11 July 2023: Articles 
Venous Thoracic Outlet Syndrome with an Upper Extremity Deep Vein Thrombosis Caused by a Dislocated Clavicle Fracture: A Case Report
Unusual clinical course
Yoshihiro Miyake12ABCDEF*, Tomohiro AbeDOI: 10.12659/AJCR.939250
Am J Case Rep 2023; 24:e939250
Abstract
BACKGROUND: Clavicle fractures are a relatively common injury, and are not problematic when occurring alone. Venous thoracic outlet syndrome (TOS) is generally caused by compression of the subclavian vein between the first rib and oblique muscles, and is often complicated by the presence of upper extremities deep vein thrombosis (UEDVT). Herein, we present a case of venous TOS complicated with UEDVT due to a dislocated clavicle fracture.
CASE REPORT: A 29-year-old man was injured in a motorcycle accident. The patient’s right clavicle was fractured, and the distal part of the fracture had dislocated into his right thorax. Contrast-enhanced computed tomography showed an obstruction of the subclavian vein by the dislocated clavicle and thrombus on the distal side of the obstruction. Anticoagulant therapy was not indicated because of other injuries, such as traumatic subarachnoid hemorrhage. No vena cava filter was placed in the superior vena cava owing to the relatively low volume of the thrombus. Alternatively, intermittent pneumatic compression to the right forearm was initiated. On day 6, surgical reduction of the clavicle was performed. The thrombus remained after the reduction. The patient received anticoagulation therapy with heparin followed by oral anticoagulants. The patient was discharged without any complications of UEDVT or bleeding.
CONCLUSIONS: Venous TOS with UEDVT caused by trauma is rare. Anticoagulation therapy, pneumatic limb compression, and vena cava filter placement should be considered according to the degree of the obstruction and other associated injuries.
Keywords: Anticoagulants, Clavicle, Fractures, Bone, Intermittent Pneumatic Compression Devices, thoracic outlet syndrome, Upper Extremity Deep Vein Thrombosis, Male, Humans, Adult, Vena Cava, Superior
Background
Upper extremities deep vein thrombosis (UEDVT) accounts for 5–10% of all deep vein thrombosis (DVT) [1], and is often caused by coagulation abnormalities such as malignancy, central venous catheterization, or pacemaker implantation [2]. Complications of UEDVT include pulmonary thromboembolism, phlegmasia cerulea dolens, and postthrombotic syndrome (PTS); anticoagulation is the mainstay of treatment for DVT [2].
In thoracic outlet syndrome (TOS), the nerves, subclavian artery, and subclavian vein are affected by compression of the neurovascular bundle crossing under the oblique muscle and over the first rib due to rib or muscle abnormalities or trauma [3]. Compression of the subclavian vein causes deep vein thrombi in the upper extremities [3,4]. Thus, decompression is crucial for treating TOS [3]. However, in cases complicated with UEDVT, there is concern that the release of compression may lead to pulmonary thromboembolism [1]. Therefore, the occurrence of TOS with UEDVT in cases involving multiple trauma is challenging because anticoagulation is often contraindicated.
We, herein, present a case with multiple trauma, including TOS involving the subclavian vein caused by a displaced fractured clavicle. Application of intermittent pneumatic compression successfully prevented the elongation of the thrombus despite the absence of anticoagulation before fracture reduction. This case highlights the difficulties in managing TOS complicated by UEDVT occurring in multiple trauma.
Case Report
A 29-year-old man was injured in a motorcycle crash. The patient had no previous history of thrombosis and was not taking any medications. There was no family history of thrombosis.
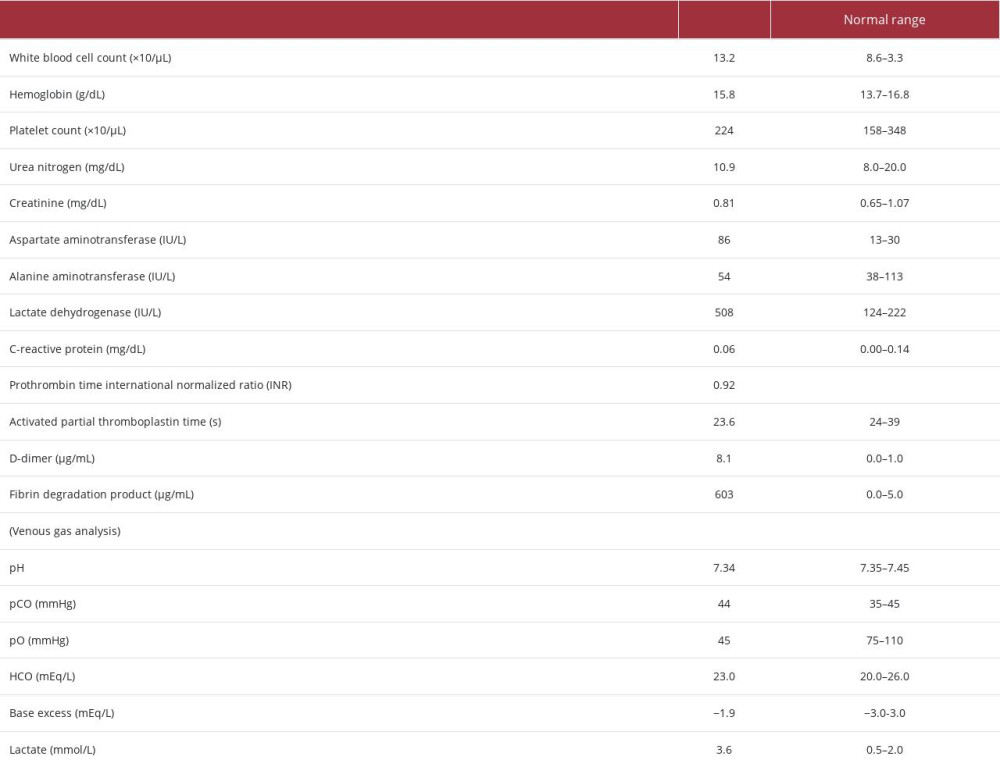
On his arrival, the patient had a level of consciousness of Glasgow Coma Scale 13 (E3V4M6), blood pressure of 110/80 mmHg, heart rate of 102 beats/min, respiratory rate of 16 breaths/min, and stable respiratory and circulatory status. The patient complained of pain in the nose, right upper chest, and left forearm. The left wrist was swollen and deformed. There was no swelling, skin color change, sensory disturbance, or motor palsy in the right upper extremity, indicating no blood flow disturbance. Chest X-ray showed a fractured right clavicle, with its distal fragment dislocated toward the thorax (Figure 1). A computed tomography (CT) scan of the chest showed that the distal portion of the right clavicle fracture had protruded into the thoracic cavity, compressing the right subclavian vein. Contrast-enhanced CT with contrast media injected from the affected limb showed a contrast defect (7×45 mm) in the subclavian vein distal to the compressed area, indicating a thrombus (Figure 2). The dorsal scapular vein, which branched from distal to the thrombus, drains blood from the right arm as a collateral vein. Other injuries, including traumatic subarachnoid hemorrhage, fractures of the left 6th–11th ribs, fracture of the distal end of the left radius, fracture of the nasal bone, and fracture of the mandible, were also diagnosed. Blood examination showed elevated levels of fibrin degradation products and D-dimer (Table 1).
Anticoagulants were not administered because of complications of traumatic subarachnoid hemorrhage and other injuries. As prophylaxis to protect against extension of the subclavian vein thrombus, fluid infusion from the right forearm with intermittent pneumatic compression was performed. We consulted with a cardiologist, interventional radiologist, cardiac surgeon, and pulmonary surgeon regarding the strategy for the reduction of the clavicle. Since the risk of fatal pulmonary thromboembolism was low because of the low thrombus volume (1.73 mL) and not all members of the medical team had sufficient experience with superior vena cava (SVC) filter placement, we decided to perform clavicle fracture repair without SVC filter placement. Instead, intraoperative backup arrangements were made to allow for surgery and catheter intervention in the event of pulmonary thromboembolism or pneumothorax.
On day 6, preoperative enhanced CT showed that the thrombus remained unchanged in size and location. We performed an open orthopedic fixation of the clavicle with the Kapandji technique and fixation with an intramedullary K-wired pin and tension band wiring. Because of the limited skin incision, the subclavian vein was not visible. There were no respiratory or circulatory changes during the reduction. Postoperative enhanced CT showed a residual thrombus in the subclavian vein (Figure 3). On the ninth day, the patient underwent an open reduction of the distal left radius fracture and an open fixation of the mandible fracture. On day 10, continuous administration of heparin was started at a dose of 12 000 units/day. On day 13, an enhanced CT revealed no significant change in the location or size of the thrombus in the subclavian vein. Heparin was changed to apixaban on day 14. The patient was discharged from the hospital on day 27. As the patient showed no symptoms, including a lack of pain and edema in the right upper extremity, the apixaban use was terminated after 6 months.
Discussion
Here, we present a case of multiple trauma, including venous TOS complicated by deep venous thrombus in the subclavian vein due to compression of the subclavian vein by a deviated clavicle fragment. Because of other injuries including traumatic brain injury, preoperative anticoagulation and thrombolytic therapy were not possible, and instead, intermittent pneumatic compression and extracellular fluid infusion from peripheral veins of the affected limb were performed. The thrombus remained in the subclavian vein both intraoperatively and postoperatively. The patient was treated with anticoagulant therapy during the chronic phase without any new recurrence of symptoms.
In this patient, venous compression and injury caused by the dislocated clavicular fracture caused the UEDVT. In other words, alteration of blood flow (venous stasis) and endothelial damage in the Virchow’s triad [5] contributed to the development of UEDVT. In general, anticoagulation therapy is indicated for DVT, although it was not possible in the acute phase of this case because of multiple trauma, including traumatic brain injury. Therefore, instead of anticoagulant therapy, we performed preoperative pneumatic limb compression on the affected limb to prevent thrombus elongation.
Pneumatic limb compression inhibits thrombus growth by facilitating and maintaining venous blood flow [6]. In general, pneumatic limb compression is contraindicated in the presence of an existing DVT, as it can fragment and sweep away the thrombus [6]. In the present case, the risk of UEDVT migration was low preoperatively because the dislocated clavicle fragment blocked the proximal side of the subclavian vein. Pneumatic limb compression would therefore be expected to be effective in preventing occlusion of the collateral blood vessel that branched from the distal side of the thrombus by inhibiting thrombus elongation to the distal side. The indication for intermittent pneumatic compression should be considered based on the degree and location of the subclavian vein obstruction in each case.
Preoperative SVC filter placement was not performed in this case. DVT is classified as acute (<2 weeks), subacute (from 2 weeks to 6 months), or chronic (>6 months); importantly, acute DVT has more characteristics of migration than the others [7]. This case was suitable for filter placement perioperatively because the indications for inferior vena cava (IVC) filter placement in lower extremity DVT are in patients with proximal DVT and contraindications to anticoagulant therapy [8,9]. However, the incidence of pulmonary thromboembolism due to upper extremity DVT is at most 9%, which is lower than that of lower extremity DVT, and the incidence of fatal pulmonary thromboembolism is extremely rare [1,10]. According to the report regarding the thrombus volume and the location of the occluding pulmonary artery [11], the thrombus volume of this case (approximately 1.73 mL) is unlikely to occlude the main trunk of the pulmonary artery. Therefore, the risk of a fatal outcome would be low even if pulmonary thromboembolism had occurred in this case and the SVC filter would have been less effective in the acute phase.
In the present case, thrombolytic therapy was not performed in the acute phase. Residual thrombus is associated with the development of PTS [12]. Among lower extremities DVT, thrombolytic therapy should be considered only for patients with symptomatic proximal DVT at low bleeding risk and patients with limb-threatening proximal DVT [8]. In upper extremity DVT, about 15% develop PTS [13]. A previous meta-analysis suggested that thrombolytic therapy lowers the risk of PTS [14]. However, in 2 randomized clinical trials of proximal venous DVT of a lower extremity, there was no difference in the incidence of PTS between the usual treatment group and the PTS group [15,16]. Further investigation is needed on whether thrombolytic therapy in upper extremity DVT can reduce the development of PTS.
The patient was anticoagulated with apixaban for 6 months. In the chronic phase, anticoagulation therapy for DVT for at least 3 months is recommended [8]. From the point of view of managing anticoagulation and bleeding complications, a direct oral anticoagulant is recommended over warfarin as anticoagulation therapy [17]. In the present case, there were no findings of underlying thrombogenic disease and well-developed collateral blood vessels, indicating a low risk of thrombus elongation and obstruction of the collateral veins. Thus, we were able to terminate anticoagulant therapy after 6 months.
Similar to the present case, there is a case report of UEDVT in which the patient died from pulmonary thromboembolism caused by an upper extremity embolus that was as large as the one presented in our case (11×45 mm) [18]. Therefore, it may be better to consider perioperative SVC filter placement before the reduction, especially in the case of large thrombus volume. However, the use of SVC filters has not been approved and is not common in many countries, including in Japan. There is a case report of an IVC filter placed in the SVC for upper extremity DVT, as an alternative [19]. SVC filter placement is controversial as fatal complications occur in approximately 4% of cases with SVC filters [10].
Adaptation of each treatment of TOS with UEDVT should be determined on a case-by-case basis because the etiology, location, concomitant pathology, and degree of complications are variable. Since TOS with UEDVT is relatively infrequent, accumulation of cases and future studies are warranted to elucidate the effectiveness of treatments, including pneumatic limb compression, SVC filter placement, and thrombolytic therapy, and to evaluate their relationship with PTS.
Conclusions
We present a case of DVT in the subclavian vein immediately after an injury due to venous TOS caused by a dislocated clavicle fracture. In patients with acute UEDVT, pneumatic limb compression, anticoagulation, thrombolytic therapy, and SVC filter placement should be considered based on venous obstruction, treatment, and other complicating injuries.
Figures
References:
1.. Muñoz FJ, Mismetti P, Poggio R, Clinical outcome of patients with upper-extremity deep vein thrombosis: Results from the RIETE Registry: Chest, 2008; 133; 143-48
2.. Kucher N, Clinical practice. Deep-vein thrombosis of the upper extremities.: N Engl J Med, 2011; 364; 861-69
3.. Cavanna AC, Giovanis A, Daley A, Thoracic outlet syndrome: A review for the primary care provider: J Osteopath Med, 2022; 122; 587-99
4.. Hood DB, Kuehne J, Yellin AE, Weaver FA, Vascular complications of thoracic outlet syndrome: Am Surg, 1997; 63; 913-17
5.. Kushner A, West WP, Khan Suheb MZ, Pillarisetty LS, Virchow triad.: StatPearls [Internet]., 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539697/
6.. Auguste KI, Quiñones-Hinojosa A, Berger MS, Efficacy of mechanical prophylaxis for venous thromboembolism in patients with brain tumors: Neurosurg Focus, 2004; 17; E3
7.. Gornik HL, Sharma AM, Duplex ultrasound in the diagnosis of lower-extremity deep venous thrombosis: Circulation, 2014; 129; 917-21
8.. Ortel TL, Neumann I, Ageno W, American Society of Hematology 2020 guidelines for management of venous thromboembolism: Treatment of deep vein thrombosis and pulmonary embolism.: Blood Adv., 2020k4; 19; 4693-738
9.. Kearon C, Akl EA, Comerota AJ: Chest., 2012; 141(2 Suppl.); e419S-96S
10.. Owens CA, Bui JT, Knuttinen MG, Pulmonary embolism from upper extremity deep vein thrombosis and the role of superior vena cava filters: A review of the literature.: J Vasc Interv Radiol, 2010; 21; 779-87
11.. Furlan A, Aghayev A, Chang CC, Short-term mortality in acute pulmonary embolism: Clot burden and signs of right heart dysfunction at CT pulmonary angiography: Radiology, 2012; 265; 283-93
12.. Prandoni P, Frulla M, Sartor D, Vein abnormalities and the post-thrombotic syndrome: J Thromb Haemost, 2005; 3; 401-2
13.. Berliner E, Ozbilgin B, Zarin DA, A systematic review of pneumatic compression for treatment of chronic venous insufficiency and venous ulcers: J Vasc Surg, 2003; 37; 539-44
14.. Watson L, Broderick C, Armon MP, Thrombolysis for acute deep vein thrombosis.: Cochrane Database Syst Rev., 2016; 11; CD002783
15.. Vedantham S, Goldhaber SZ, Julian JA, Pharmacomechanical catheter-directed thrombolysis for deep-vein thrombosis: N Engl J Med, 2017; 377; 2240-52
16.. Notten P, de Smet AAEA, Tick LW, CAVA (ultrasound-accelerated cath-eter-directed thrombolysis on preventing post-thrombotic syndrome) trial: Long-term follow-up results.: J Am Heart Assoc., 2021; 10; e018973
17.. Weycker D, Wygant GD, Guo JD, Bleeding and recurrent VTE with apix-aban vs warfarin as outpatient treatment: Time-course and subgroup analyses.: Blood Adv., 2020; 4; 432-39
18.. Li Y, Wang Z, Sang X, Subclavian vein thrombosis and fatal pulmonary embolism after proximal humerus fracture surgery.: J Orthop Surg (Hong Kong), 2019; 27 2309499019832728
19.. De Oliveira Leite TF, Silva TOE, Pereira OI, Carnevale FC, Retrievable celect™ filter placement in the superior vena cava: A case report.: Int J Surg Case Rep., 2020; 73; 105-8
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250