29 June 2023: Articles 
Endometrial Adenocarcinoma with Discordant Microsatellite Stability Status Treated with First-Line Pembrolizumab: A Case Report and Narrative Review
Unusual clinical course, Challenging differential diagnosis, Unusual or unexpected effect of treatment, Rare coexistence of disease or pathology
Christopher R. Grant1ABCDEF*, Elaine J. Chiao1EF, Zhaohui L. Arter2ADE, Cary Johnson3C, Truc Tran3BE, Farshid Dayyani2E, Krishnasu Tewari2E, Valery Vilchez4E, Joseph CarmichaelDOI: 10.12659/AJCR.939448
Am J Case Rep 2023; 24:e939448
Abstract
BACKGROUND: Microsatellite instability (MSI) is a hallmark of specific cancers and can be diagnosed using both tissue- and liquid-based approaches. When these tissue- and liquid-based approaches give differing results, they are known as discordant or being at variance. MSI-H tumors are well-researched candidates for treatment with programmed cell death protein 1 (PD-1) inhibitor-based immunotherapy, but the efficacy of immunotherapy in MSI-H discordant endometrial cancer, especially as first-line therapy, is not yet well documented in the literature.
CASE REPORT: A 67-year-old woman presented with a retroperitoneal mass positive for recurrent adenocarcinoma of endometrial origin. Her stage I endometrial adenocarcinoma 7 years ago demonstrated microsatellite stable (MSS) by immunohistochemical (IHC) stain and indeterminant due to insufficient tissue by Caris Next-Generation Sequencing (NGS). She then presented with a retroperitoneal mass that was MSI-H on IHC stain and Caris NGS, as well as MSI high on liquid biopsy @Guardant360 (@G360). The patient proceeded with pembrolizumab treatment 1 year ago and has sustained a complete clinical response at the time of writing.
CONCLUSIONS: Our case provides further evidence for the need to retest the microsatellite stability of metastatic sites, especially after a long disease-free survival. Here, we providing a literature review of case reports and a review of studies outlining discordance of testing modalities. Our case also highlights the importance of considering the use of immunotherapy as a first-line agent in patients who may have a poor ECOG performance status, as it can significantly improve their quality of life and reduce the number of adverse effects compared to chemotherapy.
Keywords: Endometrial Neoplasms, Immune Checkpoint Inhibitors, Immunotherapy, microsatellite instability, Pembrolizumab, Female, Humans, Aged, Quality of Life, Neoplasm Recurrence, Local, Microsatellite Repeats, Adenocarcinoma
Background
Microsatellites are highly abundant repeated sequences of 1–6 nucleotides with a wide distribution pattern in the genome [1,2]. Although most MS tandem repeats are located near chromosome ends within the coding region, they may also be found in introns and other non-coding regions. The literature suggests that microsatellite sequences are generated when DNA slippage or mismatch occurs during the process of replication, resulting in 1 or more repeat or deletion sequences. In tumor cells with a deficient mismatch repair (dMMR) system, an intrinsic cellular machinery that corrects such DNA replication errors, microsatellite mutations can serve as a trigger for subsequent cancer development and tumorigenesis [1–3].
There are 2 main classifications of MSI: high microsatellite instability (MSI-H) and microsatellite stability (MSS). MSI-H associated dMMR has been well-delineated in several types of human cancers and has further been shown to be an indicator for both disease prediction and prognosis [1,2]. Approximately 15% of colorectal adenocarcinomas display MSI-H as a result of MLH-1 gene promotor methylation or germline mutations in the MLH-1 or MLH-2 genes [4–6]. We see this in endometrial carcinoma as well with subclonal MLH1 promoter MLH-1 loss and MSI correlating with MMR deficient status [7]. A 2017 study using an MSI-calling software, MANTIS, explored the landscape of MSI across an expanded number of cancer types and identified MSI in 27 tumor types, including cancers that have not been well-researched in the context of MSI [8].
The criterion standard for identifying MSI-related cancers is polymerase chain reaction (PCR) and immunohistochemistry (IHC), while liquid biopsy approaches have emerged in recent years as potent alternatives or confirmatory screening tools [3,6]. A molecular approach with PCR presents the advantage of studying the molecular system based upon the dysfunction and is not limited to protein expression to allow point mutations to be identified. This means that some point mutations can allow MMR protein expression without having an MSI status [9]. However, IHC has many benefits, such as easier preparation and less expense [9]. IHC demonstrates the protein expression, so it may not always detect an MMR system deficiency. This can cause a discordance, or a discrepancy, between IHC and PCR analysis, as demonstrated in many studies. For instance, studies on the rate of discordance between MMR IHC and MSI-PCR testing in colorectal cancer has shown a range from 1% to 10% of samples [9]. This range is significant and makes it difficult for oncologists to select an ideal method to evaluate tumors MSS status, as many oncologists choose to pursue both options of testing, which provides a burden on selecting the ideal approach to treating patients with discordant results. With this, there is a gap in knowledge, necessitating an essential review to further compare completed studies on discordance and provide insight on whether to utilize IHC or PCR analysis when assessing MSS status. The aim of this review is to provide a synthesized overview highlighting landmark studies to guide oncologists in selecting a treatment plan when discordant diagnostic results arise to assist in the development of conceptual frameworks to reconcile past, current, and future research.
Conventional chemotherapy has historically been used for dMMR/MSI-H solid tumors; however, recent clinical trials have demonstrated that immunotherapy elicits a stronger and more clinically favorable response in these patients. In the KEYNOTE-177 trial, patients treated with the PD-1 inhibitor pembrolizumab as a first-line treatment experienced fewer adverse effects and significantly longer progression-free survival than patients treated with chemotherapy for MSI-H or dMMR metastatic colorectal cancer [5]. We have seen the blockade of the immune checkpoints in solid malignancies such as lung and renal cancers and melanoma and studies have demonstrated up-regulation of the pathway in endometrial cancer, leading us to believe that there is a rationale for testing PD-1/PD-L1 status in endometrial carcinoma [10]. Even in patients with MSS, we have seen clinical benefit in longer progression-free survival and overall survival when compared to chemotherapy among patients with advanced endometrial cancer when using lenvatinib with pembrolizumab [11]. In this paper, we report the post-treatment outcomes involving a case of endometrial adenocarcinoma with discordant MSI status in a patient who achieved clinical complete response with front-line pembrolizumab.
Case Report
INITIAL PRESENTATION:
A 67-year-old woman with a history of endometrial adenocarcinoma initial stage 1B diagnosed 7 years ago, status post total abdominal hysterectomy with bilateral salpingo-oophorectomy presented to the emergency department with intractable nausea and vomiting that had started 2 days prior. She was previously able to tolerate a diet, had been having normal brown-colored stools, denied any itching of the palms, significant weight loss, fevers or chills, abdominal pain, or yellowing of the skin or eyes. She denied any alcohol use, smoking, or drug use. She lived at home and was previously independent and able to cook for herself, do laundry, and walk up a flight of stairs. Her family history was not notable for any pancreatic cancer, endometrial cancers, or ovarian cancers. Her physical exam was notable for some mild tenderness in the epigastric region with deep palpation, positive bowel sounds, and no findings of scleral icterus or jaundice. She had computed tomography (CT) scans of the abdomen and pelvis, which demonstrated a 25×17 mm retroperitoneal mass posterior to the third portion of the duodenum, partial duodenal obstruction, invasion of left renal vein, inferior vena cava, and abdominal aorta (Figure 1A, 1B). During this hospitalization, she developed paroxysmal atrial fibrillation and congestive heart failure with a reduced ejection fraction of 20%.
CANCER HISTORY:
Her previous endometrial adenocarcinoma that was diagnosed 7 years ago was moderately differentiated and extended in the outer half of the myometrium without involvement of the cervix. She had a total abdominal hysterectomy performed, without evidence of regional invasion and was found to have a nonspecific reactive 0.9-cm external iliac lymph node that was characterized as nonspecific. Her pathology was given a FIGO grade 2 with MSS by IHC and indeterminant by Caris NGS (Table 1). She did not receive any adjuvant therapy and was being actively surveilled with imaging.
INITIAL WORK-UP:
During the current hospitalization, she had a stent placed in her duodenum. A fine-needle aspiration biopsy obtained from the mass revealed adenocarcinoma with presence of PAX 8, ER, CK7, and CK17, concerning for primary gynecologic cancer. Her tumor profiling from her retroperitoneal nodes demonstrated MSI-H by IHC and Caris NGS, and circulating DNA was found at the time of recurrence by @G360 and showed MSI-H (Table 1). She later had a positron emission tomography (PET)-CT scan demonstrating localization in the retroperitoneum with no suspicious activity in neck, chest, or pelvis, without enlarged pelvic or inguinal lymph nodes. Her residual disease by Signatera was 8.73 MTM/mL (Figure 2). Her tumor markers were notable for carcinoembryonic antigen (CEA) level of 75.9, carbohydrate antigen-125 (CA-125) level of 186, and cancer antigen 19-9 (CA19-9) of 360. Her case was discussed at a multidisciplinary tumor board, and it was believed that her tumor was not resectable due to the major vascular and duodenal invasion, but that she was a candidate for immunotherapy. Since she had congestive heart failure and numerous medical comorbidities, first-line chemotherapy with a platinum-based chemotherapy was not an option that we felt she was able to tolerate.
TREATMENT AND FOLLOW-UP:
Due to the MSI-H status of the recurrent retroperitoneal node and MSS at the primary site, she was started on pembrolizumab 400 mg every 6 weeks, as well as lenvatinib 12 mg to cover possible heterogeneity of both diseases. Lenvatinib was discontinued after 1 week due to nausea and vomiting, as well as musculoskeletal pains. Subsequent imaging after 3 months of treatment demonstrated an interval decrease in size of the retroperitoneal mass of 23×7 mm and normalization of previously elevated tumor markers with CEA level of 1.6, CA-125 level of 5, and CA19-9 of 11 (Figure 3). A repeat Signatera test demonstrated residual disease level of 0 MTM/mL (Figure 2). She was continued on pembrolizumab 200 mg every 3 weeks due to rash from high-dose pembrolizumab. The imaging at 6 months continue to show an interval decrease in her retroperitoneal mass, measuring 21×7 mm.
She had a repeat EGD after 8 months of treatment, which demonstrated no visualized mass on examination. Pembrolizumab was discontinued and she was surveilled with tumor markers and imaging every 3 months. She has since sustained complete clinical response for 10 months at the time of this report. A timeline of her case report is listed in Figure 4.
Discussion
MSS STATUS AMBIGUITY:
The detection of MSI-H status in patients with any solid tumor, including endometrial adenocarcinoma, is a crucial step in intervening with immune checkpoint inhibitors. The present case highlights the clinical ambiguity of MSI-H screening tools and tumor characteristics, given the discordant MSI-H results between the patient’s IHC, tissue NGS, and G360 tests, as well as similarly discordant results between her biopsies at baseline and recurrence (Table 1). This case is unique in that is the first ever report of a patient able to obtain a complete clinical response in an endometrial cancer with discordant microsatellite stability, especially in an individual who had recurrence after surgical treatment. These discordances can be seen in a variety of cases. Most notably, a recent study by Orellana et al demonstrated that 12% of patients with recurrent uterine cancer demonstrated clonal evolution in their MMR-D status, indicating a need for retesting the MMR status in patients with recurrent endometrial adenocarcinoma [12].
NARRATIVE REVIEW: CASE REPORTS WITH DISCORDANT MSS STATUS:
To further understand this case, a review of the medical literature was performed to discover case reports (Table 2) pertaining to the discordance of a primary carcinoma and metastasis, primary carcinoma, and recurrence, as well as treatment with immune checkpoint inhibitors in patients with discordant MSI status [13–16]. We performed a thorough search for case reports with discordance using the databases PubMed and Google Scholar. The following search terms were used in the literature search: “endometrial adenocarcinoma,” “discordance,” “microsatellite stability,” “immunotherapy,” and “microsatellite instability.” This brief review only included case reports published in English. Of the cases that were reviewed, all had received chemotherapy treatment before, and all had a population of recurrence that was rebiopsied, similar to our case. After the recurrence, 75% of the patients received treatment with pembrolizumab. Two cases with a metastasis that was microsatellite-stable demonstrated a partial response. One case with MSI-H status in the primary tumor and metastasis obtained no response; possibly due to a subclonal population of the tumor that may have had IHC staining expression, but in fact was nonfunctional and thus was nonresponsive. Most like our case is the report by Zheng et al, in which a patient with a primary MSS esophageal adenocarcinoma that was MSS had an MSI-H bony metastasis treated with pembrolizumab, resulting in a complete response [16]. We suspect this case had a similar genetic profile as ours, with a subclonal population that had progressive spread, but had a functional protein pathway that was able to be targeted with immune checkpoint inhibitors.
THEORIES OF DISCORDANCE:
There are many theories on why discordance is observed. First, intratumor heterogeneity plays a significant role and has been shown to demonstrate focal IHC staining [4,17]. In our patient, this could have been the cause of her discordance in testing as she could have had an intratumor subset population of cancer cells that was more predisposed to grow. This can be due to MMR IHC stains being reported in a dichotomous manner as “intact” or “lost.” “Lost” is described as cases where there is a complete absence of staining in the tumor epithelium, with the surrounding stroma as a positive internal control. Despite this, up to 7.2% of endometrial carcinoma samples have subclonal loss of the MMR protein expression, which does not fit this dichotomous reporting system [18]. Second, IHC staining can depict MSS, in which it is identified that the protein is present, although it does not necessarily mean the protein is functional. NGS can depict whether a protein is functional or not. In our case, we may have seen a protein being expressed in the primary endometrial carcinoma, but the functionality of the protein was ineffective due to methylation. Given that the NGS of the primary endometrial tissue did not have a sufficient quantity, the protein could have been nonfunctional. Third, pre-analytical difficulties with immunostaining could play a potential role, as the fixation of specific samples can vary and using a protocol standardized fixation is key to prevention of discordance [19]. This is less likely in our case, as we would expect to see MSI in the primary endometrial tissue, whereas the primary endometrial issue demonstrated MSS.
NARRATIVE REVIEW: STUDIES EVALUATING DISCORDANT MSS STATUS:
A brief narrative review was used to provide an overview highlighting landmark studies to guide providers in selecting a treatment plan when discordant diagnostic results arise. This review was conducted using the databases PubMed and Google Scholar. The following search terms were used in the literature search: “endometrial adenocarcinoma”, “discordance,” “micro-satellite stability,” “immunotherapy,” “checkpoint inhibitors”, and “microsatellite instability.” This brief review only included articles and abstracts that were published in English.
Further analyzation on the various studies evaluating discordances between the methods of IHC and PCR or NGS was more limited (Table 3). It was also difficult to compare studies, as the individuals evaluating the tests, location of population, and type of cancer were vastly different. The rate of discordance between samples varied from 1.0% to 15.7% [17,20–28], and 70% of these studies consisted of retrospective cohort studies with large sample sizes ranging from 92 to 8229. There are several key takeaway points from the narrative review. First, it is important to highlight Amemiya et al in particular because MSI-PCR and IHC staining were obtained from 284 patients across 14 various cancer types and found that 3 cases demonstrated a “mosaic” pattern of heterogeneity [23]. They found that IHC was still able to detect the heterogenous status while MSI-PCR had ambiguous results, which is potentially what could have been detected in our sample from the primary Caris NGS from the primary tumor, resulting in an inadequate sample quantity to perform testing. With their results, they believe that IHC demonstrated more favorable utility, as it will demonstrate the expression for mosaic cases [23]. Additionally, most of the studies aimed to assess the validity of using PCR compared to IHC. Several studies favored dual testing, as their rate of discordance was high [20,26,28]. Uniquely, Park et al had the largest sample size and the lowest discordance rate, possibly due to the statistical power in the study and likely means that with dual testing, most cases will remain concordant [26]. Discordance rates may be low, but can have major consequences at the individual level for patients. In the event that there is a discordant case, some studies recommended retesting [24,29]. In Guyot D’Asinieres et al, repeated reading of testing found only 0.4% of cases remained discordant [29]. They believe these cases were due to methylation and lack of protein expression in the IHC staining causing the mismatch, creating inactive mutant proteins that are still detected as positive. After reviewing these studies, we recommend dual testing with IHC and PCR to assess microsatellite stability because the low discordance rates were associated with large sample sizes in the various studies. We also recommend retesting additional metastases, and if there is a discordance between testing, performing repeat testing to ensure appropriate treatment is delivered to each patient to help further reduce the incidence of true discordant results. Lastly, further research is needed to evaluate discordance results that remain after retesting.
CONSIDERATION OF FIRST-LINE AGENT WITH POOR ECOG:
Traditionally, metastatic endometrial carcinoma is treated with first-line chemotherapy consisting of carboplatin and paclitaxel [30]. Given our patient’s significant comorbidities, including paroxysmal atrial fibrillation and congestive heart failure with a reduced ejection fraction of 20%, as well as a poor ECOG performance status of 2, the decision was made to treat her with pembrolizumab as a first line. Numerous studies have demonstrated that treatment of advanced solid-organ malignancies with immunotherapy compared with traditional chemotherapy is associated with a lower risk of adverse effects [31–33]. Pembrolizumab has been shown to improve patient quality of life for many solid-organ malignancies [31,34,35]. Our patient stated that she has had a significant improvement in her quality of life, she is able to eat again without problems, and denies any pain at her routine visits, in addition to her complete response from pembrolizumab. With this in mind, it is important to consider the use of immunotherapy as a first-line treatment in patients with a poor ECOG performance status.
STRENGTHS, LIMITATIONS, AND FUTURE DIRECTIONS:
Our case report shows the importance of retesting additional metastases and recurrences after treatment if there is concern about microsatellite instability for treatment with immunotherapy. This also highlights the importance of considering use of immunotherapy in individuals with a poor ECOG as a first-line agent, given the success in our patient. Our review article gives insight to oncologists on how to utilize data such as MSS status obtained with IHC and PCR analysis to encourage an evidence-based approach when determining if a patient can benefit from immune checkpoint inhibitor therapy. Despite these strengths of the study, there are limitations in that this is a case report of 1 patient rather, not a cohort or clinical study. Further ambiguity exists in discordant results of MSS status and highlights the need for clinical trials or larger observational studies of individuals with discordant MSS status. In addition, numerous studies have demonstrated additional viable diagnostic markers that could have a role in predicting the stage of endometrial cancer. For instance, in a study of tissue samples and whole blood from 30 patients, Oplawski et al found that miR-144, miR-106a, and miR-30d were potential diagnostic markers [36].
Conclusions
To the best of our knowledge, this study is the first to report treatment of endometrial adenocarcinoma in a patient with discordant MSI-H status who achieved complete response with first-line pembrolizumab. Our case highlights many key points. First, there are many factors that could cause discrepancies in microsatellite testing. This is highlighted throughout numerous case reports and studies in addition to ours. Our case provides further evidence for the need to retest the microsatellite stability of metastatic sites, especially after a long period of disease-free survival. Our case also highlights the importance of considering the use of immunotherapy as a first-line agent in patients who have a poor ECOG performance status, as it can significantly improve their quality of life and reduce the number of adverse effects compared to chemotherapy.
Figures
Tables
Table 1.. Immunohistochemical stain and next-generation sequencing for microsatellite instability.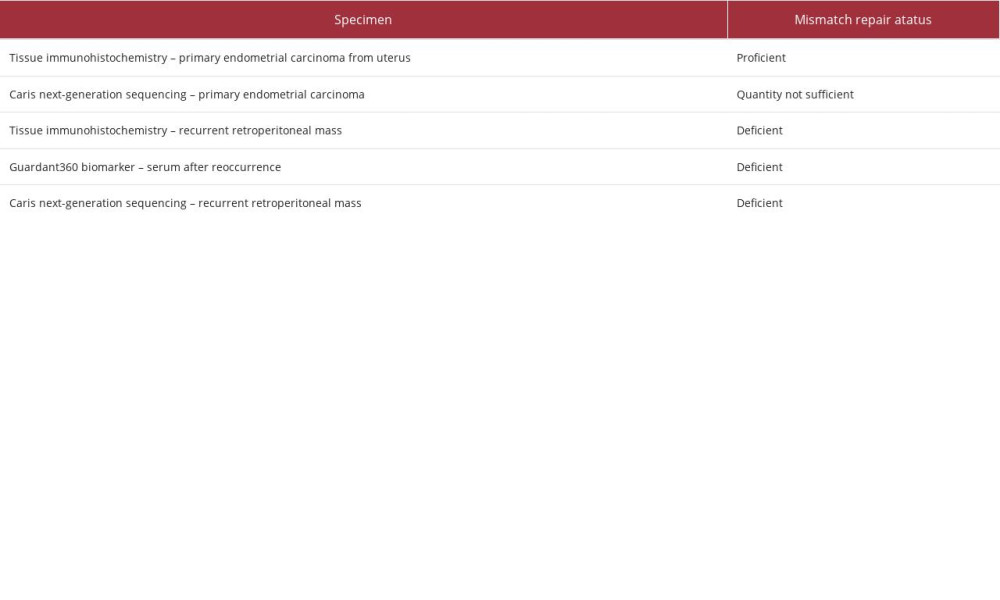 Table 2.. Case reports regarding discordance between primary and recurrent/metastatic carcinoma.
Table 2.. Case reports regarding discordance between primary and recurrent/metastatic carcinoma.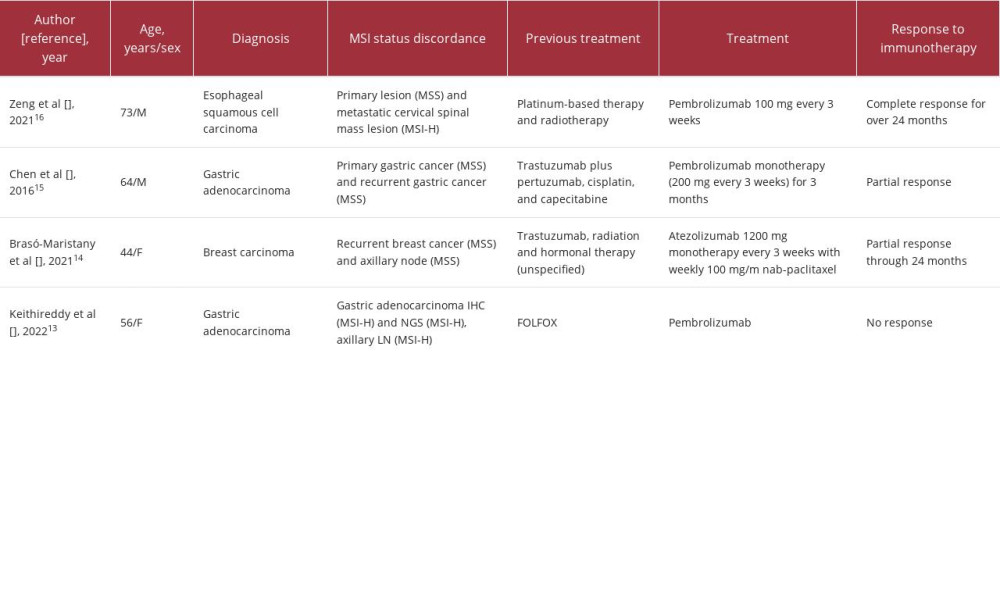 Table 3.. Studies regarding discordance of Immunohistochemistry and PCR/Next-Generation Sequencing in various carcinomas.
Table 3.. Studies regarding discordance of Immunohistochemistry and PCR/Next-Generation Sequencing in various carcinomas.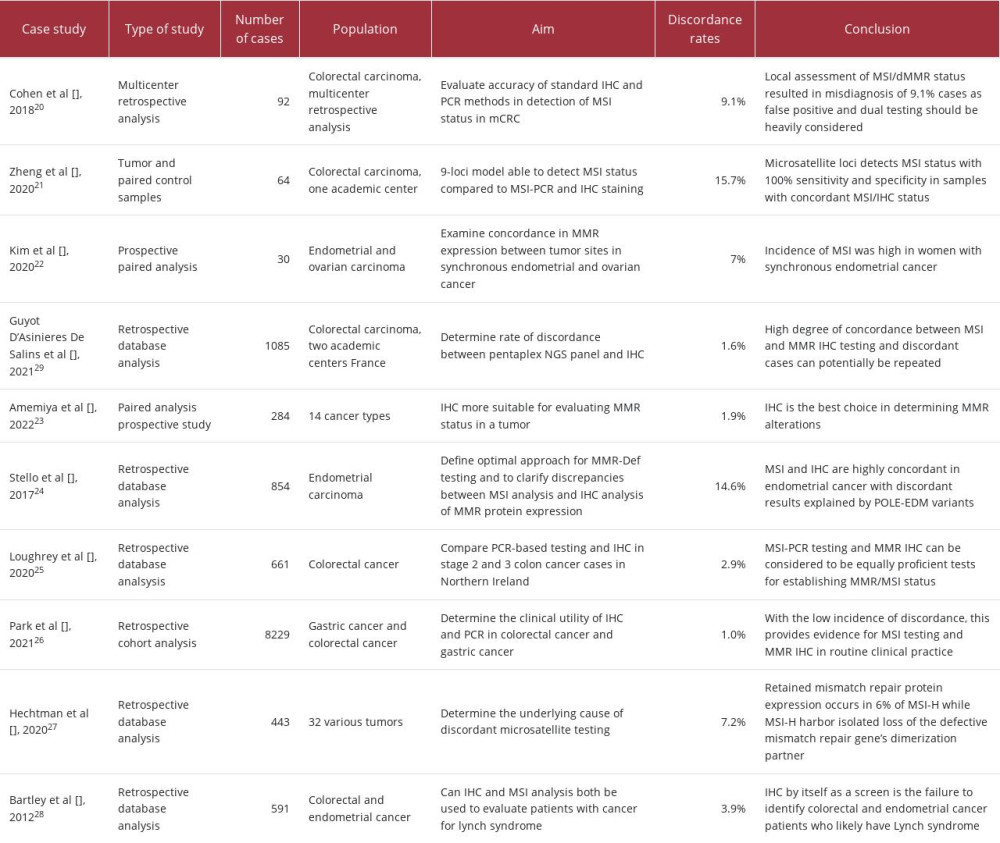
References:
1.. Li K, Luo H, Huang L, Microsatellite instability: A review of what the oncologist should know: Cancer Cell Int, 2020; 20; 16
2.. Woerner SM, Kloor M, von Knebel Doeberitz M, Gebert JF, Microsatellite instability in the development of DNA mismatch repair deficient tumors: Cancer Biomark, 2006; 2(1–2); 69-86
3.. Chakrabarti S, Bucheit L, Starr JS, Detection of microsatellite instability-high (MSI-H) by liquid biopsy predicts robust and durable response to immunotherapy in patients with pancreatic cancer: J Immunother Cancer, 2022; 10(6); e004485
4.. Gatalica Z, Vranic S, Xiu J, High microsatellite instability (MSI-H) colorectal carcinoma: A brief review of predictive biomarkers in the era of personalized medicine: Fam Cancer, 2016; 15(3); 405-12
5.. André T, Shiu KK, Kim TW, Pembrolizumab in microsatellite-instability-high advanced colorectal cancer: N Engl J Med, 2020; 383(23); 2207-18
6.. Rigau V, Sebbagh N, Olschwang S, Microsatellite instability in colorectal carcinoma. The comparison of immunohistochemistry and molecular biology suggests a role for hMSH6 [correction of hMLH6] immunostaining.: Arch Pathol Lab Med, 2003; 127(6); 694-700
7.. Soslow RA, Wethington SL, Cesari M, Clinicopathologic analysis of matched primary and recurrent endometrial carcinoma: Am J Surg Pathol, 2012; 36(12); 1771-81
8.. Bonneville R, Krook MA, Kautto EA, Landscape of microsatellite instability across 39 cancer types.: JCO Precis Oncol., 2017; 2017 PO.17.00073
9.. Evrard C, Tachon G, Randrian V, Microsatellite instability: Diagnosis, heterogeneity, discordance, and clinical impact in colorectal cancer: Cancers (Basel), 2019; 11(10); 1567
10.. Gargiulo P, Della Pepa C, Berardi S, Tumor genotype and immune microenvironment in POLE-ultramutated and MSI-hypermutated endometrial cancers: New candidates for checkpoint blockade immunotherapy?: Cancer Treat Rev, 2016; 48; 61-68
11.. Makker V, Colombo N, Casado Herráez A, Lenvatinib plus pembrolizumab for advanced endometrial cancer: N Engl J Med, 2022; 386(5); 437-48
12.. Spinosa D, Wong J, Whitaker R, To test or re-test, that is the question: comparison of the mismatch repair deficiency between primary and recurrent sites of uterine cancers: Gynecol Oncol, 2022; 166(1); S60
13.. Kethireddy N, Arvanitis L, LoBello J, A case report of immunotherapy-resistant MSI-H gastric cancer with significant intrapatient tumoral heterogeneity characterized by histologic dedifferentiation: J Clin Med, 2022; 11(12); 3413
14.. Brasó-Maristany F, Sansó M, Chic N, Case report: A case study documenting the activity of atezolizumab in a PD-L1-negative triple-negative breast cancer: Front Oncol, 2021; 11; 710596
15.. Chen KH, Yuan CT, Tseng LH, Case report: mismatch repair proficiency and microsatellite stability in gastric cancer may not predict programmed death-1 blockade resistance: J Hematol Oncol, 2016; 9; 29
16.. Zeng T, Zhang L, Chen C, Durable complete response to pembrolizumab in esophageal squamous cell carcinoma with divergent microsatellite status: A case report: Front Oncol, 2021; 11; 767957
17.. Boutin M, Gill S, Controversies and management of deficient mismatch repair gastrointestinal cancers in the neoadjuvant setting: Ther Adv Med Oncol, 2023; 15 17588359231162577
18.. Watkins JC, Nucci MR, Ritterhouse LL, Unusual mismatch repair immunohistochemical patterns in endometrial carcinoma: Am J Surg Pathol, 2016; 40(7); 909-16
19.. Shia J, Immunohistochemistry versus microsatellite instability testing for screening colorectal cancer patients at risk for hereditary nonpolyposis colorectal cancer syndrome. Part I. The utility of immunohistochemistry.: J Mol Diagn, 2008; 10(4); 293-300
20.. Cohen R, Hain E, Buhard O, Association of primary resistance to immune checkpoint inhibitors in metastatic colorectal cancer with misdiagnosis of microsatellite instability or mismatch repair deficiency status: JAMA Oncol, 2019; 5(4); 551-55
21.. Zheng K, Wan H, Zhang J, A novel NGS-based microsatellite instability (MSI) status classifier with 9 loci for colorectal cancer patients: J Transl Med, 2020; 18(1); 215
22.. Kim SR, Tone A, Kim R, Tumor site discordance in mismatch repair deficiency in synchronous endometrial and ovarian cancers: Int J Gynecol Cancer, 2020; 30(12); 1951-58
23.. Amemiya K, Hirotsu Y, Nagakubo Y, Simple IHC reveals complex MMR alternations than PCR assays: Validation by LCM and next-generation sequencing: Cancer Med, 2022; 11(23); 4479-90
24.. Stelloo E, Jansen AML, Osse EM, Practical guidance for mismatch repair-deficiency testing in endometrial cancer: Ann Oncol, 2017; 28(1); 96-102
25.. Loughrey MB, McGrath J, Coleman HG, Identifying mismatch repair-deficient colon cancer: Near-perfect concordance between immunohistochemistry and microsatellite instability testing in a large, population-based series: Histopathology, 2021; 78(3); 401-13
26.. Park Y, Nam SK, Seo SH, Comprehensive study of microsatellite instability testing and its comparison with immunohistochemistry in gastric cancers: J Gastric Cancer, 2023; 23(2); 264-74
27.. Hechtman JF, Rana S, Middha S, Retained mismatch repair protein expression occurs in approximately 6% of microsatellite instability-high cancers and is associated with missense mutations in mismatch repair genes: Mod Pathol, 2020; 33(5); 871-79
28.. Bartley AN, Luthra R, Saraiya DS, Identification of cancer patients with Lynch syndrome: Clinically significant discordances and problems in tissue-based mismatch repair testing: Cancer Prev Res (Phila), 2012; 5(2); 320-27
29.. Guyot D’Asnières De Salins A, Tachon G, Cohen R, Discordance between immunochemistry of mismatch repair proteins and molecular testing of microsatellite instability in colorectal cancer: ESMO Open, 2021; 6(3); 100120
30.. Rodrigues da Cunha Colombo Bonadio R, Gondim Meira Velame Azevedo R, Harada G, Adjuvant carboplatin and paclitaxel chemotherapy followed by radiotherapy in high-risk endometrial cancer: A retrospective analysis: J Glob Oncol, 2018; 4; 1-8
31.. Shitara K, Van Cutsem E, Bang YJ, Efficacy and safety of pembrolizumab or pembrolizumab plus chemotherapy vs chemotherapy alone for patients with first-line, advanced gastric cancer: The KEYNOTE-062 phase 3 randomized clinical trial: JAMA Oncol, 2020; 6(10); 1571-80
32.. Reck M, Rodríguez-Abreu D, Robinson AG, Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer: N Engl J Med, 2016; 375(19); 1823-33
33.. Magee DE, Hird AE, Klaassen Z, Adverse event profile for immunotherapy agents compared with chemotherapy in solid organ tumors: A systematic review and meta-analysis of randomized clinical trials: Ann Oncol, 2020; 31(1); 50-60
34.. Brahmer JR, Rodríguez-Abreu D, Robinson AG, Health-related quality-of-life results for pembrolizumab versus chemotherapy in advanced, PD-L1-positive NSCLC (KEYNOTE-024): A multicentre, international, randomised, open-label phase 3 trial: Lancet Oncol, 2017; 18(12); 1600-9
35.. Harrington KJ, Soulières D, Le Tourneau C, Quality of life with pembrolizumab for recurrent and/or metastatic head and neck squamous cell carcinoma: KEYNOTE-040: J Natl Cancer Inst, 2021; 113(2); 171-81
36.. Opławski M, Nowakowski R, Średnicka A, Molecular landscape of the epithelial-mesenchymal transition in endometrioid endometrial cancer: J Clin Med, 2021; 10(7); 1520
Figures
Tables
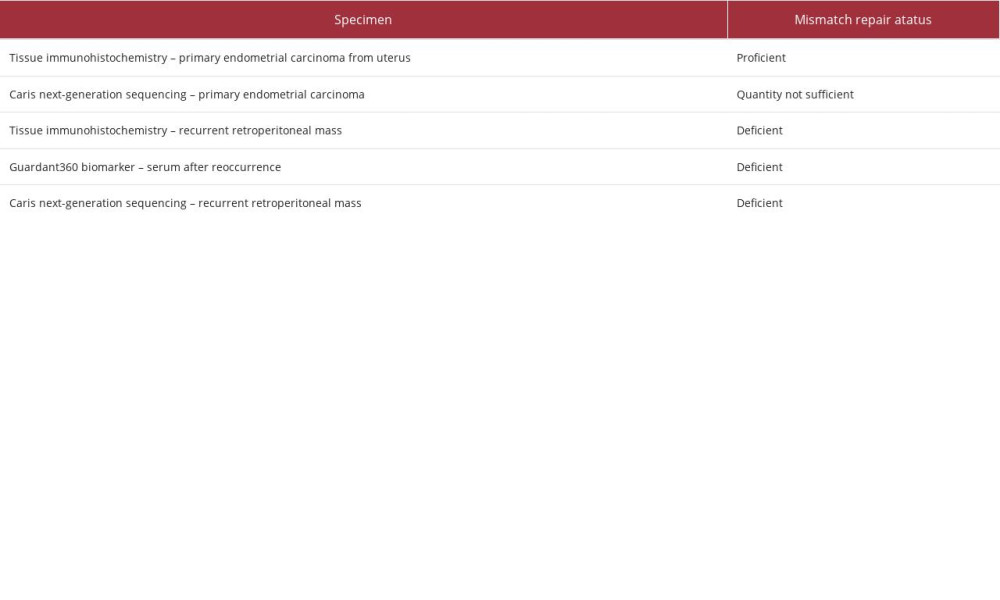 Table 1.. Immunohistochemical stain and next-generation sequencing for microsatellite instability.
Table 1.. Immunohistochemical stain and next-generation sequencing for microsatellite instability.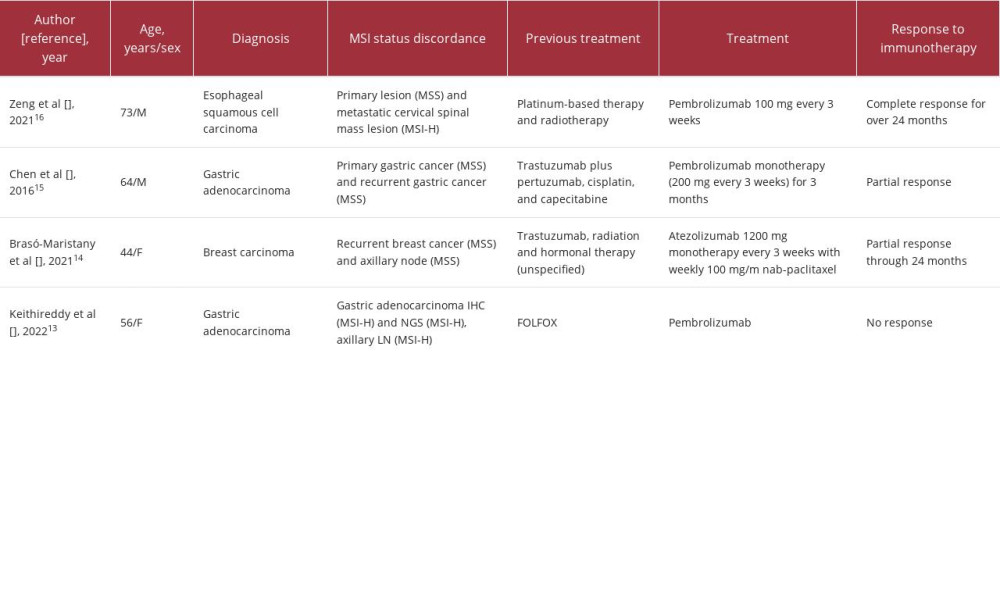 Table 2.. Case reports regarding discordance between primary and recurrent/metastatic carcinoma.
Table 2.. Case reports regarding discordance between primary and recurrent/metastatic carcinoma.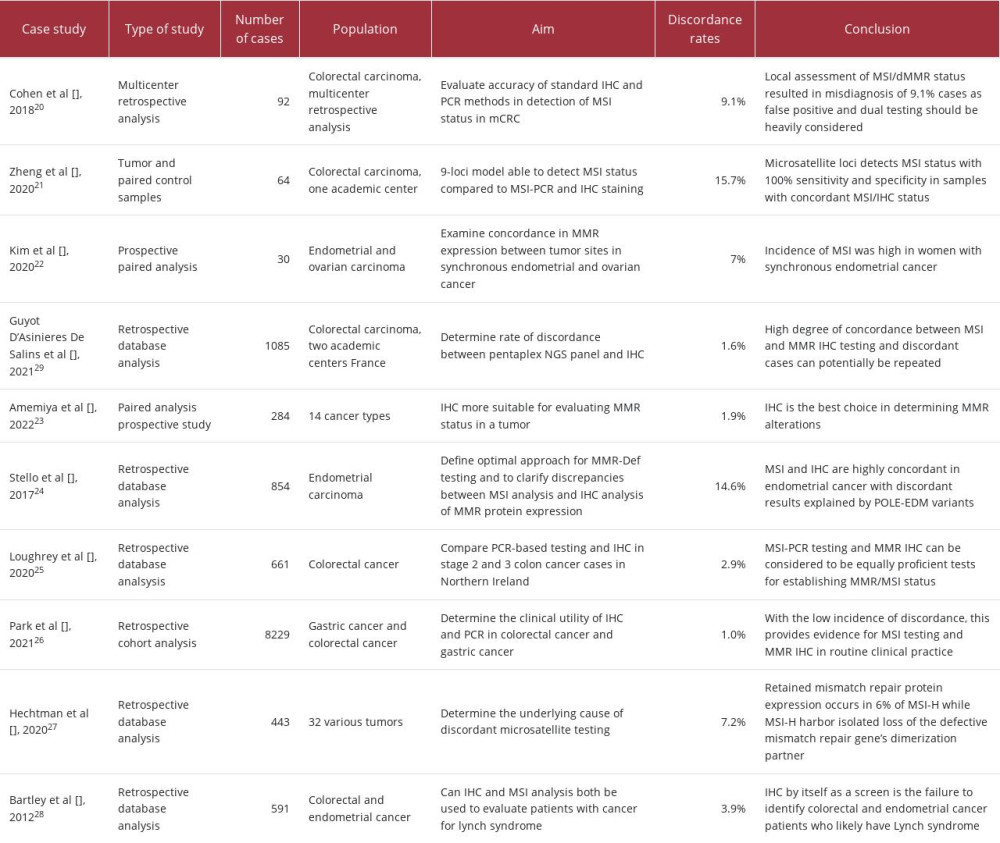 Table 3.. Studies regarding discordance of Immunohistochemistry and PCR/Next-Generation Sequencing in various carcinomas.
Table 3.. Studies regarding discordance of Immunohistochemistry and PCR/Next-Generation Sequencing in various carcinomas.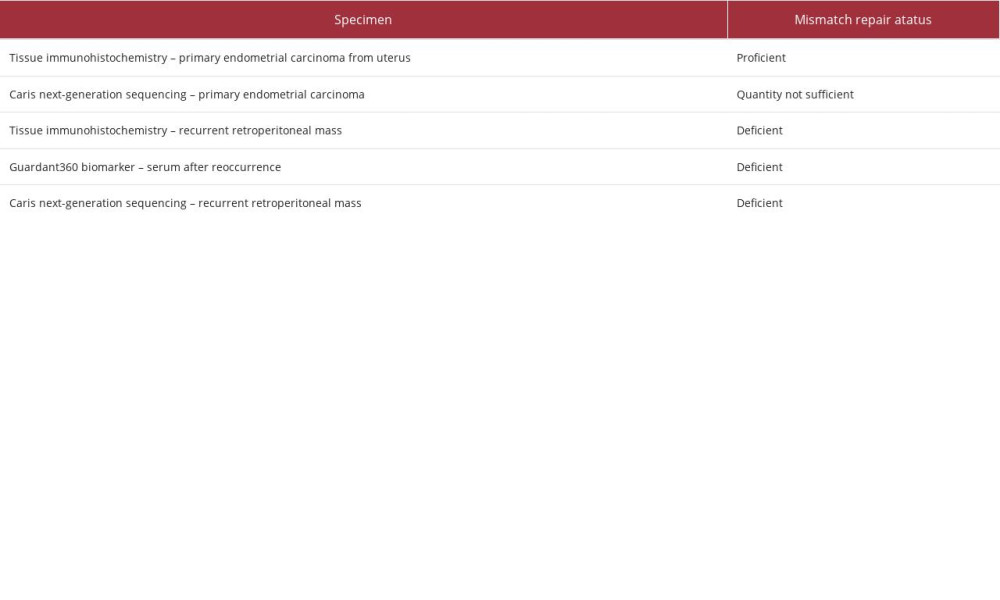 Table 1.. Immunohistochemical stain and next-generation sequencing for microsatellite instability.
Table 1.. Immunohistochemical stain and next-generation sequencing for microsatellite instability.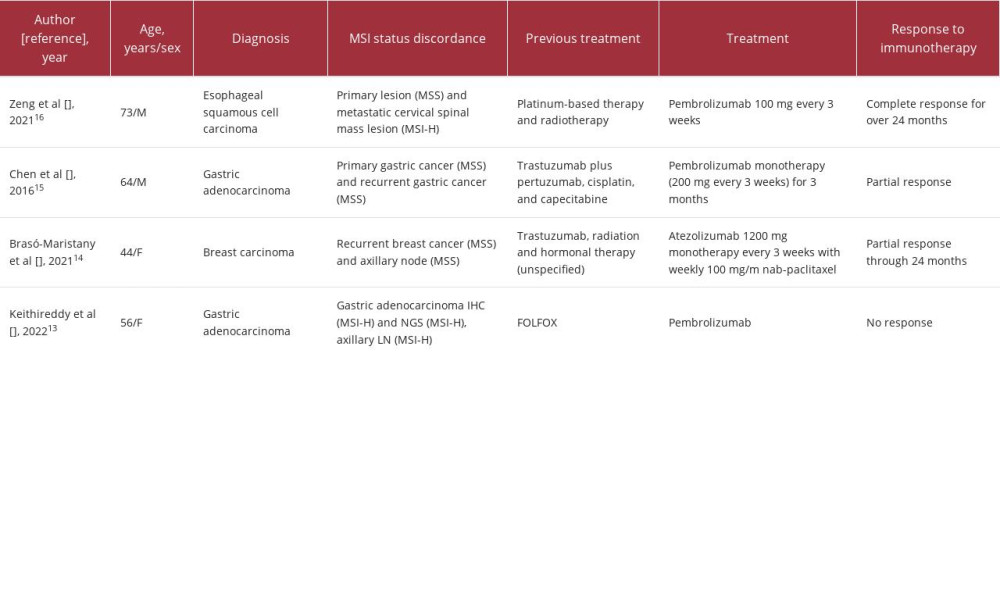 Table 2.. Case reports regarding discordance between primary and recurrent/metastatic carcinoma.
Table 2.. Case reports regarding discordance between primary and recurrent/metastatic carcinoma.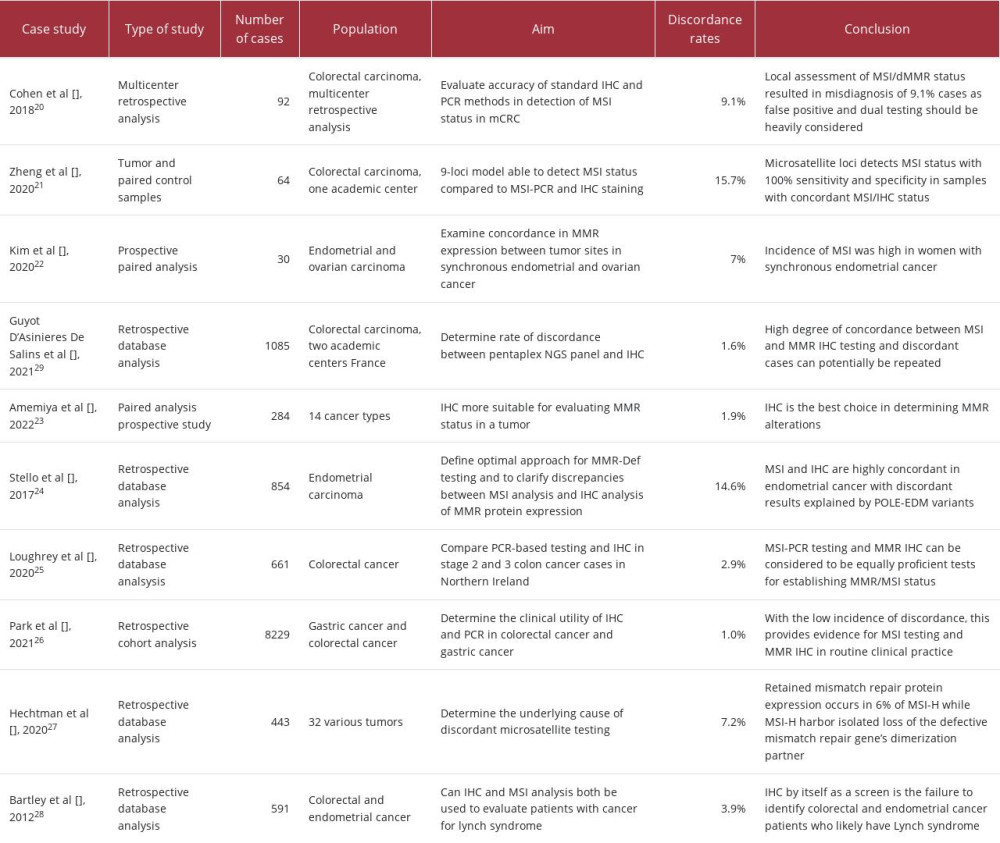 Table 3.. Studies regarding discordance of Immunohistochemistry and PCR/Next-Generation Sequencing in various carcinomas.
Table 3.. Studies regarding discordance of Immunohistochemistry and PCR/Next-Generation Sequencing in various carcinomas. In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943420
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942824
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








