15 August 2023: Articles 
Acute Esophageal Necrosis as a Rare Complication of Metabolic Acidosis in a Diabetic Patient: A Case Report
Challenging differential diagnosis
Salvatore Greco12ABEF, Antonio Giovine1ABEF, Cindy Rocchi1E, Riccardo Resca1E, Renato Bigoni1E, Luca Formigaro1E, Anna Grazia Angeletti1E, Nicolò Fabbri3E, Aurora BonazzaDOI: 10.12659/AJCR.939624
Am J Case Rep 2023; 24:e939624
Abstract
BACKGROUND: Acute esophageal necrosis, or Gurvits syndrome, is a rare clinical process often secondary to a systemic low-flow state. It can be caused by several medical conditions, and it is thought to arise from a combination of impaired mucosal barrier and chemical and ischemic insults to the esophagus. Acute esophageal necrosis usually presents with severe complications due to delayed diagnosis and only rarely has surgical indications. We present a case of Gurvits syndrome, presumably triggered by metabolic acidosis in a diabetic patient.
CASE REPORT: A 61-year-old man with history of hypertension and type 2 diabetes mellitus treated with metformin, canagliflozin, glimepiride, and pioglitazone came to our attention with persistent vomiting, odynophagia, chest pain after each meal, and progressive weight loss. Arterial blood analysis showed mild metabolic acidosis, while the first esophagogastroduodenoscopy performed revealed a circumferential black appearance of the esophageal mucosa, as in concentric necrosis of the distal esophagus with possible fungal superinfection. Brushing cytology confirmed the infection by Candida spp. and the patient was treated with intravenous fluconazole. The second esophagogastroduodenoscopy, performed after 2 weeks, showed almost complete healing of the esophageal mucosa; in this case, biopsy confirmed mucosal ischemia and necrosis, without showing deep impairment of the mucosa by fungal agents.
CONCLUSIONS: Due to its high lethality, often caused by the underlying medical diseases, acute esophageal disease should be considered in the differential diagnosis of digestive symptoms, even without upper gastrointestinal bleeding. Prompt diagnosis and treatment of contextual collateral conditions can help clinicians to avoid the worst outcomes of the disease. Among the causative factors of metabolic acidosis leading to esophageal necrosis we recognized metformin and dapagliflozin.
Keywords: Acute Disease, Esophageal Perforation, Esophagus, Humans, Male, Middle Aged, Acidosis, Diabetes Mellitus, Type 2, Esophageal Diseases, Necrosis
Background
Acute esophageal necrosis (AEN), also known as “black esophagus”, “necrotizing esophagitis”, and Gurvits syndrome, is a rare and underdiagnosed clinical disease characterized by a striking circumferential black appearance of the esophageal mucosa and it is reported to be a very rare cause of upper gastrointestinal bleeding. It was described for the first time in 1990 by Goldenberg et al [1], but brought into the spotlight only in 2007 by Gurvits et al, who gave the name to the underlying syndrome [2].
The prevalence of AEN is up to 0.2% in autopsy series [3], while it can be even lower in endoscopy series (0.01–0.28% of cases). Its incidence seems to be higher in males (up to 4 times higher than in females) and in middle-aged subjects [4,5]. In most cases AEN affects the distal esophagus, with a prevalence of 97%, usually sparing the other two-thirds of the organ and only rarely extended proximally, stopping almost universally at the gastro-esophageal junction [6].
Since its etiopathogenesis is supposed to be multifactorial, a holistic approach to patients is needed to provide a definite diagnosis: AEN, in fact, is thought to arise from a combination of impaired mucosal barrier and chemical and ischemic insults to the esophagus [7]. Possible risk factors for the development of this syndrome are male sex, malignancies, diabetes mellitus, cardiovascular diseases, prothrombotic conditions, chronic kidney disease, malnutrition, alcohol abuse, and gastro-esophageal reflux disease [8]. Eventual complications include stenosis or stricture formation in the distal esophagus, perforation, and mediastinitis; microbial superinfections (bacterial and/or fungal) of ischemic/necrotic areas are not rare and often need broad-spectrum intravenous antibiotic or antifungal treatment [9]; general treatment include high-dose proton pump inhibitors (PPIs), fluid therapy, correction of causative conditions, and monitoring for eventual complications [10].
Surgery is usually reserved to treat esophageal perforation with subsequent mediastinitis and abscess formation: standard surgical approaches can be followed by esophagectomy, decortication, lavage, and delayed reconstruction, while primary closure of the perforated tissue is not recommended [11].
The clinical presentation of AEN depends on the status of the esophageal mucosa and on the underlying medical conditions leading to mucosal ischemia and necrosis: symptoms range from functional pyrosis, vomiting, progressive dysphagia, and hematemesis. Overall mortality is usually related to the same conditions described above, ranging from 13% to 35%. Prompt diagnosis and therapy are thus necessary to avoid the worst outcomes related to the syndrome.
Until 2007, as reported by Gurvits et al, a total of 88 patients were diagnosed with AEN, while, to date (March 1, 2023), “black esophagus” is cited in less than 800 articles (less than 700 if we consider the “Acute esophageal necrosis”) in PubMed.
In this article we described the case of a diabetic patient admitted to our hospital with persistent digestive symptoms and later diagnosed with AEN, which was presumably caused by acidosis secondary to antidiabetic treatment, with superficial
Case Report
A 61-year-old man of Bulgarian origin with a medical history of hypertension and type 2 diabetes mellitus (T2DM) was admitted to our hospital with a 4-week history of persistent odynophagia, continuous vomiting, epigastric pain after each meal, and progressive weight loss of about 5 kilograms due to forced liquid diet. At hospital observation he was 175 cm tall, weighed 85 kilograms, with a body mass index (BMI) of 27.8 and showed cutaneous and mucosal moderate dehydration. His home medications included metformin, canagliflozin, glimepiride, and pioglitazone, but he was taking no medications for hypertension. He was a former smoker (20 pack years) and denied drinking alcohol, caustic ingestion, or eating spicy foods.
His vital signs were the following: Glasgow Coma Scale (GCS) 15 (E4V5M6), body temperature 36.5°C, blood pressure 165/100 mmHg, heart rate 120 beats per minute (bpm) and percutaneous oxygen saturation 98% on ambient air, without signs of dyspnoea (respiratory rate 14 per minute).
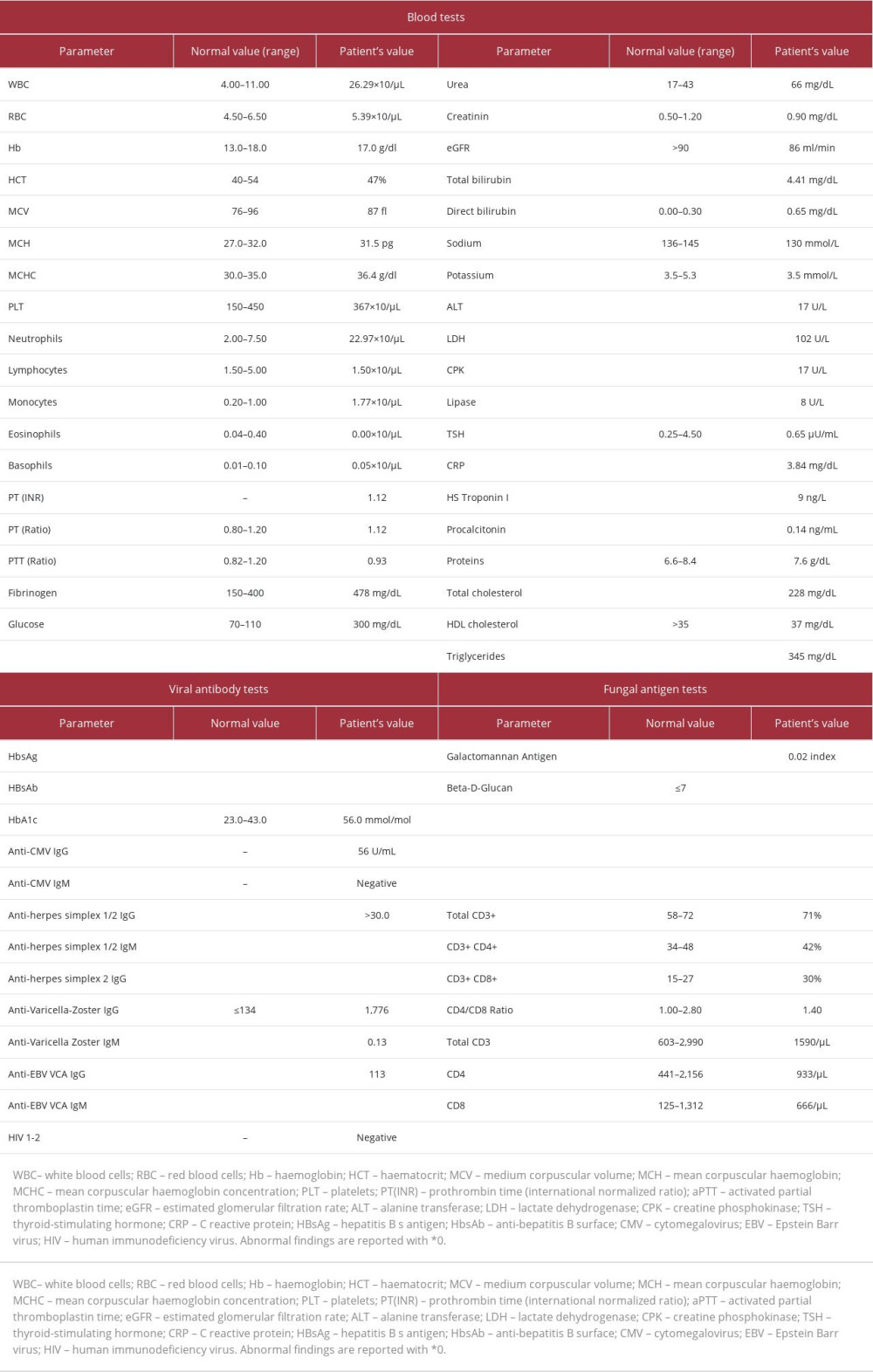
The physical examination was completely negative for remarkable pathological signs, while laboratory analysis revealed neutrophilic leukocytosis, and hyperglycemia (300 mg/dl), with mild elevation of glycated haemoglobin (HbA1c, 56.0 mmol/mol according to IFCC standardization) and mild hypertriglyceridemia (Table 1).
Arterial blood gas analysis showed metabolic acidosis and only partial respiratory compensation (pH 7.33, pO2 95 mmHg, pCO2 17 mmHg, HCO3-9 meq/L, LAC 1.4 mmol/L). The patient was diagnosed with “compensated metabolic acidosis in a diabetic patient.” The Emergency Room (ER) chest X-ray did not reveal signs of pneumonia or pleural effusion.
The patient was then admitted to the hospital and was treated with oral proton pump inhibitors (PPIs), later switched to intravenous administration, and basal bolus insulin with improved blood glycemic levels, and total parenteral nutrition (TPN). Empiric antibiotic treatment with amoxicillin/clavulanate was also instituted, as well as subcutaneous low-molecular-weight heparin (LMWH, enoxaparin) at prophylactic dosage (4000 IU/die); oral antidiabetic drugs were obviously discontinued.
On day 2, the patient underwent esophagogastroduodenoscopy (EGD), which revealed a malacic esophagus with circumferential necrosis of the distal third of the mucosa stopping at the gastro-esophageal junction; moreover, EGD showed a bulbar Forrest III ulcer with no sign of recent local bleeding (Figure 1A–1C). Biopsies were not taken due to mucosal fragility, but cellular brushing was performed. The patient was kept on
We also investigated the main causes of esophagitis, excluding some of the most important viral causes (HBV, HCV, herpes simplex and zoster, CMV, and EBV), searching for signs of an immunocompromised state: the study of lymphocyte sub-population and the HIV 1/2 test were both negative, as well as the blood cultures performed before empiric antibiotic therapy. CT scans revealed thickening of the distal esophagus, but no esophageal perforation (Figure 2A–2C).
On day 5 we received the brush cytology report, which revealed fungal hyphae by
The final pathology report, received after discharge, showed
Discussion
AEN is a rare condition, only occasionally reported in the literature and often leading to worse outcomes due to delayed diagnosis and complications. The multifactorial etiopathogenesis is supposed to be the basis for the development of “black esophagus” and diabetic-related acidosis can be among the most common underlying conditions [10,12].
Diabetes mellitus, together with malignancies, chronic kidney disease, poor nutritional status, cardiovascular illnesses, and general deconditioning, can predispose to altered and compromised mucosal barriers, which could potentiate eventual chemical or ischemic injury to the esophagus [13,14].
A low-flow state, common in case of sepsis, congestive heart failure, systemic inflammation, or lactic- and keto-acidosis, can lead to mucosal ischemia and necrosis (focal or extended), which is favoured by the particular segmentation of the arterial network of the esophagus. While the upper third is vascularized by the descending branches from the inferior thyroid arteries and numerous additional small arteries, the middle esophagus receives its blood supply from the bronchial arteries, right third or fourth intercostal arteries, and numerous small esophageal arteries from the descending aorta. Finally, the distal third of the esophagus has less blood supply, provided by small branches from the left gastric artery or left inferior phrenic artery, with several possible anatomic variations: consequently, ischemic injuries typically affect this part of the organ.
The first arterial blood sample in our patient showed mild metabolic acidosis, but the prolonged vomiting in the previous days had probably buffered the blood pH, which could have been even lower during the first phases of metabolic acidosis. Some of the patient’s own medications (eg, metformin and canagliflozin) may also have contributed to development of metabolic acidosis, as already described for biguanides and SGLT-2 inhibitors in a small percentage of cases [15,16].
As already stated above, microbial infections commonly complicate AEN, requiring in most cases specific and long-lasting treatment [17] – this happened to our patient, since
Although biopsy is not always needed to confirm the diagnosis of AEN, it is strongly recommended: necrotic debris, absence of squamous epithelium, and necrosis of mucosa are often present. We were able to collect biopsy samples only during the second EGD due to mucosal fragility at the first endoscopy: histological analysis showed the presence of ulcerated and partially necrotic mucosa, with tracks of granulation tissue, as signs of repair attempts by the esophageal mucosa itself. Hence, all symptoms and findings seem to be compatible with the diagnosis of AEN we made and, after 6 months of remote follow-up, the patient did not show further digestive symptoms and reported complete healing of the acute disease.
It is our opinion that the patient’s home therapy could be the key for understanding the origin of metabolic acidosis and that one drug or both metformin and canagliflozin could have strongly contributed to it, leading to focal esophageal ischemia and necrosis and, contextually, to the digestive symptoms.
In healthy patients without immune compromise, it is very hard to find circumferential necrosis due to fungal infections, since in immunocompromised subjects such infections usually affect the entire mucosa. In our case, the only finding in mucosal tissue was partial necrosis and no signs of fungal infiltration were encountered, showing how the fungal infection was primarily the consequence and not the cause of AEN.
As in almost all cases of AEN, factors clearly leading to the disease are rarely found, and also in our case, it was hard to determine which factors formerly acted as the “primum movens” in the development of esophageal necrosis.
Although AEN is gaining attention among the medical community, it is still an underdiagnosed illness, and it is rarely recognized, with high mortality rates due to delayed diagnosis and therapy. For this reason, we are convinced that each case report is a chance for clinicians to learn about such a disease and could be the basis for further and larger studies on the topic.
Conclusions
We presented a case of AEN presumably triggered by metabolic acidosis and complicated with fungal infection in a diabetic patient.
AEN is an uncommon, potentially lethal, medical condition, and should be included in the differential diagnosis of upper gastrointestinal bleeding or digestive symptoms in diabetic patients. The endoscopic approach, with or without biopsy, can be necessary to avoid the worst outcomes of the illness. In this case, we hypothesized that the causative agents leading to esophageal necrosis were (one or both) the antidiabetic drugs metformin and canagliflozin.
Figures
References:
1.. Goldenberg SP, Wain SL, Marignani P, Acute necrotizing esophagitis: Gastroenterology, 1990; 98; 493-96
2.. Gurvits GE, Shapsis A, Lau N, Gualtieri N, Robilotti JG, Acute esophageal necrosis: A rare syndrome: J Gastroenterol, 2007; 42; 29-38
3.. Etienne JP, Roge J, Delavierre P, Veyssier P, [Esophageal necrosis of vascular origin.]: Sem Hop, 1969; 45; 1599-606 [in French]
4.. Postlethwait RW, Musser AW, Changes in the esophagus in 1,000 autopsy specimens: J Thorac Cardiovasc Surg, 1974; 68; 953-56
5.. Lacy BE, Toor A, Bensen SP, Acute esophageal necrosis: Report of two cases and a review of the literature: Gastrointest Endosc, 1999; 49; 527-32
6.. Weerakkody Y, Acute oesophageal necrosis.: Radiopaedia.org;, 2022
7.. Le K, Ahmed A, Acute necrotizing esophagitis: Case report and review of the literature.: J La State Med Soc, 2007; 159(330); 333-38
8.. Augusto F, Fernandes V, Cremers MI, Acute necrotizing esophagitis: A large retrospective case series: Endoscopy, 2004; 36; 411-15
9.. Kim Y-H, Choi S-Y, Black esophagus with concomitant candidiasis developed after diabetic ketoacidosis: World J Gastroenterol, 2007; 13; 5662-63
10.. Dias E, Diagnosis and management of acute esophageal necrosis: Ann Gastroenterol, 2019; 32(6); 529-40
11.. Gurvits GE, Black esophagus: Acute esophageal necrosis syndrome: World J Gastroenterol, 2010; 16; 3219-25
12.. Jaber F, Alsakarneh S, Sripada S, “Black esophagus” or Gurvits syndrome: A rare cause of upper gastrointestinal bleeding in diabetic ketoacidosis: Cureus, 2023; 15(2); e34989
13.. Siddiqi A, Chaudhary FS, Naqvi HA, Black esophagus: A syndrome of acute esophageal necrosis associated with active alcohol drinking: BMJ Open Gastroenterol, 2020; 7; e000466
14.. Rodriguez Fernandez L, García Sánchez MC, Prieto de Paula JM, Miramontes González JP, Black esophagus and diabetes: A close relationship: Cardiovasc Endocrinol Metab, 2020; 10; 59-61
15.. Mathieu C, Ranetti AE, Li D, Randomized, double-blind, phase 3 trial of triple therapy with dapagliflozin add-on to saxagliptin plus metformin in type 2 diabetes: Diabetes Care, 2015; 38; 2009-17
16.. Matthaei S, Catrinoiu D, Celiński A, Randomized, double-blind trial of triple therapy with saxagliptin add-on to dapagliflozin plus metformin in patients with type 2 diabetes: Diabetes Care, 2015; 38; 2018-24
17.. Grudell ABM, Mueller PS, Viggiano TR, Black esophagus: Report of six cases and review of the literature, 1963–2003: Dis esophagus, 2006; 19; 105-10
Figures
In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943136
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943645
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942921
22 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943346
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250