28 April 2023: Articles 
Splinter Cataract in Patients with Keratoconus and Frequent Eye Rubbing: A Novel Finding
Unknown etiology
Omar Kirat1ABCDE, Muhammad A. AhadDOI: 10.12659/AJCR.939082
Am J Case Rep 2023; 24:e939082
Abstract
BACKGROUND: Patients with keratoconus are at increased risk of developing cataract at a younger age compared to the normal population. Predisposing factors include atopy and topical steroid use. In this case series we report the novel observation of splinter-shaped cortical cataract in 16 eyes of 14 patients with keratoconus in the absence of other risk factors of cataract development from a single center in Riyadh, Saudi Arabia.
CASE REPORT: This is a retrospective review of 16 eyes of 14 patients diagnosed with keratoconus and found to have splinter cortical cataract. Twelve patients had unilateral and 2 patients had bilateral splinter cortical cataract in the inferotemporal quadrant of the crystalline lens. Thirteen eyes (81.25%) had clinically proven keratoconus and 3 eyes (18.75%) were keratoconus suspects. All patients affirmed frequent eye rubbing and 62.5% of eyes had a history of vernal keratoconjunctivitis. Best corrected visual acuity (BCVA) by the logarithm of the minimum angle of resolution (LogMAR) was reported between 0 to 0.2 in 69% of eyes (11 eyes) and 4 eyes (25%) had BCVA of 0.3 to 0.6, and 1 eye (6%) had BCVA of 1.3.
CONCLUSIONS: Splinter-shaped cortical cataract could be a sign of frequent eye rubbing. Careful examination of the crystalline lens with dilated pupil may reveal peripheral cortical opacities in the inferotemporal quadrant, which can alert the physician that the patient has habitual eye rubbing and is at increased risk of keratoconus development or progression.
Keywords: Cataract, Keratoconus, Humans, Risk Factors, Retrospective Studies, Foreign Bodies
Background
Cataract is defined as any change in crystalline lens clarity that obscures passage of light through the lens to the retina [1]. The changes in the lens transparency and refractive index are a result of a shift in the water content and type of proteins in the crystalline lens [1]. Cataract can be classified according to the area of the lens that is affected (nuclear sclerotic, cortical, or subcapsular) [1]. Multiple risk factors have been associated with cataract formation, including age, trauma, inflammation, smoking, chronic ultraviolet light exposure, metabolic disorders, and use of certain medications [2,3]. The onset of age-related cataract formation typically happens in the fifth and sixth decade of life [4].
Patients with keratoconus are at increased risk of developing cataract at a younger age compared to the normal population, and predisposing factors include atopy and topical steroid use [5,6]. Atopy is the most significant risk factor for the development of keratoconus, as vigorous and prolonged eye rubbing can lead to irreversible corneal thinning and scar formation [7]. Cataracts in patients with atopic dermatitis are either anterior or posterior subcapsular cataract [8], while glucocorticoid use is usually associated with posterior subcapsular cataract [9]. In this case series we report the novel observation of splinter-shaped cortical cataract in 16 eyes of 14 patients with keratoconus in the absence of other risk factors of cataract development from a single center in Riyadh, Saudi Arabia.
Case Report
This is a case series of 16 eyes of 14 patients diagnosed with keratoconus and found to have splinter cortical cataract. Patients were enrolled from the Ophthalmology outpatient clinic at a tertiary eye care hospital in Riyadh, Saudi Arabia from January 2017 to March 2022. Retrospective review of charts was carried out and demographic data, including age and gender, were recorded, as well as history of atopy, medical comorbidities, history of smoking, and medications use, including steroids. Patients were also asked about past or current history of eye rubbing, and to illustrate the significance of eye rubbing, certain variables were ascertained, including the duration of eye rubbing, gentle or vigorous in nature, and unilateral or bilateral. Complete ocular examination was performed, including uncorrected (UCVA) and best corrected visual acuity (BCVA), slit-lamp examination, Pentacam® tomography (Oculus Systems, Wetzlar, Germany), and all results were recorded. Slit-lamp photography of the lens was conducted for all patients.
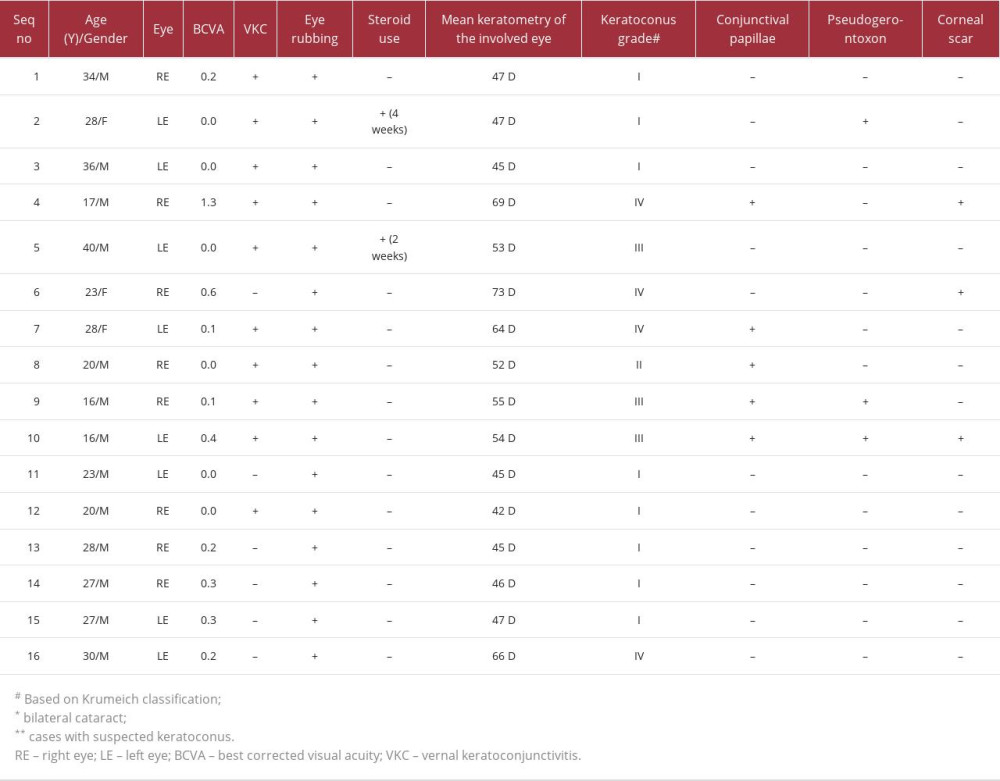
A total of 16 eyes of 14 patients were included in this case series. Eleven patients (78.6%) were male and 3 patients (21.4%) were female. Patients had an average age of 26 years (range, 16–40). All eyes had splinter-shaped cortical cataract in the inferotemporal quadrant of the crystalline lens and not involving the visual axis. The location of the cataract corresponded to the keratoconus cone location in 12 out of 16 eyes (75%). This sign was first described by the principal investigator of this series (Dr. Omar Kirat). Two patients had bilateral splinter cortical cataract (14%) and 3 patients had visually significant corneal scar (21.4%). A history of vernal keratoconjunctivitis (VKC) was found in 62.5% of eyes (10 eyes) and all patients gave a positive history of frequent eye rubbing. Only 2 eyes of 2 patients had a history of using a short course of topical steroids. None of the patients had a history of systemic steroid use. Six eyes (37.5%) had positive vernal signs of slit-lamp examination, such as conjunctival papillae and pseudogerontoxon. Slit-lamp photographs of the lens changes are shown in Figure 1. Fundus examination was normal in all patients. Best corrected visual acuity (BCVA) by the logarithm of the minimum angle of resolution (LogMAR) was reported between 0 to 0.2 in 69% of eyes (11 eyes) and 4 eyes (25%) had BCVA of 0.3 to 0.6, and 1 eye (6%) had BCVA of 1.3. Thirteen eyes (81%) had clinically proven keratoconus, while 3 eyes (19%) were keratoconus suspects. Based on Krumeich classification of keratoconus [10], 8 out of 16 eyes (50%) had stage I keratoconus, 1 eye had stage II (6%), 3 eyes (19%) had stage III, and 4 eyes (25%) had stage IV keratoconus. The complete details of patients with their keratometry values are tabulated in Table 1.
Discussion
Keratoconus has been associated with multiple etiologies and risk factors in the literature, such as ethnic background, genetic and environmental factors, ultraviolet (UV) exposure, and, most importantly, eye rubbing [11]. Eye rubbing is a common habit among individuals, which can occur spontaneously or as a response to ocular irritation and fatigue or compulsive eye rubbing in individuals with mental illness [12]. Chronic abnormal eye rubbing is associated with keratoconus development [11], and repetitive and vigorous knuckle-grinding rubbing is associated with progression of keratoconus [13]. In this case series we report an intriguing observation of splinter-shaped cortical cataract in the inferotemporal quadrant of the crystalline lens in patients with habitual eye rubbing.
There are many proven consequences of eye rubbing on ocular structures in the literature [13–16]. An experimental study asked volunteers to rub their eyes for 60 seconds and tear samples were collected and tested, showing that multiple inflammatory markers were significantly raised after eye rubbing, including matrix metalloproteinase-13 and interleukin-6 and tumor necrosis factor-a [13]. These markers are believed to play a role in the development of keratoconus [17]. Increased corneal temperature and spikes in intraocular pressure (IOP) were also observed [18]. Yusuf and Salmon reported a case of iridoschisis and keratoconus in a patient with compulsive eye rubbing [15]. Panikkar et al reported a case of bilateral retinal detachment secondary to vigorous eye rubbing in an 18-year-old male with obsessive compulsive disorder [16].
To the best of our knowledge, there are no existing reports of splinter-shaped cataract formation secondary to frequent eye rubbing in keratoconus patients. In this case series of 16 eyes, we report the presence of splinter-shaped cortical cataract in the inferotemporal quadrant of the crystalline lens, and all eyes had a history of frequent eye rubbing. Stage I keratoconus was the most common (50%) among 16 eyes, followed by stage IV, then stage III (25% and 19%, respectively) and lastly stage II (6%), which may indicate that splinter-shaped cataract is not limited to a certain stage of keratoconus severity. The morphology of the cataract described in this case series is unlike the cataract frequently found in keratconic eyes. For example, atopy-related cataract is described as anterior subcapsular opacities [8,19], while steroid-induced cataract has a characteristic appearance of opacities confined in the posterior subcapsular area of the crystalline lens [9].
It is important to highlight that the clinical diagnosis of this sign can be easily missed because the opacities are usually found in the periphery of the crystalline lens, as shown in the clinical photographs; therefore, meticulous dilated-pupil examination of the crystalline lens is critical to making a diagnosis. Splinter-shaped cataract reported in this case series did not involve the visual axis; therefore, cataract removal was not warranted. All patients were observed with periodic IOP assessment. Most of the eyes reported in this series had unilateral cataract except for 2 patients who had bilateral cataract, and this could be attributed to many factors, including the pattern of eye rubbing and hand dominance. Similarly, Kymionis et al reported unilateral keratoconus in a patient with bilateral eye rubbing related to hand dominance [20].
The mechanism of cataract development with frequent eye rubbing is not completely understood. However, a few theories have been proposed, one of which is that repetitive mechanical rubbing of the cornea or iris against the crystalline lens could be responsible for cataract development. Furthermore, ocular rigidity is reduced in ectatic corneas [21,22], which might support the theory that mechanical rubbing, even in mild forms, in patients with keratoconus can play a role in cataract development due to greater corneal deformability.
This case series also illustrates that 75% of eyes had correspondence between the cataract and the inferotemporal cone location on topography. The inferotemporal location of the cataract could be related to the usual site of contact with the eye during rubbing by fingers or knuckles. Similarly, a study investigating the effect of eye rubbing on corneal epithelium showed significant thinning in the inferotemporal quadrant on anterior segment optical coherence tomography [23]. Other theories include inflammatory mechanism related to increased mediators secondary to eye rubbing [13,24], and intermittent elevation in IOP triggered by eye rubbing might play a role in cataract development [25]. Another possibility is that the lens undergoes ectasia similar to what happens to the cornea during eye rubbing.
The limitations of this case series include the lack of a control group, the lack of an objective and quantifiable measure of eye rubbing frequency and intensity due to recall bias, and the limited possibility to establish a cause-effect relationship. Furthermore, the results should be interpreted with caution due to the small sample size. However, we believe that by reporting this sign we can stimulate researchers and scientists to investigate the proposed hypotheses by experimental studies. Informed consent was obtained from all patients to publish clinical/topography/slit-lamp images. The study adhered to the Declaration of Helsinki and was approved by the Institutional Research Board (KKESH, RP 22043-R) at King Khaled Eye Specialist Hospital.
Conclusions
In conclusion, splinter-shaped cortical cataract could be a sign of frequent eye rubbing. Careful examination of the crystalline lens with dilated pupil might reveal peripheral cortical lens opacities in the inferotemporal quadrant, which can alert the physician that the patient has habitual eye rubbing and is at increased risk of keratoconus development or progression, which warrants patient counselling for behavioral change. Splinter-shaped cataract is visually insignificant and can be managed with observation alone with periodic IOP assessment.
References:
1.. , Cataracts in Adults: Management National Institute for Health and Care Excellence (NICE), 2017 Available at: https://www.ncbi.nlm.nih.gov/books/NBK464182/
2.. West S, Epidemiology of cataract: Accomplishments over 25 years and future directions: Ophthalmic Epidemiol, 2007; 14(4); 173-78
3.. Chang JR, Koo E, Agrón E, Risk factors associated with incident cataracts and cataract surgery in the Age-Related Eye Disease Study (AREDS). AREDS Report Number 32: Ophthalmology, 2011; 118(11); 2113-19
4.. Nizami AA, Gulani AC: Cataract, StatPearls Published online July 5, 2022. Accessed January 1, 2023. Available at: https://www.ncbi.nlm.nih.gov/books/NBK539699/
5.. Moshirfar M, Walker BD, Birdsong OC, Cataract surgery in eyes with keratoconus: A review of the current literature: Curr Opin Ophthalmol, 2018; 29(1); 75-80
6.. Thebpatiphat N, Hammersmith KM, Rapuano CJ, Cataract surgery in keratoconus: Eye Contact Lens, 2007; 33(5); 244-46
7.. Bawazeer AM, Hodge WG, Lorimer B, Atopy and keratoconus: A multivariate analysis: Br J Ophthalmol, 2000; 84(8); 834-36
8.. Bair B, Dodd J, Heidelberg K, Krach K, Cataracts in atopic dermatitis: A case presentation and review of the literature: Arch Dermatol, 2011; 147(5); 585-88
9.. Jobling AI, Augusteyn RC, What causes steroid cataracts? A review of steroid-induced posterior subcapsular cataracts: Clinical Exp Optom, 2002; 85(2); 61-75
10.. Gore DM, Shortt AJ, Allan BD, New clinical pathways for keratoconus: Eye (Basingstoke), 2013; 27(3); 329-39
11.. Gordon-Shaag A, Millodot M, Shneor E, The epidemiology and etiology of keratoconus: Int J Keratoconus Ectatic Corneal Dis, 2012; 1(1); 7-15
12.. Hawkes E, Nanavaty MA, Eye rubbing and keratoconus: A literature review: Int J Keratoconus Ectatic Corneal Dis, 2014; 3(3); 118-21
13.. Balasubramanian SA, Pye DC, Willcox MDP, Effects of eye rubbing on the levels of protease, protease activity and cytokines in tears: Relevance in keratoconus: Clin Exp Optom, 2013; 96(2); 214-18
14.. Liu WC, Lee SM, Graham AD, Lin MC, Effects of eye rubbing and breath holding on corneal biomechanical properties and intraocular pressure: Cornea, 2011; 30(8); 855-60
15.. Yusuf IH, Salmon JF, Iridoschisis and keratoconus in a patient with severe allergic eye disease and compulsive eye rubbing: A case report: J Med Case Rep, 2016; 10(1); 134
16.. Panikkar K, Manayath G, Rajaraman R, Saravanan V, Progressive keratoconus, retinal detachment, and intracorneal silicone oil with obsessive-compulsive eye rubbing: Oman J Ophthalmol, 2016; 9(3); 170-73
17.. Galvis V, Sherwin T, Tello A, Keratoconus: An inflammatory disorder?: Eye, 2015; 29(7); 843-59
18.. McMonnies CW, Mechanisms of rubbing-related corneal trauma in keratoconus: Cornea, 2009; 28(6); 607-15
19.. Brunsting LA, Reed WB, Bair HL, Occurrence of cataracts and keratoconus with atopic dermatitis: AMA Arch Derm, 1955; 72(3); 237-41
20.. Kymionis GD, Blazaki SV, Tsoulnaras KI, Corneal imaging abnormalities in familial keratoconus: J Refract Surg, 2017; 33(1); 62-63
21.. Moshirfar M, Edmonds JN, Behunin NL, Christiansen SM, Corneal biomechanics in iatrogenic ectasia and keratoconus: A review of the literature: Oman J Ophthalmol, 2013; 6(1); 12-17
22.. Fontes BM, Ambrósio R, Velarde GC, Nosé W, Ocular response analyzer measurements in keratoconus with normal central corneal thickness compared with matched normal control eyes: J Refract Surg, 2011; 27(3); 209-15
23.. Loureiro T, Rodrigues-barros S, Carreira AR, Corneal epithelium remodelling after eye rubbing discontinuation in pediatric allergic patients: Revista da Sociedade Portuguesa de Oftalmologia, 2021; 45; 210-17
24.. Kallinikos P, Efron N, On the etiology of keratocyte loss during contact lens wear: Invest Ophthalmol Vis Sci, 2004; 45(9); 3011-20
25.. Khazaeni B, Khazaeni L: Acute closed angle glaucoma, StatPearls Published online April 30, 2022. Available at: https://www.ncbi.nlm.nih.gov/books/NBK430857/
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250