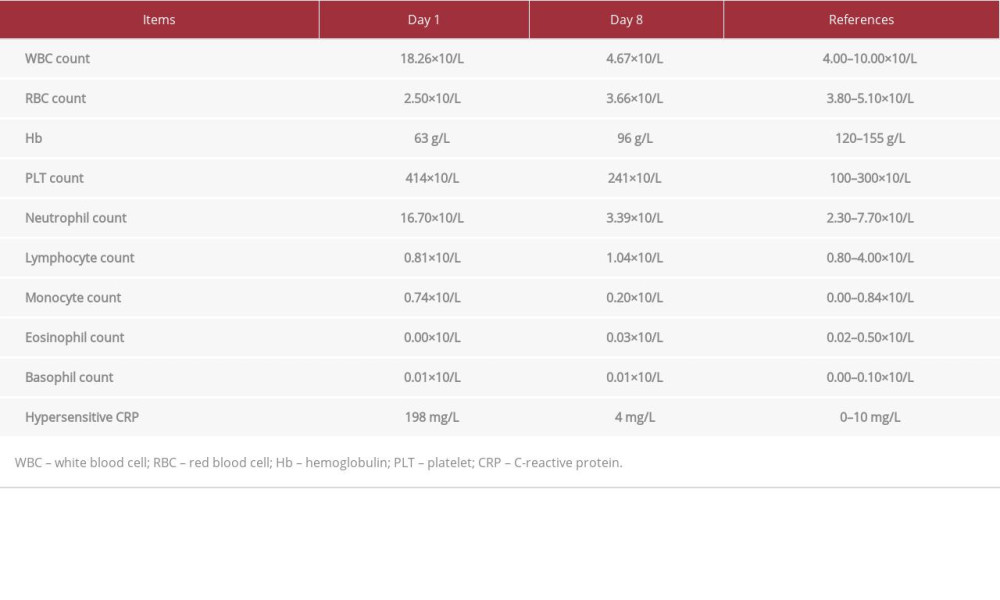 Table 1.. Core parameters of the blood routine examination (plus CRP) on day 1 and day 8.
Table 1.. Core parameters of the blood routine examination (plus CRP) on day 1 and day 8.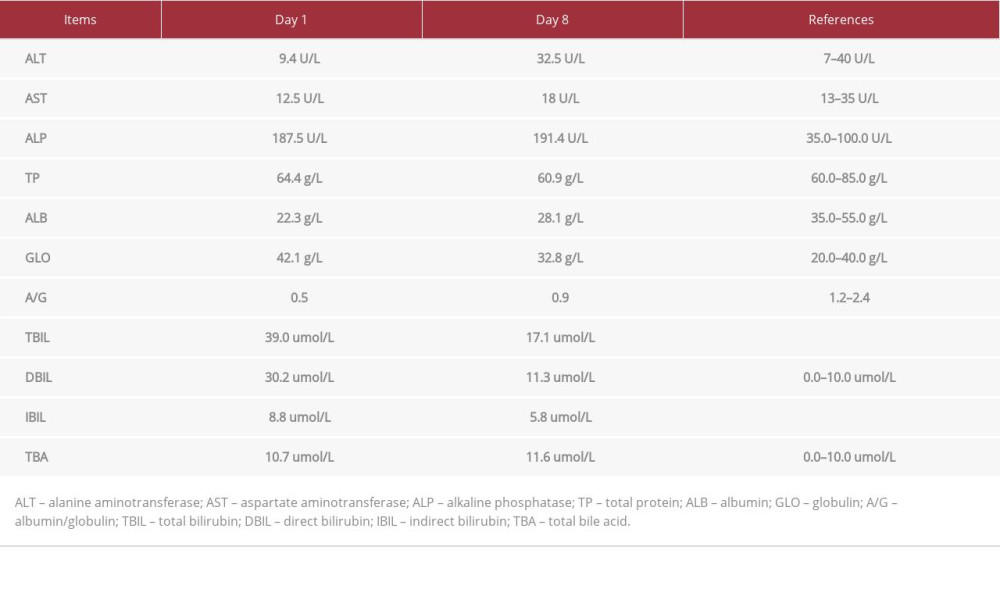 Table 2.. Core parameters of the biochemical examination on day 1 and day 8.
Table 2.. Core parameters of the biochemical examination on day 1 and day 8.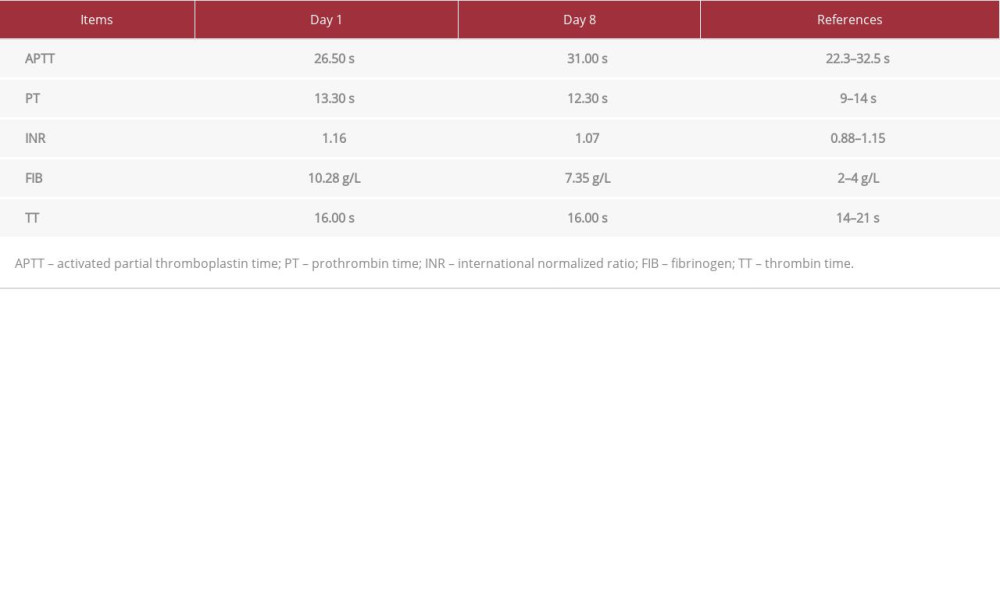 Table 3.. Core parameters of the coagulation routine examination on day 1 and day 8.
Table 3.. Core parameters of the coagulation routine examination on day 1 and day 8.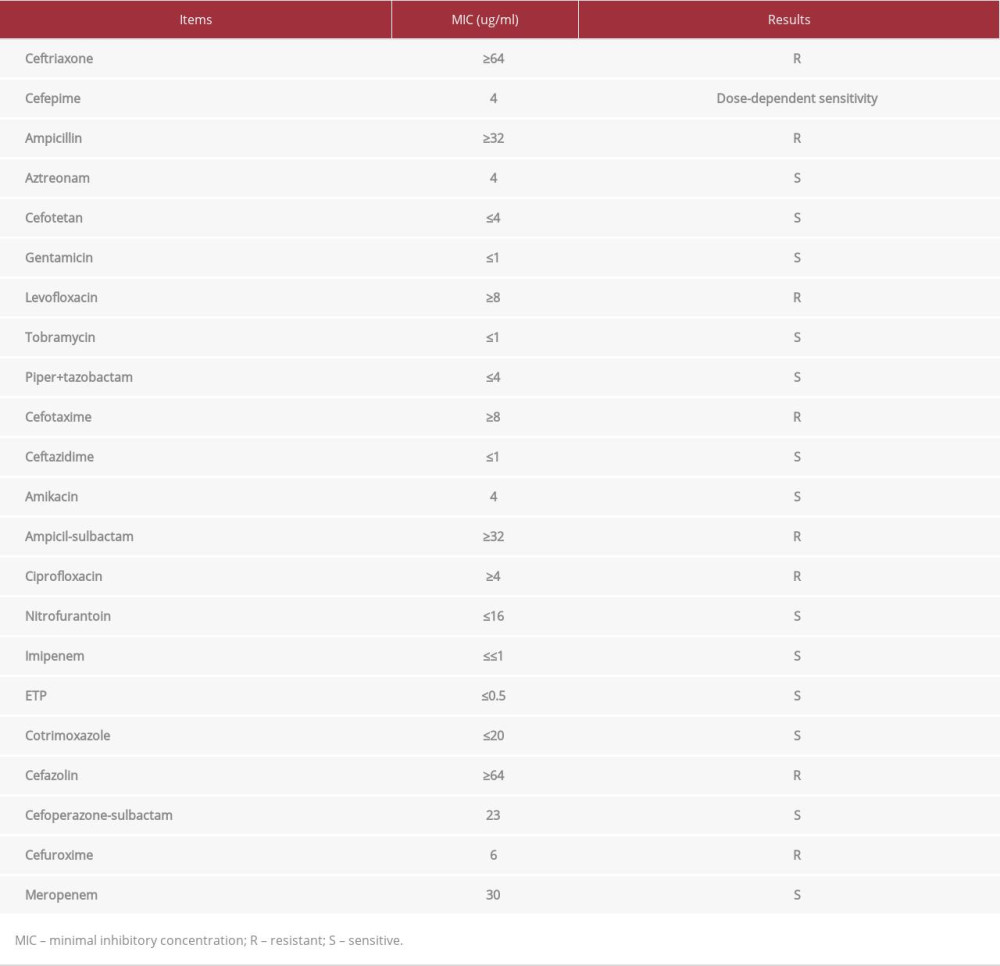 Table 4.. Antibiotic sensitivity examination.
Table 4.. Antibiotic sensitivity examination.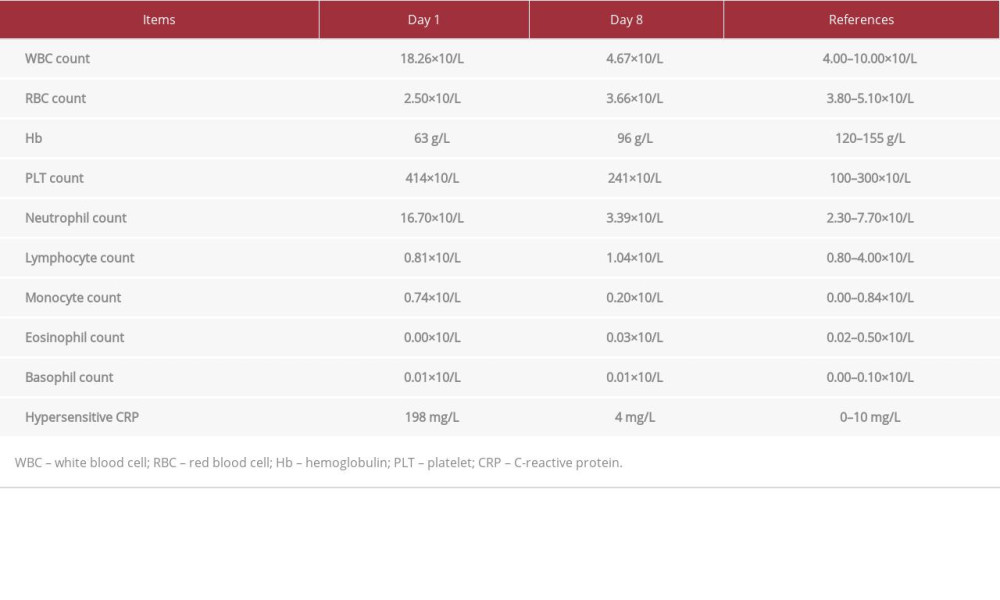 Table 1.. Core parameters of the blood routine examination (plus CRP) on day 1 and day 8.
Table 1.. Core parameters of the blood routine examination (plus CRP) on day 1 and day 8.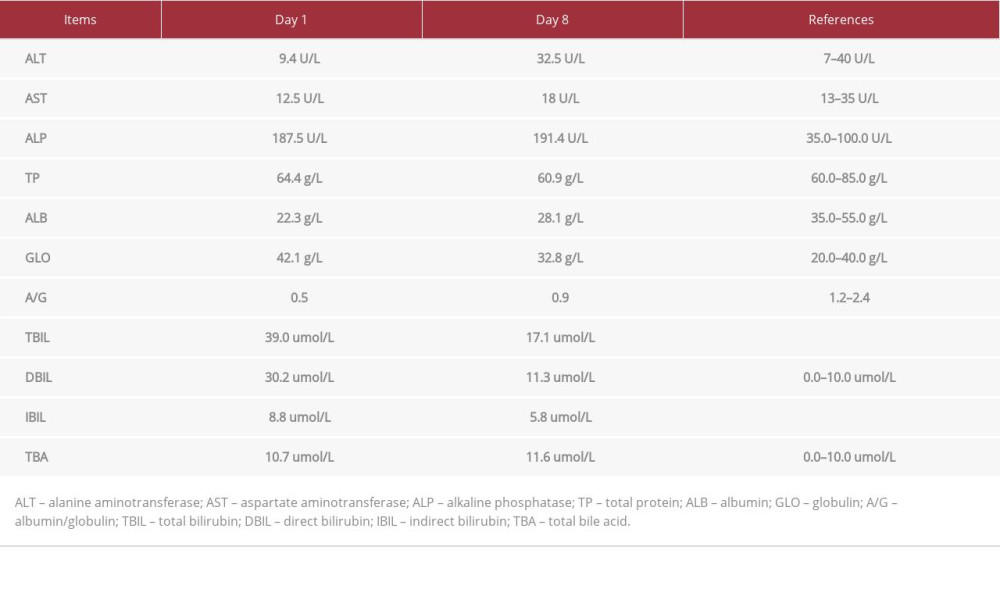 Table 2.. Core parameters of the biochemical examination on day 1 and day 8.
Table 2.. Core parameters of the biochemical examination on day 1 and day 8.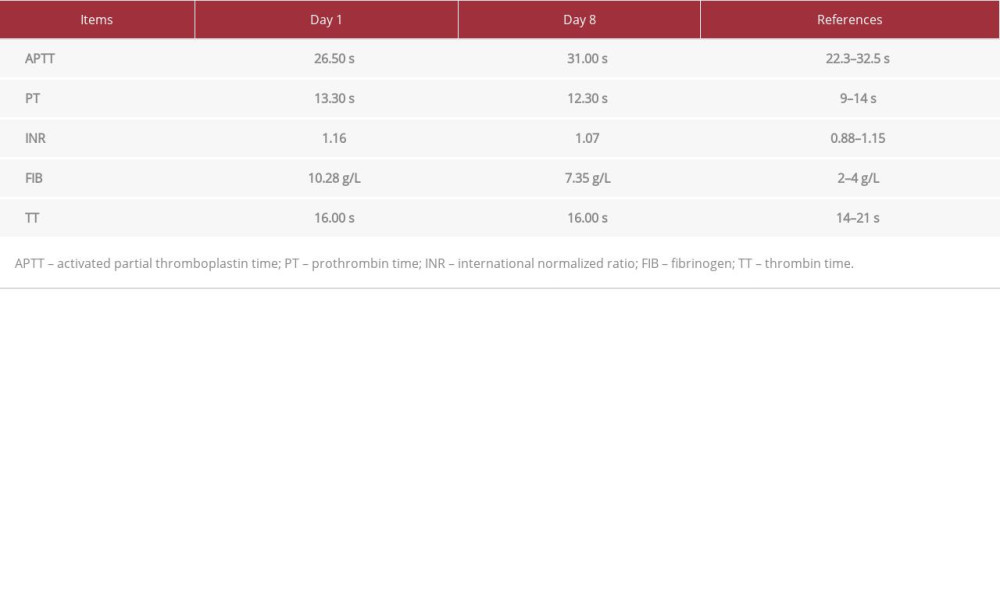 Table 3.. Core parameters of the coagulation routine examination on day 1 and day 8.
Table 3.. Core parameters of the coagulation routine examination on day 1 and day 8.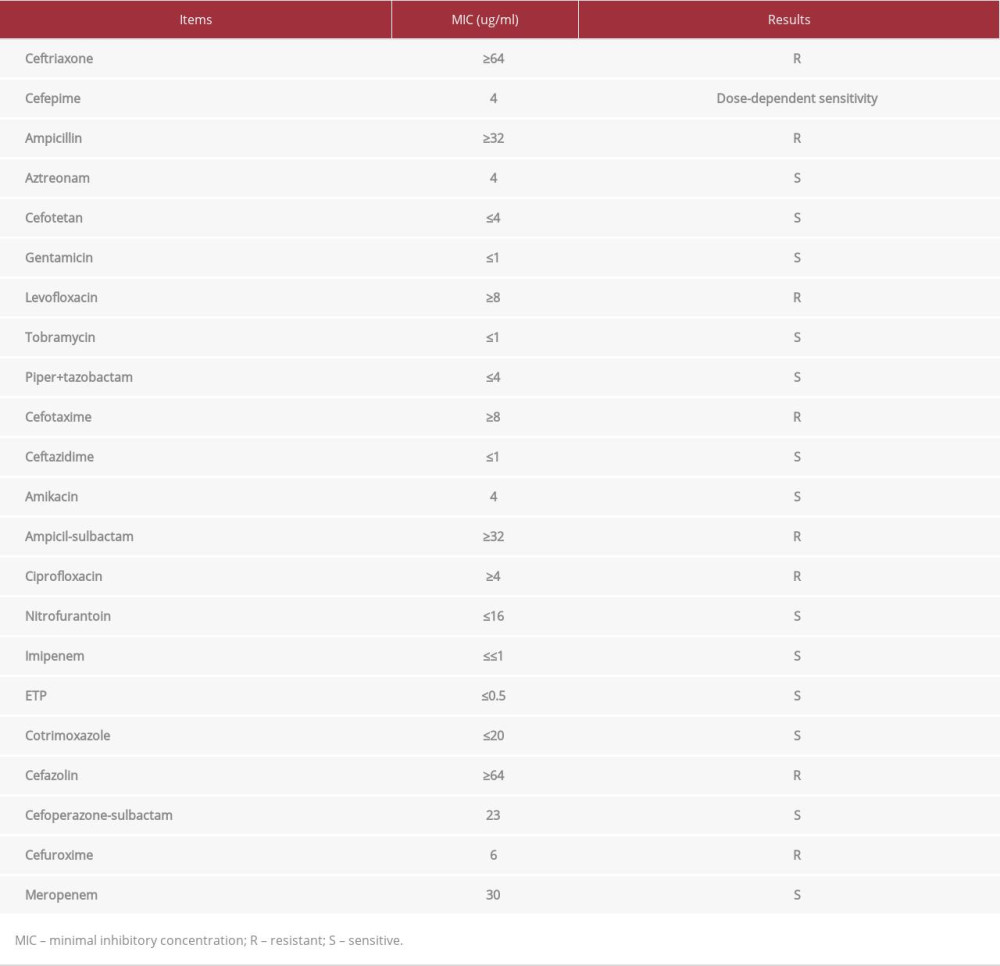 Table 4.. Antibiotic sensitivity examination.
Table 4.. Antibiotic sensitivity examination. In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








