10 July 2023: Articles 
Chylothorax: A Tangled Road to Definitive Diagnosis of Non-Hodgkin Lymphoma
Unusual clinical course, Challenging differential diagnosis
Andra Krūmiņa12ABDEF*, Daiga Auziņa23ABDE, Arta Legzdiņa12ABEF, Sandra Lejniece23ADEDOI: 10.12659/AJCR.939098
Am J Case Rep 2023; 24:e939098
Abstract
BACKGROUND: Chylothorax is a rare condition caused by the leak of chyle into the pleural cavity. Malignancy, especially advanced lymphomas, are the most common non-traumatic causes of chylothorax. When thoracentesis and the following pleural effusion studies reveal the fluid to be a chyle, it is important to look at the patients’ history and understand the possible etiological factors, as the appropriate management can differ. In some instances, the true reason behind the chylothorax can be a diagnostic challenge, as presented in this case.
CASE REPORT: We report a case of a patient in her 70s presenting with progressive dyspnea at rest and non-productive cough. A chest X-ray showed subtotal right pleural effusion that was revealed to be a chylothorax. A CT scan was performed and revealed mediastinal, abdominal, and retroperitoneal lymphadenopathy, that, compared to the CT results 6 years ago, when for the first time enlarged lymph nodes were discovered by thyroid ultrasound, was without any progression. Initial diagnostic tests were inconclusive, and the goal was to rule out other differential diagnoses while maintaining a minimally invasive diagnostic approach. A video-assisted thoracoscopic surgery with mediastinal lymph node dissection and biopsy led to a diagnosis of follicular lymphoma.
CONCLUSIONS: This clinical case highlights not only an uncommon follicular lymphoma complication but also is an example of a diagnostic challenge due to certain clinical features being misleading from the true cause of the chylothorax. After a wide variety of investigations were applied, the patient was finally diagnosed with non-Hodgkin lymphoma. Successful treatment led to a full metabolic remission.
Keywords: chylothorax, Lymphoma, Follicular, Female, Humans, Lymphoma, Non-Hodgkin, Pleural Effusion, Lymph Nodes
Background
A chylothorax is a rare condition caused by the leak of chyle into the pleural cavity, defined by pleural fluid triglyceride levels >1.24 mmol or >110 mg/dl, presence of chylomicrons, and low cholesterol level. Historically, non-traumatic chylothorax was the leading etiological cause, but in recent years it has shifted towards traumatic chylothorax, which now accounts for more than 50% of cases described in the literature. Among traumatic cases, the leading cause is iatrogenic, due to damage to the thoracic duct during thoracic surgery [1]. It is well established that malignancy, especially advanced lymphomas, are the most common non-traumatic causes of chylothorax [2]. Less common non-traumatic etiologies include other malignancies (eg, lung cancer, Kaposi sarcoma, myeloma), infections (eg, tuberculosis, filariasis), SVC thrombosis, lymphangioleiomyomatosis, sarcoidosis, and fibrosing mediastinitis [3].
In lymphoma patients there are 2 mechanisms that could lead to chyle reflux into the pleural cavity. The first mechanism involves the thoracic duct or its collaterals being infiltrated by lymphomatous tissue or externally compressed by enlarged lymph nodes. Chylothorax due to a duct obstruction is almost exclusively left-sided [4]. The second mechanism is thoracic duct rupture. If the thoracic duct is infiltrated by lymphomatous tissue, its structure changes, becoming increasingly rigid and susceptible to rupture. That can happen with even the slightest and often unnoticed trauma as simple as hyperextension of the vertebral column, sneezing, coughing, or anything that results in sudden increase of intrathoracic pressure [5].
When thoracentesis and subsequent pleural effusion studies reveal the fluid to be chyle, it is important to look at the patients’ history and understand the possible etiological factors, as the appropriate management can differ. Classically, chylothorax treatment includes 1 or more of multiple interventions that are classified under 3 categories: treatment of the underlying condition, conservative management, and surgical management.
In some instances, the true reason behind the chylothorax can be a diagnostic challenge, as presented in our case. Certain features of this case were unusual and thus led to a broad approach of differential diagnoses. The fact that the patient had a long-standing history of lymphadenopathy that had previously been treated, as well as recent scans showing no progression, made this case challenging and required a multidisciplinary approach. This clinical case also proves how challenging it can sometimes be to diagnose lymphomas overall, especially slow-growing follicular lymphomas. Initial symptoms may vary and patients can be asymptomatic for years and later present with sudden nonspecific symptoms involving other organ systems.
Case Report
A 73-year-old woman presented with progressive dyspnea at rest and non-productive cough. Chest radiography showed subtotal right-side pleural effusion. The patient was admitted to a hospital for further investigations. During clinical examination, she mentioned that her dyspnea started shortly after lifting heavy boxes that same day. She had no known history of serious illnesses. Six years prior to this episode, due to pain in the right side of the neck, she was investigated for cervical, mediastinal, and abdominal lymphadenopathy, and a thyroid ultrasound revealed cervical lymphadenopathy. At that time, a neck lymph node biopsy was performed, but histologically there were no signs of specific changes or malignancy. Until the development of respiratory symptoms, the patient felt well and healthy.
At the time of admission, her oxygen saturation by pulse oximetry was 96% on room air and her respiratory rate was 18 breaths per minute. Physical examination revealed diminished breath sounds over the right lung field and dullness to percussion there.
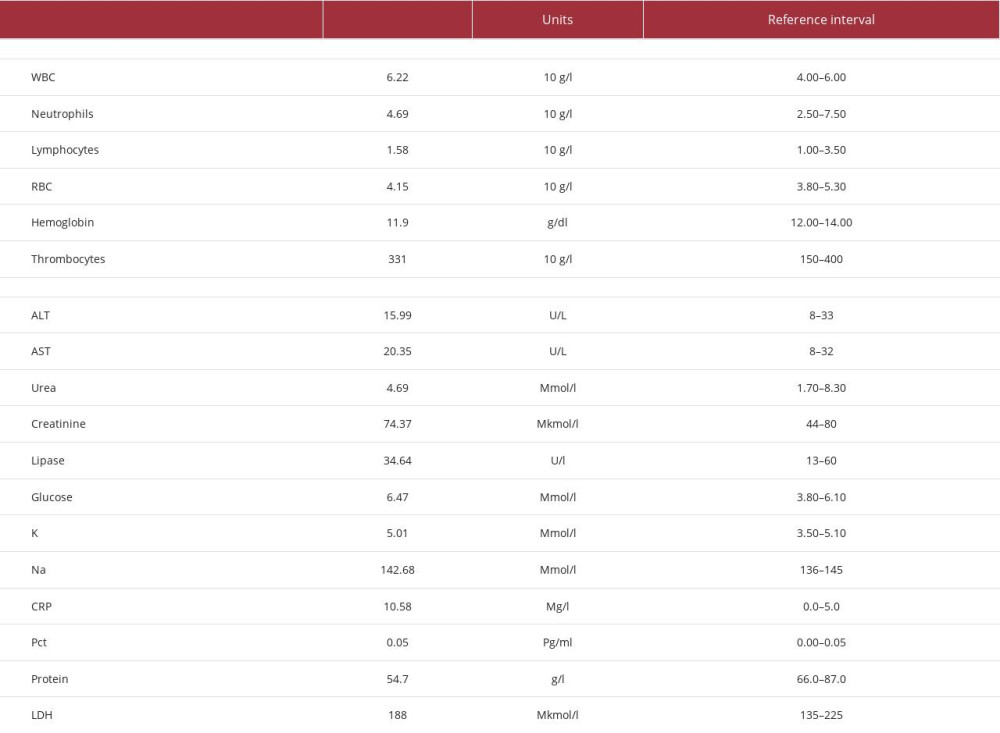
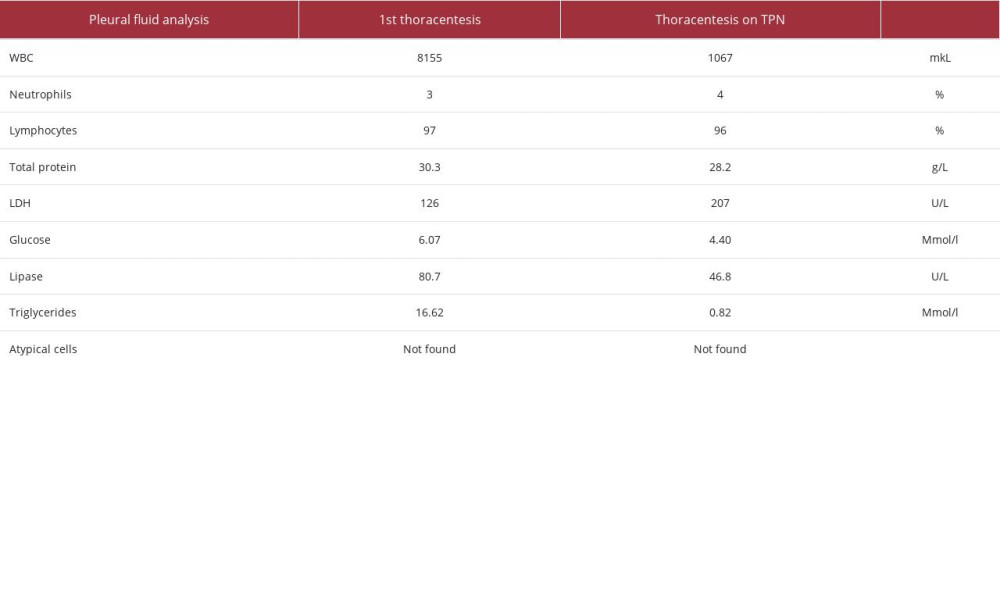
Complete blood count, coagulation panel, and basic metabolic panel showed no significant changes (Table 1). During thoracentesis, about 1500 mL of white, cloudy fluid was evacuated (Figure 1). Pleural effusion studies revealed a lymphocyte-dominant (97% of total leukocyte count) exudative pleural effusion with no malignant cells. Biochemical examination of pleural fluid revealed total protein of 30.3 g/L (reference interval (RI) 10–20 g/L), lipase of 80.7 U/L (RI 30–110 U/L), and lactate dehydrogenase of 126 U/L (reference interval (RI) 135–214 U/L), revealing discordant exudate (positive only by protein levels). Additionally, testing of triglyceride levels was performed, showing significant elevation at 16.62 mmol/L (RI < 2 mmol/L), confirming the presence of chylothorax (Table 2). Intercostal drainage was used. A computed tomography (CT) scan of the chest and abdomen with contrast was performed and revealed mediastinal (the biggest lymph nodes 1.1–2.2 cm), abdominal (0.9 cm), and retroperitoneal (1.3 cm) lymphadenopathy, that compared to the examination 6 years prior, was without any negative trend, and some of the lymph nodes had even decreased in size. Considering these findings and unclear etiology of chylothorax at that point, a multidisciplinary discussion (MDD) was held, and a comprehensive examination plan was created. As no progression of the lymphadenopathy was noted, the hematologist and surgeon were of the opinion that hematological disease is unlikely and before any major surgical interventions and lymph node biopsy, other most probable causes of chylothorax should be ruled out. Also, the patient agreed to a less invasive approach at first. All the microbiological investigations, including testing for tuberculosis, came back negative. To rule out any gastrointestinal tract changes or malignancy, as by the recommendations of the surgeon, gastroscopy and colonoscopy were performed, but revealed no abnormal findings. The results of phenotypic lymphocyte screening by flow cytometry of both blood and pleural fluid showed no evidence of lymphoproliferative disease. Furthermore, an interventional pneumonologist performed medical thoracoscopy with pleural biopsy only. The histological examination revealed pleural tissue fragments with active inflammation and edema without any signs of malignancy.
Simultaneously, the patient was started on total parenteral nutrition (TPN) to decrease the production of chyle fluid and its leakage into the pleural space. At first oral feeding with modifications was tried, but it proved to be unsuccessful, and the daily fluid output would not significantly decrease. During TPN, the triglyceride level in pleural fluid decreased to 0.82 mmol/L and intercostal drainage was around 600 ml in 24 h (Table 2).
After 2 weeks, total parenteral nutrition was discontinued but intercostal drainage significantly increased to ≥1100 ml in a 24-h period. Another MDD was held and as the chylothorax etiology was still unclear, the possibility of both lymphoproliferative disease or suspected thoracic duct leak due to possible injury were the main differentials, a decision was made to perform a video-assisted thoracoscopic surgery (VATS) with mediastinal lymph node dissection and thoracic duct clipping. During VATS subcarinal lymph node (7th mediastinal lymph node group) was dissected. Histological and immunohistochemical examination was performed, describing multiple pseudo-follicular and nodular structures, aggregates of small lymphoid B cell: CD20+, CD10+, BCL2+, Ki-67+ (10–20%), CD23+, Cyclin D1, with the conclusion of a morphological and immunohistochemical picture of follicular lymphoma, Grade I. After thoracic duct clipping, the chyle leak continued but the output was significantly lower, and it was able to be managed with dietary modifications.
Three weeks after VATS, the patient had a consult with a hematologist, and to assess the spread of the disease underwent a positron emission tomography scan (PET/CT), where increased metabolic activity was observed in the lower lobe of the right lung (Deauville 4), as well as mediastinal and mesenteric lymph nodes (Deauville 3) (Figure 2).
After confirmation of a diagnosis, the patient started chemotherapy according to the R-CVP regimen with intravenous rituximab 375 mg/m2, cyclophosphamide 400 mg/m2, vincristine 1.4mg/m2, and prednisolone 100 mg/m2 p.o. The patient responded well to the treatment. After the 3rd chemotherapy course, a PET/CT examination was performed, showing small residual mediastinal (Deauville 1), abdominal (Deauville 3), and retroperitoneal (Deauville 1) lymphadenopathy, without pathological hypermetabolism was observed, as well as a complete metabolic remission picture, and right pleural effusion (chylous exudate), with a downward trend. No metabolic activity was observed in the lungs. The patient received an additional 3 chemotherapy treatment courses, with follow-up PET/CT examination, and complete metabolic remission was confirmed (PET-negative) (Figure 3).
Currently, the patient continues to receive maintenance therapy with rituximab every 2 months for a total of 2 years.
Discussion
Follicular lymphoma (FL) is typically a slow-growing or indolent form of non-Hodgkin lymphoma (NHL) derived from germinal B cells that are mixed with nonmalignant cells. FL is the second most common nodal lymphoma and occurs at a median age of 60 years [6].
Chylothorax is a rare condition accounting for up to 3% of all pleural effusions, with traumatic cases outnumbering all non-traumatic etiologies combined [7,8]. It is caused by disruption or obstruction of the thoracic duct or collaterals with leakage of chyle into the pleural space [9]. Chyle consists of lymph from interstitial fluid and emulsified fat from intestinal lacteals and is collected and transported by the thoracic duct into the circulation. There are variations in the anatomy of thoracic duct, and based on the level of disruption, mostly unilateral chylous effusions develop [10]. The degree of injury and patient diet will dictate the rate at which fluid accumulates in the pleural space and as such there may be a variable latency period of 2 days to several weeks before a patient becomes symptomatic [2]. As mentioned before, in most cases chylothorax is associated with advanced lymphoma when lymph node masses are formed and causes obstruction of the thoracic duct or collaterals. However, chylothorax is an uncommon and poorly described complication [11,12].
Chylothorax occurring because of duct obstruction is almost exclusively left-sided. If right thoracic lymphatics are also obstructed, a right chylothorax may then accumulate [4]. Since bulky disease was not present in our patient’s newest CT scans, it seemed unlikely that separate lymph nodes could cause damage to a thoracic duct to such a degree. Possibly, the lymphomatous tissue had in fact infiltrated the duct, leading to its rigidity and injury during physical exertion, such as this patient presented after heavy box lifting. Following rupture of the duct, chyle leaks first into the mediastinum and then into the pleural cavity as the parietal pleura ruptures due to pressure caused by the mediastinal effusion [2]. The disruption of the duct had to be below the level of Th 5–6 to result in a right-sided effusion.
During MDD, the main point of discussion was, that due to nonprogressive lymphadenopathy and previous histological conclusion from a few years ago, the lymphoproliferative disease was unlikely; therefore, the decision was made to first employ less invasive procedures and manage chylothorax conservatively, before a potential lymph node extirpation. Looking back, if it was done in a timely manner, right when the patient first presented to the hospital, the final diagnosis would have come sooner. Also, the patient herself was presented with the options and agreed to this approach.
At present, there are no specific guidelines or universally accepted protocols for the treatment of chylothorax. That is largely due to numerous clinical factors unique to each patient, including etiology, symptoms, output of chyle per day, and other individual factors. In general, conservative treatment is tried first before more invasive measures are considered. In a conservative approach, mostly dietary modifications and drainage of the effusion are required. It is important to note that prolonged drainage can lead to immunocompromise, malnutrition, and electrolyte disturbances [8].
Dietary modifications (low-fat diet) can reduce the volume of chyle production and reduce the chyle flow in the thoracic duct, allowing a potential leak to heal. The effect of oral in-take on a chyle leak is unpredictable and may vary from patient to patient. In our patient it failed, and she was switched to total parenteral nutrition (TPN). In the meantime, she had to undergo multiple investigations to address and understand the underlying pathology. Approximately 43% of patients can be managed successfully with conservative therapy alone with no mortality [13]. TPN can meet patient needs and compensate for the energy and protein losses, and parenteral lipids are delivered directly into the blood stream and thus do not pass through the lymph system as chyle [14].
Our patient received 2 weeks of TPN and after it was discontinued, intercostal drainage significantly increased to >1100 ml per day (high-volume output), which finally led to the decision to perform VATS mediastinal lymph node dissection and thoracic duct clipping. Surgical ligation of the thoracic duct provides best results in cases of traumatic chylothorax with high-volume chyle leak, and the outcome of this modality is less certain in non-traumatic chylothorax patients. In the previous studies, overall success rates after thoracic duct ligation have ranged between 67% and 91% [15–17]. In the present case the chylothorax persisted after the surgical management, but the leak was low-output and could be managed with dietary modifications. This could be explained by the anatomy, as there are many lymphatic-venous communications as the thoracic duct ascends through the thorax and anastomoses between the duct and right posterior intercostal lymphatics. These communications allow collateral flow of lymph following surgical ligation of the thoracic duct and usually provide an alternative route of flow in situations of thoracic duct obstruction [18].
Histopathological, including immunohistochemical and morphological, examination finally revealed the main diagnosis of the patient – non-Hodgkin lymphoma. FL has a characteristic immunophenotype and B cell markers are expressed in the cell surface [19]. When our patient was first examined for lymphadenopathy, neck lymph node biopsy showed small follicles containing a well-formed germinal center, Ki67 <40%, CD20+, Bc12-, interfollicular zone containing heterogeneous population, B lymphocytes CD20+ (40%), T lymphocytes CD3+ (50–55%), and stromal edema, but no signs of lymphoproliferative disorder. The second time, lymphoproliferative disorder was always on the differential list, but due to long-standing history of lymphadenopathy with no progression over a 6-year period and previously normal histopathological finding, it was decided to perform many different tests before doing another lymph node excision biopsy. It took 6 courses of chemotherapy for the patient to be in full metabolic remission and for her chylothorax to fully resolve.
Conclusions
This clinical case highlights how challenging it sometimes can be to diagnose indolent lymphomas. Malignancy, especially lymphomas, are the main non-traumatic cause of chylothorax, which is generally a rare occurrence accounting for only a tiny portion of all pleural effusions. Patient presentation and certain features sometimes make a broad list of differential diagnoses and the correct diagnosis is reached only after a wide variety of investigations are performed. Successful treatment led to full metabolic remission and resolution of chylothorax.
Figures
References:
1.. Majdalany BS, Murrey DA, Kapoor BS: J Am Coll Radiol, 2017; 14; 118-26
2.. Rudrappa M, Paul M, Chylothorax: StatPearls. February 21, 2023, Treasure Island (FL), StatPearls Publishing Available from: URL: https://www.ncbi.nlm.nih.gov/books/NBK459206/
3.. Riley LE, Ataya A, Clinical approach and review of causes of a chylothorax.: Respir Med, 2019; 157; 7-13
4.. Schulman A, Fataar S, Dalrymple R, Tidbury I, The lymphographic anatomy of chylothorax: Br J Radiol, 1978; 51(606); 420-27
5.. Valentine VG, Raffin TA, The management of chylothorax: Chest, 1992; 102(2); 586-91
6.. Khanlari M, Chapman JR, Follicular lymphoma: Updates for pathologists.: J Pathol Transl Med., 2022; 56(1); 1-15
7.. Cholet C, Delalandre C, Monnier-Cholley L, Nontraumatic chylothorax: Nonenhanced MR lymphography.: Radiographics, 2020; 40; 1554-73
8.. Ur Rehman K, Sivakumar P, Non-traumatic chylothorax: Diagnostic and therapeutic strategies.: Breathe (Sheff)., 2022; 18(2); 210163
9.. Nair SK, Petko M, Hayward MP, Aetiology and management of chylothorax in adults.: Eur J Cardiothorac Surg, 2007; 32(2); 362-69
10.. Maldonado F, Cartin-Ceba R, Hawkins FJ, Medical and surgical management of chylothorax and associated outcomes: Am J Med Sci, 2010; 339; 314-18
11.. Freedman A, Jacobsen E, Follicular lymphoma: 2020 update on diagnosis and management.: Am J Hematol., 2020; 95(3); 316-27
12.. Kotze V, Van Schalwyk N, Medical Nutrition therapy for a patient presenting with a chylothorax.: S Afr J Clin Nutr, 2013; 26(3); 152-55
13.. Pulle MV, Puri HV, Asaf BB, Chylothorax – modalities of management and outcomes: A case series.: Lung India, 2021; 38(2); 154-60
14.. McCray S, Parish CR, When chyle leaks: Nutrition management options.: Practical Gastroenterology, 2004; 28(5); 60-76
15.. McGrath EE, Blades Z, Anderson PB, Chylothorax: Aetiology, diagnosis and therapeutic options.: Respir Med, 2010; 104(1); 1-8
16.. Akin H, Olcmen A, Isgorucu O, Approach to patients with chylothorax complicating pulmonary resection: Thorac Cardiovasc Surg, 2012; 60; 135-39
17.. Cerfolio RJ, Allen MS, Deschamps C, Postoperative chylothorax: J Thorac Cardiovasc Surg, 1996; 112(5); 1361-66
18.. Seaton A, Leitch AG, Seaton D: Crofton and Douglas’s respiratory diseases, 2000, Wiley Blackwell Chapter 43: Diseases of the pleura
19.. Filippo L, Claudio S, Giampietro M, David FM: Pleural diseases, 2022; 59-68, Elsevier Chapter 07 – Chylothorax Associated with Indolent Follicular Lymphoma
Figures
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943420
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942824
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250