31 October 2022: Articles 
Neck pain and Headache Complicated by Persistent Syringomyelia After Foramen Magnum Decompression for Chiari I Malformation: Improvement with Multimodal Chiropractic Therapies
Unusual or unexpected effect of treatment, Rare disease
Eric Chun-Pu ChuDOI: 10.12659/AJCR.937826
Am J Case Rep 2022; 23:e937826
Abstract
BACKGROUND: Patients with Arnold-Chiari Malformation I (CM-I) treated with foramen magnum decompression (FMD) can have ongoing neck pain, headaches, and other symptoms complicated by persistent syringomyelia, yet there is little research regarding treatment of these symptoms.
CASE REPORT: A 62-year-old woman with a history of residual syringomyelia following FMD and ventriculoperitoneal shunt for CM-I presented to a chiropractor with progressively worsening neck pain, occipital headache, upper extremity numbness and weakness, and gait abnormality, with a World Health Organization Quality of Life score (WHO-QOL) of 52%. Symptoms were improved by FMD 16 years prior, then progressively worsened, and had resisted other forms of treatment, including exercises, acupuncture, and medications. Examination by the chiropractor revealed upper extremity neurologic deficits, including grip strength. The chiropractor ordered whole spine magnetic resonance imaging, which demonstrated a persistent cervico-thoracic syrinx and findings of cervical spondylosis, and treated the patient using a multimodal approach, with gentle cervical spine mobilization, soft tissue manipulation, and core and finger muscle rehabilitative exercises. The patient responded positively, and at the 6-month follow-up her WHO-QOL score was 80%, her grip strength and forward head position had improved, and she was now able to eat using chopsticks.
CONCLUSIONS: This case highlights a patient with neck pain, headaches, and persistent syringomyelia after FMD for CM-I who improved following multimodal chiropractic and rehabilitative therapies. Given the limited, low-level evidence for these interventions in patients with persistent symptoms and syringomyelia after FMD, these therapies cannot be broadly recommended, yet could be considered on a case-by-case basis.
Keywords: Arnold-Chiari Malformation, Chiropractic, Exercise Therapy, Manipulation, Spinal, Neck Pain, Therapy, Soft Tissue, Female, Humans, Middle Aged, Syringomyelia, Foramen Magnum, Quality of Life, Decompression, Surgical, Magnetic Resonance Imaging, Headache, Treatment Outcome
Background
Arnold-Chiari malformation type I (CM-I), the most common type of Arnold-Chiari malformation, is defined as a downward descent of the cerebellar tonsils at least 5 mm inferior to the level of the foramen magnum [1]. Between 30% and 80% of patients with Arnold-Chiari malformation also have syringomyelia [2], an abnormal fluid-filled cavity within the spinal cord [3]. While symptoms of CM-I are varied, patients with syringomyelia can present with sensory symptoms, hand weakness, scoliosis, neck and back pain, and headaches [2]. While these patients often undergo foramen magnum decompression (FMD) surgery, there has been little research on treatment of neck pain and other symptoms that can persist along with syringomyelia after surgery.
About 93% of patients with a syrinx undergoing FMD have a reduction in the size of the syrinx [4]. However, among those treated surgically for arachnoid cyst with syrinx, symptoms can improve even with minimal or no change in the syrinx size [5]. Persistence of the syrinx and associated symptoms are thought to relate to ongoing impairment of cerebrospinal fluid (CSF) flow [6,7]. In those patients without improvement in CSF flow following surgery, symptoms can persist, including weakness in 100% of patients, vision symptoms in 84%, dizziness in 78%, neck pain in 66%, and headache in 50% [7].
Half of patients with persistent or recurrent syringomyelia after FMD are treated conservatively and can experience improvement 1 to 2 years following their original surgery [5]. However, the remainder of patients undergo another surgical procedure, at a mean 15 months after surgery [5]. CSF diversion is the most commonly utilized procedure among these patients and involves a syringo-subarachnoid shunt [5]. Another method of CSF diversion is ventriculoperitoneal shunting [4,5]. Revision surgery is another option which is only rarely considered, when cerebellar tonsillar herniation persists after surgery [5].
There is a limited understanding of the optimal conservative treatment options for patients with neck pain or other symptoms and persistent syringomyelia after FMD [4,8]. One article described that pain medications and rest were commonly prescribed for these patients [9]. Most research regarding manual therapies has been devoted to CM-I prior to or instead of surgical decompression, mostly in the form of case reports. These have shown a variety of responses to care, including negative [10–13], equivocal [14,15], or positive outcomes [16–22]. As of July 4, 2022, we are aware of only 2 cases which reported the use of manual therapies for a patient following FMD, both yielding a positive outcome [8,23].
The literature regarding rehabilitative and manual therapies for syringomyelia in general is also limited [24]. However, according to one survey, patients reported that physical therapy was helpful with symptom management [24]. Other case reports have noted improvement in syringomyelia-related symptoms with various conservative treatments, including cervical traction, joint mobilization, soft tissue manual therapies, posture correction, and acupuncture [25–28].
Given the limited research on treatments for neck pain, headache, and other symptoms persistent in conjunction with syringomyelia after FMD for CM-I, we present a patient who responded positively to a multimodal chiropractic treatment regimen.
Case Report
PATIENT INFORMATION:
A 62-year-old woman presented to a chiropractor in a multidisciplinary office with frequent severe neck pain and occipital headache and intermittent numbness and weakness of the bilateral upper limbs, more prominently affecting the right side. The pattern of numbness chiefly affected her right deltoid region to the lateral arm, forearm, and the hand, diffusely. The patient’s self-reported pain intensity was a 9 out of 10 on the numeric pain rating scale. She noted being unable to use chopsticks with her right hand due to numbness, weakness, and hand deformity. Her World Health Organization Quality of Life Score (WHO-QOL) was 52%.
Her medical history was significant for CM-I with FMD, persistent syringomyelia, and epilepsy. She denied having any difficulty swallowing or speaking, hoarseness, sleep apnea, and gastrointestinal or cardiovascular symptoms. She was a homemaker, nonsmoker, and did not drink alcohol. Her family history was negative for scoliosis, cancer, connective tissue disease, and any neurological disorders.
Thirty years prior to her presentation to the chiropractor, at age 32, she had episodic nausea and dizziness that occurred about once per week depending on activity and lasted about 5 min. She was initially diagnosed with benign paroxysmal positional vertigo and treated with physiotherapy.
Sixteen years prior to presentation, at age 46, she began to have sudden loss of balance and unprovoked episodes of epilepsy. She then visited a neurosurgeon and underwent magnetic resonance imaging (MRI), which revealed herniation of the cerebellar tonsils through the foramen magnum greater than 5 mm and syringomyelia, and CM-I was accordingly diagnosed. Her primary care provider and neurosurgeon recommended surgery, and she underwent FMD that year.
The neurosurgeon performed a suboccipital craniectomy and laminectomy of C1 and C2 and simultaneously implanted a ventriculoperitoneal shunt. Following surgery, her neck pain, headache, and dizziness improved but were not completely alleviated. At this time, she still had occasional epileptic seizures, and these were managed with oral sodium valproate (200 mg) and levetiracetam (500 mg). At the time of presentation to the chiropractor, she had no recent seizures.
Six years prior to presentation to the chiropractor, at age 56, she began to experience bilateral upper limb weakness, worse on the right side, and revisited her neurosurgeon, who ordered a brain and cervical spine MRI, and computed tomography (CT) angiogram of the head without and with contrast. The CT angiogram exhibited small focal calcified plaque causing mild (20%) stenosis at the left carotid bulb, which was deemed to not be a source of her symptoms. The MRI revealed persistent syringomyelia; however, the surgeon reportedly determined that the patient was not a candidate for further surgeries and instead referred the patient to physical therapy.
At physical therapy, the patient recalled performing neck exercises and cervical traction; other specific details, however, were unclear. The patient also received acupuncture treatment. None of these therapies improved her symptoms, which slowly became worse.
She reported her episodes of neck pain and dizziness in the month prior to presenting to the chiropractor would occur 4 to 5 days per week, 3 to 4 times per day, depending on activity. She visited an orthopedic surgeon, who ordered full spine radiographs, which revealed a reversed cervical lordosis and degenerative changes of the cervical zygapophyseal and uncovertebral joints, suggestive of cervical spondylosis, as well as 3 mild scoliotic curvatures (Figure 1). The ventriculoperitoneal shunt appeared intact. The patient was prescribed a nonsteroidal anti-inflammatory drug and tramadol, 100 to 200 mg per day, and again was referred for physical therapy with cervical traction.
Because the patient had only temporary relief with these therapies previously and had progressively worsened over the past 6 years, she presented to a chiropractor for a second opinion.
CLINICAL FINDINGS:
The patient was brought by her husband to the chiropractor. Upon examination by the chiropractor, she was in distress and crying. She demonstrated a slow gait and held her husband’s arm to help maintain her balance while walking. She was slow to rise from a seated position and required the use of her arms to help push herself into a standing position. She had a kyphotic posture with her head and neck positioned anteriorly deviated to the right side. Muscle atrophy was evident, affecting the right upper extremity and hand and bilateral calf muscles. The patient also had a right claw hand deformity. Her active cervical range of motion was limited by pain to 10° of extension (normal >70°) and 40° of cervical rotation bilaterally (normal >80°), which appeared to trigger a spasm of the neck muscles. Although her lumbar range of motion was full, flexion caused a dull ache in the lower back. Palpation identified hypertonicity of the sternocleidomastoid, trapezius, rhomboid, and levator scapulae muscles bilaterally and tenderness at C2. A cranial nerve examination was normal, no overt cerebellar signs were noted (eg, intention tremor, nystagmus), and muscle stretch reflexes were normal bilaterally. Motion palpation identified restriction of the C4/5, C6/7, T2/3, and T7/8 segments.
The patient had diminished sensation to light touch and pain in the right lateral arm, forearm, and hand; however, temperature sense was not assessed. Her motor strengths for right shoulder abduction, arm flexion, extension, and wrist flexion and extension were 4 out of 5 (Medical Research Council scale) for each action. The patient also demonstrated lower extremity weakness with 4 out of 5 strength for hip flexion and extension, quadriceps extension, and plantar flexion bilaterally. Her grip strength was diminished bilaterally, as measured using a digital dynamometer (Jamar Plus, JLW Instruments, USA), which yielded 4.3 kg for the left hand (normal 20.7±4.6) and 8.7 kg for the right (dominant) hand (normal 25.0±4.6).
The chiropractor’s differential diagnosis included persistence of the patient’s syringomyelia, concurrent degenerative spondylosis causing cervical and lumbar radiculopathy, and cervical facet arthropathy related to scoliosis. The chiropractor also considered the possibility that the syringomyelia extended further inferiorly into the thoracic spinal cord. Given the patient’s complex medical history, including scoliosis and history of CM-I, syringomyelia, and previous FMD, which are precautions to certain manual therapies used by chiropractors, as well as her upper and lower extremity neurologic deficits, gait abnormality, and progressive worsening despite conservative care, the chiropractor ordered whole spine MRI, which was conducted that week.
The MRI revealed the presence of post-surgical FMD changes and syringomyelia extending from C1 to T9 (Figure 2). There was also cervical spondylosis with degenerative disc changes from C3 to C7. Most notably, at C4/5, there was moderate narrowing of the central canal and right neuroforamen, caused by disc displacement (Figures 3, 4). At C5/6, there was mild narrowing of the left neural foramen due to uncovertebral joint hypertrophy. At C6/7, there was a small disc osteophyte complex with an annular fissure causing mild canal stenosis and moderate right neuroforamen stenosis (Figure 4).
There was no evidence of dens retroflexion, pseudomeningocele, or other pathology in the vicinity of the prior FMD. The thoracic spine did not demonstrate any canal stenosis, with the only abnormality being the syrinx, which extended to the level of T9. The lumbar spine was relatively normal, showing only mild posterior disc bulges at L3/4, L4/5, and L5/S1, without nerve root compression.
The chiropractor considered the whole spine MRI findings to be most consistent with symptoms related to the patient’s cervicothoracic cord syrinx. In addition, the cervical spondylosis was considered to potentially account for some of the patient’s neck pain and upper extremity symptoms. In contrast, the lumbar spine findings were deemed inconsistent with a clinical diagnosis of lumbar radiculopathy. Accordingly, treatment focused on the cervical and thoracic regions rather than the lumbar spine.
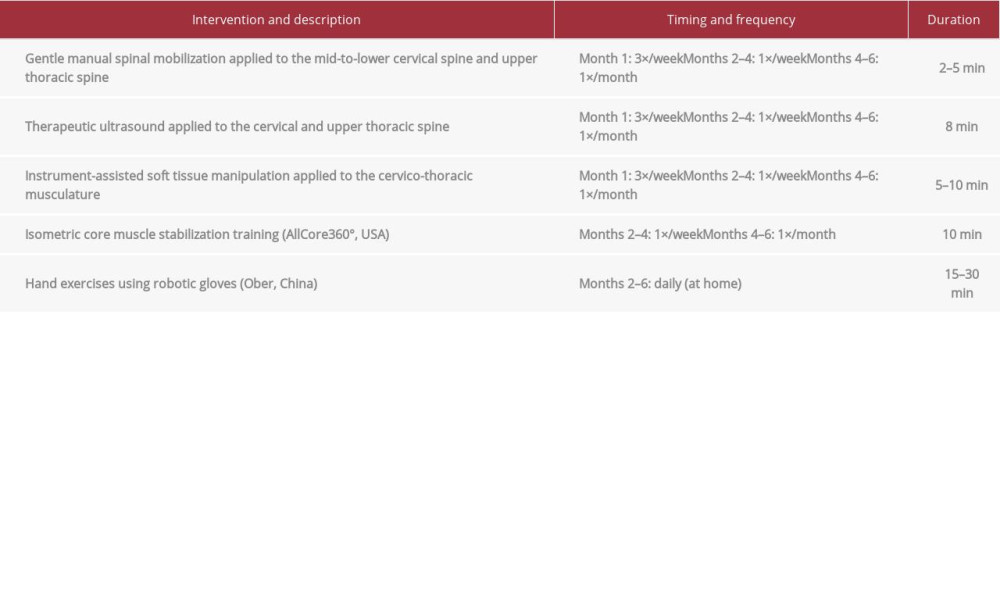
The patient consented to a chiropractic treatment plan which began at a frequency of 3 visits per week and included a variety of therapies (Table 1). Gentle manual spinal mobilization was administered to the mid to lower cervical and upper thoracic segments to alleviate muscle hypertonicity and restore spinal mobility (Figure 5). This treatment was well tolerated by the patient. Therapeutic ultrasound and instrument-assisted soft tissue manipulation (also called gua sha) using a massage tool (Strig, Korea) was applied to further alleviate muscular hypertonicity and reduce pain (Figure 6).
After the first week of care, the patient reported she was able to turn her head better without an increase in pain, yet her baseline pain was still severe at 7 to 8 out of 10. She also reported improvement in her grip strength, which improved to 4.9 kg on her left hand; however, her right hand strength remained similar at 8.8 kg.
After the first month of treatment, the patient’s reported neck pain severity decreased to 4 out of 10. Given the patient’s improvement, her visit frequency was reduced to once per week. After the second month of treatment, all numbness symptoms were resolved. The patient had stopped taking tramadol and was now able to use chopsticks. Low-impact isometric core muscle stabilization training was added, with the goal of strengthening the paraspinal muscles and spine and improving posture. This was accomplished by having the patient sit in a robotic device that rotated slowly at different angles of inclination while the patient maintained a neutral spine position; this was performed for 10 min per visit (AllCore360° [29], USA; Figure 7)
Hand exercises were also added, which were conducted using robotic gloves (Ober, China). These were rented to the patient for home use for 15 to 30 min per day (Figure 8). This type of robotic glove is used to augment hand motion for patients with weakness or functional deficits of the hand and fingers and has been previously studied for use with patients with spinal cord injury [30]. In the setting used, the device matched the patient’s own finger movement and provided mechanical assistance. The degree of assistance was reduced as the patient regained strength. The patient was recommended to perform tasks such as opening and closing the hands and squeezing a ball with the aid of the gloves.
At the 4-month follow-up, the patient no longer had neck pain, and her other symptoms were now mild or absent. Her active cervical spine range of motion improved to 40° of extension and 60° of cervical rotation bilaterally. Owing to her continued improvement, the patient’s visit frequency was reduced to once per month.
At the 6-month follow-up, the patient was pain free, with no neck pain or headaches. Her WHO-QOL score improved to 80%. Measurement of grip strength showed improvements to 5.8 kg (left hand) and 10.0 kg (right hand), and upon visual inspection, her anterior head posture had improved. The patient still had residual slowness of gait and limitations of strength, and although she could eat more easily, she still had difficulty cooking due to an inability to hold pots and pans. Because of these subjective and objective measures of improvement, the patient chose to remain in chiropractic care with monthly appointments.
The patient provided written consent for the publication of this case report and accompanying images. There were no adverse events in relation to the multimodal chiropractic interventions provided.
Discussion
LIMITATIONS:
First, as a single case, the results shown may not be generalizable to all patients following FMD. It is possible that the patient’s cervical spondylosis played a role in her response to manual therapies and exercise. In contrast, other patients with persistent symptoms after FMD may not have concomitant spondylosis and thus may not respond to a similar treatment program. Second, several tests were unavailable in the present case that could have aided in objective measures of improvement, such as balance testing and functional gait assessment. Further, images from before the patient’s surgery were unavailable upon request and only imaging after surgery could be identified. Finally, our literature search for similar cases describing the use of manual therapies for patients with persistent symptoms after FMD included PubMed, the Index to Chiropractic Literature, and Google Scholar. This search identified only a conference abstract and case report, which was not indexed in PubMed [8,23]. Accordingly, these references have limited detail and/or reliability.
Conclusions
This case demonstrates an adult woman with recalcitrant neck pain and headache complicated by a chronic, persistent cervicothoracic cord syrinx after FMD for CM-I who improved after a combination of conservative chiropractic and rehabilitative therapies. Despite the success in this case, there remains a limited, low level of evidence supporting the therapies used in this case for patients with neck pain, headache, or other symptoms and syringomyelia after FMD for CM-I. These treatments should not be broadly applied to other similar patients and should be approached with caution on a case-by-case basis. Further research should examine the safety and efficacy of such therapies in this patient population.
Figures
References:
1.. van Dellen JR, Chiari malformation: An unhelpful eponym: World Neurosurgery, 2021; 156; 1-3
2.. George TM, Higginbotham NH, Defining the signs and symptoms of Chiari malformation type I with and without syringomyelia: Neurol Res, 2011; 33; 240-46
3.. Vandertop WP, Syringomyelia. Neuropediatrics: Georg Thieme Verlag KG, 2014; 45; 3-9
4.. Schuster JM, Zhang F, Norvell DC, Hermsmeyer JT, Persistent/recurrent syringomyelia after chiari decompression – natural history and management strategies: A systematic review: Evid Based Spine Care J, 2013; 4; 116-25
5.. Soleman J, Bartoli A, Korn A, Treatment failure of syringomyelia associated with Chiari I malformation following foramen magnum decompression: How should we proceed?: Neurosurg Rev, 2019; 42; 705-14
6.. Heiss JD, Suffredini G, Smith R, Pathophysiology of persistent syringomyelia after decompressive craniocervical surgery: J Neurosurg Spine, 2010; 13; 729-42
7.. Mugge L, Caras A, Henkel N, Headache and other symptoms in Chiari malformation type I are associated with cerebrospinal fluid flow improvement after decompression: A two-institutional study: World Neurosurg, 2022; 163; e253-62
8.. Aslıyüce YÖ, Ülger Ö, Efficacy of suboccipital release and stabilization exercise training in type 1 Chiari malformation patient undergoing surgical treatment: A case report: Int J Sport Exerc Health Res, 2021; 5; 30-33
9.. Parmar H, Shah JK, Gaud J, Observational outcome in surgery for Chiari malformation patients: Int Surg J, 2020; 7; 3068-72
10.. Bahk J, Poquiz P, Syrinx formation associated with chiropractic cervical spinal manipulation: roceedings of UCLA Health, 2021; 25
11.. Leong WK, Kermode AG, Acute deterioration in Chiari type 1 malformation after chiropractic cervical manipulation: J Neurol Neurosurg Psychiatry, 2001; 70; 816-17
12.. Scully RE, Mark EJ, McNeely WF, McNeely BU, Case 3-1987: New Engl J Med, 1987; 316; 150-57
13.. Zink E, Lohenry K, Williams J, Acute exacerbation of Chiari I symptoms after chiropractic intervention: 67. JAAPA, 2007; 20; 67-68
14.. Elam MJ, Vaughn JA, Chiari type I malformations in young adults: Implications for the college health practitioner: J Am Coll Health, 2011; 59; 757-59
15.. McArthur RA, Arnold–Chiari type I malformation: A look at two cases in the adult: J Can Chiropr Assoc, 1994; 38; 203
16.. Francio VT, Syringomyelia and Arnold-Chiari malformation associated with neck pain and left arm radiculopathy treated with spinal manipulation: Case Rep, 2014; 2014; bcr2014207319
17.. Hock S, Kelly A, Reduction of headaches in a patient with type I Chiari malformation and Ehlers-Danlos following chiropractic care to correct vertebral subluxation: A case study: Ann Vert Sublux Res; 2021; 18-23
18.. Murphy D, Goldstein D, Katz M, Chiropractic adjustment to the cervical spine and the Arnold-Chiari malformation: J Manipulative Physiol Ther, 1993; 16; 550-55
19.. Thakur JD, Storey C, Kalakoti P, Early intervention in cauda equina syndrome associated with better outcomes: A myth or reality? Insights from the Nationwide Inpatient Sample database (2005–2011): J Spine, 2017; 17; 1435-48
20.. Sergent AW, Cofano GP, Chiropractic care for headaches and dizziness of a 34-year-old woman previously diagnosed with Arnold-Chiari malformation type 1: J Chiropr Med, 2014; 13; 192-95
21.. Smith J, Effects of upper cervical subluxation concomitant with a mild Arnold-Chiari malformation: A case study: Chiropr Res J, 1997; 4; 77-81
22.. Zhu G-D, Wei X-Y, Case report adult syringomyelia associated with Chiari I malformation treated with cervical manipulation: A case report: Int J Clin Exp Med, 2018; 11; 8783-87
23.. Boesch R, Losby S, Olsheski C, Arnold Chiari malformation and chiropractic care for headaches: Two cases. Abstracts of ACC Conference Proceedings: Poster presentations: J Chiropr Educ; 2010; 122
24.. Smith R, Jones G, Curtis A, Are established methods of physiotherapeutic management for long-term neurological conditions applicable to ‘orphan’ conditions such as syringomyelia?: Physiother Res Int, 2016; 21; 4-21
25.. Osama M, Yaqoob F, Cervical syringomyelia: Conservative physical therapy management of a patient: A case report: Professional Med J, 2017; 24; 627-32
26.. Yoo H-J, Kim M-K, Lee D-H, Case reports on neck pain with cervical syringomyelia patients treated by Korean medical therapy: The Journal of Korea CHUNA Manual Medicine for Spine and Nerves, 2015; 10; 107-16
27.. Choi HY, Jeong JE, Lee JS, A case of syringomyelia with back and shoulder pain: J Acupunct Res, 2019; 36; 45-49
28.. Haas JW, Harrison DE, Harrison DD, Bymers B, Conservative treatment of a patient with syringomyelia using chiropractic biophysics protocols: J Manipulative Physiol Ther, 2005; 28; 452.e1-e7
29.. Palevo G, Walsh DJ, Park E, Physiological responses to Allcore360° core training system: J Exerc Physiol Online, 2021; 24; 67-74
30.. Cappello L, Meyer JT, Galloway KC, Assisting hand function after spinal cord injury with a fabric-based soft robotic glove: J Neuroeng Rehabil, 2018; 15; 59
31.. Mehta A, Chilakamarri P, Zubair A, Kuruvilla D, Chiari headache: Curr Pain Headache Rep, 2018; 22; 49
32.. Yuan C, Guan J, Du Y, Repeat craniocervical decompression in patients with a persistent or worsening syrinx: A preliminary report and early results: World Neurosurg, 2020; 138; e95-105
33.. Gore DR, Roentgenographic findings in the cervical spine in asymptomatic persons: A ten-year follow-up: Spine, 2001; 26; 2463-66
34.. Lee H-D, Jeon C-H, Chung N-S, Is the severity of cervical foraminal stenosis related to the severity and sidedness of symptoms?: Healthcare (Basel), 2021; 9; 1743
35.. Iyer S, Kim HJ, Cervical radiculopathy: Curr Rev Musculoskelet Med, 2016; 9; 272-80
36.. Borrella-Andrés S, Marqués-García I, Lucha-López MO, Manual therapy as a management of cervical radiculopathy: A systematic review: Biomed Res Int, 2021; 2021; e9936981
37.. Alpaslan M, Ozkacmaz S, Dadali Y, Ucar I, Association of Chiari type 1 malformation and cervical spine curve changes: J Anat Soc India, 2021; 70; 162
38.. Padua L, Padua R, LoMonaco M, Tonali P, Radiculomedullary complications of cervical spinal manipulation: Spinal Cord, 1996; 34; 488-92
39.. Malone DG, Baldwin NG, Tomecek FJ, Complications of cervical spine manipulation therapy: 5-year retrospective study in a single-group practice: Neurosurg Focus, 2002; 13; ecp1
Figures
In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250