21 June 2023: Articles 
Effective Surgical Management of a Large Serous Ovarian Cyst in a Morbidly Obese Middle-Aged Woman: A Case Study and Literature Review
Rare disease
Michele Peiretti1ABDE, Valerio Mais1ABD, Gianmarco D'AnconaDOI: 10.12659/AJCR.939697
Am J Case Rep 2023; 24:e939697
Abstract
BACKGROUND: In contemporary gynecological practice, encountering giant ovarian tumors is a rarity. While most are benign and of the mucinous subtype, the borderline variant only accounts for approximately 10% of these cases. This paper addresses the paucity of information about this specific subtype, emphasizing critical elements of managing borderline tumors that can pose life-threatening complications. Additionally, a review of other documented cases of the borderline variant in the literature is also included to foster a deeper understanding of this uncommon condition.
CASE REPORT: We present the multidisciplinary management of a 52-year-old symptomatic woman with a giant serous borderline ovarian tumor. Preoperative assessment showed a multiloculated pelvic-abdominal cyst responsible for compression of the bowel and retroperitoneal organs, and dyspnea. All tumor markers were negative. Together with anesthesiologists and interventional cardiologists, we decided to perform a controlled drainage of the cyst of the tumor, to prevent hemodynamic instability. Subsequent total extrafascial hysterectomy, contralateral salpingo-oophorectomy, and abdominal wall reconstruction, followed by admission to the intensive care unit, were also conducted by the multidisciplinary team. During the postoperative period, the patient experienced a cardiopulmonary arrest and acute renal failure, which were managed by dialysis. After discharge, the patient underwent oncologic followup, and after 2 years, she was found to be completely recovered and disease free.
CONCLUSIONS: Intraoperative controlled drainage of Giant ovarian tumor fluid, planned by a multidisciplinary management team, constitutes a valid and safe alternative to the popular choice of “en bloc” tumor resection. This approach avoids rapid changes in body circulation, which are responsible for intraoperative and postoperative severe complications.
Keywords: case reports, Ovarian Cysts, Ovarian Neoplasms, Patient Care Team, Middle Aged, Female, Humans, Obesity, Morbid, Renal Dialysis, Cysts
Background
Giant ovarian tumors (GOTs) are rare tumors of the ovary with no current consensus on their definition. Some authors have described GOTs as tumors with diameter greater than 10 cm, while others set the cut-off at 20 cm [1,2].
In the modern era of medicine, such large ovarian tumors are rarely observed in current medical practice, given that most cases are diagnosed early during routine gynecological examinations or incidental findings on ultrasound examination of the pelvis and abdomen [3].
These tumors are generally asymptomatic at early stages, with clinical symptoms present only after the tumor has reached massive dimensions. These clinical symptoms include progressive abdominal distension, nonspecific diffuse abdominal pain, vaginal bleeding, and symptoms related to organ compression.
In the English literature, giant cysts are described as mainly benign with a mucinous subtype. We herein present a rare case of a giant serous ovarian borderline tumor (GOBT), which constitutes only 10% of all GOTs [4].
The aim of the present paper is to highlight some critical aspects of GOBTs, given the lack of data in the literature regarding this histological type of giant ovarian cysts/tumors. It also remarks upon the importance of multidisciplinary management to obtain a feasible and safe surgical approach to prevent the many life-threatening complications related to rapid changes in circulation.
Moreover, we review other cases of borderline GOTs published in the literature in, to improve the knowledge and management of this rare condition.
The following case report was written according to CARE guidelines [5].
Case Report
A 52-year-old nulliparous woman was referred to our gynecological department after previous hospitalization in the internal medicine unit. During the last 10 years, she gradually developed massive abdominal distention responsible for reflux, early satiety, constipation, difficulty in ambulation, and progressive pulmonary and cardiological symptoms, such as dyspnea. The delayed diagnosis in this woman was probably due to her low socio-economic and educational status, which led the patient to postpone medical evaluation since she assumed she was getting obese. At gynecological anamnesis, the patient was a virgin. The cyst had no apparent hormonal effects on her periods. Despite her age, she reported regular menstrual cycles. Her past medical history did not present previous noteworthy surgical interventions. Her personal medical history revealed class 3 obesity (weight 123 kg; height 156 cm; BMI 50.5). Moreover, her family history was negative for malignant ovarian or breast cancer in first-degree relatives.
On physical examination, the patient was conscious and oriented with normal vital parameters. Her abdomen was massively distended with evident skin discoloration and cutaneous striae and tense upon palpation as shown in Figure 1.
The margins of the mass were not well defined, arising from the lower pelvis and extending from the xiphisternum up to both sides of the iliac fossa.
Laboratory investigation showed a low level of hemoglobin (10.3 g/dL), hepatic and renal profiles in deterioration (creatinine 1.65; total bilirubin 7.25), and negativity for tumor markers including the cancer antigen-125 (CA-125), carcinoembryonic antigen (CEA), cancer antigen 19.9 (CA 19-9) and α-fetoprotein (CA-125=33 U/mL; CEA=0.97 ng/mL; CA 19-9=19.2 U/mL; α-fetoprotein=1.1 ng/mL).
Ultrasound examination showed that the abdominal cavity was entirely occupied by heterogeneous lesions.
To improve presurgical information and obtain an accurate estimation of tumor size, it was also necessary to perform a computed tomography (CT) scan. The CT scan revealed a multiloculated pelvic-abdominal cyst measuring approximately 47×36×33 cm with septa and fluid or semifluid content, suggesting an ovarian cyst as shown in Figure 2. The abdominal mass was responsible for compression of the bowel and retroperitoneal organs. The kidneys and liver were normal, and no ascites was seen.
The clinical case was discussed by a multidisciplinary team composed of a gynecologic oncologist, plastic surgeon, anesthesiologist, general surgeon, and interventional cardiologist. The multidisciplinary team considered the risk of intraoperative death following hemodynamic instability and bleeding as well as the postoperative risk of deep vein thrombosis, pulmonary embolism, difficulty weaning off the ventilator, and death. The proposed surgical approach was initial laparotomic removal of the mass using controlled drainage and intra-operative histopathological analysis followed by abdominal wall reconstruction. Admission to the intensive care unit after surgery was also planned due to postoperative mortality risk.
The patient was informed about all the complications, and she provided consent to undergo the high-risk surgical procedure. Before surgery, anemia was corrected with packed red blood cells in 2 units.
A xiphopubic incision was made with the patient under general anesthesia in the head-up and left lateral tilt positions to avoid supine hypotension (Figure 1). An incision was performed on the cyst surface and it was large enough to allow the introduction of a suction cannula and to thereby avoid any inadvertent peritoneal spillage. The suction of fluid content was carried out as slowly as possible to prevent rapid changes in body circulation.
Approximately 37 liters of dense brown fluid were drained and at the end of the drainage, the patient was turned to the supine position. The GOBT originated from the right ovary and both were removed prior to excision of dense adhesions to the parietal peritoneum, stomach, and bowel. At the end of the drainage, the maximum length of the cyst wall was 40 cm, and its capsule weight was 5.097 kg. Exploration of the abdominal cavity demonstrated a smooth peritoneum with omentum, bowel, and the surfaces of upper abdominal organs free of suspected metastatic nodules. No lymphadenopathy was found.
Total extrafascial hysterectomy with contralateral salpingo-oophorectomy were performed. The peritoneum and omentum were also sent for histopathology as part of the staging laparotomy. The appendix was enlarged by coprolites and was also removed. Intraoperative histopathological analysis revealed an apparent stage IA serous borderline ovarian tumor which was confirmed by final pathology.
The second surgical step consisted of abdominal wall reconstruction by a plastic surgery team. To reduce the size of the abdominal cavity, the Fleur-De-Lys technique was used, which allowed the removal of a large quantity of redundant abdominal wall, especially skin and subcutaneous tissue, yielding a total of 12 kg (Figure 3). At the end of the procedure, the postoperative BMI of the patient was 28.3.
The overall duration of surgery was 400 minutes, during which 6 units of blood were lost and subsequently transfused.
After surgery, the patient was transferred to the intensive care unit and remained there for approximately 30 days, during which time she experienced cardiopulmonary arrest due to postoperative hypovolemia and temporary dialytic therapy was necessary to manage acute renal failure. When the patient was readmitted to the gynecological unit, blood samples, disinfection of the abdominal wound, and physiotherapy rehabilitation were performed daily.
After 2 months, the patient was discharged from the hospital, and she was transferred to a rehabilitation center in good health. The patient underwent oncologic followup, and after 2 years she is completely recovered and disease free.
Discussion
Giant ovarian cysts constitute a challenging condition in general practice given their rarity and their nonspecific clinical features and findings, resulting in a wide range of differential diagnoses, such as pelvic endometriosis, intra-abdominal pregnancy, and intra-abdominal cysts from varying origins (omentum, kidney, liver, pancreas, cystic lymphangiomas, or choledochal cysts).
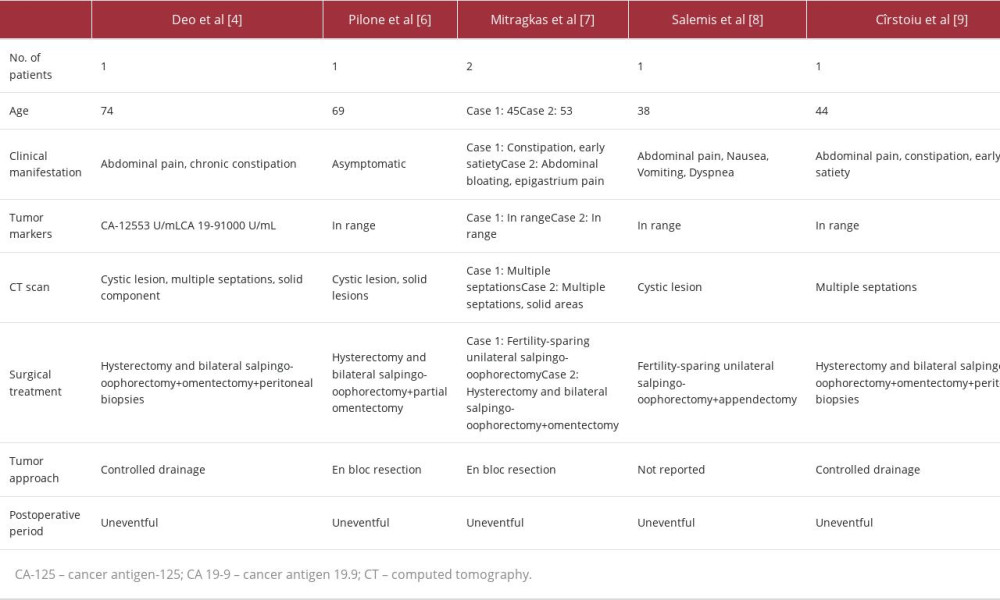
Large ovarian masses described in the literature are mostly benign, but malignancy should be excluded by investigations and clinical assessment [4]. Only a few reports describe patients affected by GOBT, with a variety of clinical manifestations (Table 1) [4,6–10]. The most frequently reported symptoms are related to the compressive effect of the tumor, such as chronic constipation, early satiety, and dyspnea in severe cases. Alternatively, the patient can be asymptomatic, as described by Pilone et al in 2018 [6].
At preoperative imaging assessment, the lesion is frequently described as multiloculated with multiple septations and intracystic solid areas. Trans-abdomen ultrasound is considered to be a first line modality, followed by CT scan, which can provide further information such as the relationship with other anatomical structures. In order to predict the risk of malignancy of ovarian masses, the evaluation of tumor markers is suggested. In most reported cases, the masses were negative for tumor markers [6,8,9], except for Lee et al (2016) [10] and Deo et al (2022) [4]. In the case report of Lee et al, the authors reported CA 19-9 and CA-125 levels of 2581 U/mL and 284 U/mL, respectively, but these levels were probably related to the young age of the patient [10].
Management of a patient with GOT should be planned with a multidisciplinary approach, due to the risk of fatal surgical complications such as pulmonary and cardiac failure, pulmonary embolism, and sepsis [11]. Thus, adequate supportive care to resect giant ovarian masses is of the utmost importance.
Owing to their compressive symptoms and risk of malignancy, surgery is mandatory in patients with GOT, and laparotomic removal with intraoperative pathological evaluation remains the standard criterion of treatment [12].
The most commonly reported surgical technique for treating GOBTs consists of “en bloc” resection of tumors without controlled drainage of tumor fluid. Aspiration of an abdominal cyst is not considered a safe procedure compared with “en bloc” removal of the tumor, since it can lead to some complications, such as infections, bleeding, cyst rupture, increased peritoneal adhesion, or possible dissemination of malignant cells [13]. Inadvertent peritoneal spillage is considered unsafe especially with mucinous masses, owing to the rare possibility of pseudomyxoma peritonei. Thus, some authors declare that aspiration of abdominal cysts should be avoided [1].
On the other hand, many case reports have shown that controlled drainage of the tumor can adequately prevent the hemodynamic instability related to rapid changes in body circulation [4,9]. Controlled drainage is reported as useful in preventing supine hypotension syndrome and splanchnic shock due to fast decompression of the splanchnic vascular bed adjacent to the inferior vena cava [14]. Similarly, pulmonary edema related to the sudden expansion of the chronically collapsed lung can be avoided with intraoperative drainage. In the present case, we decided to perform slow fluid component drainage due to the large size of the tumor and the risk of inadvertent rupture of the cyst related to high wall tension.
To reduce hemodynamic instability, in addition to intraoperative drainage, lateral decubitus is mandatory during this surgery. The supine position should be avoided given that resultant vena cava compression can reduce cardiac output with sudden loss of pulse and cardiac arrest.
In most of the case reports in the literature, the authors preferred a midline abdominal incision, although the choice depends on the size of the tumor and preference of the surgeon. On the contrary, Matory et al (1989) reported that a low transverse incision is associated with a lower risk of ventral hernia formation and permits a better restoration of normal rectus abdominis muscle function [15].
In the postoperative period, reducing ileus, providing respiratory support, supporting abdominal wall tension, and monitoring hemodynamic parameters in the intensive care unit are of the utmost importance to reduce the risk of complications [6].
Conclusions
This case report provides further information about this rare condition and highlights the importance of detection, preoperative evaluation, and subsequent surgical management of giant ovarian cysts with a multidisciplinary approach to decrease preoperative and postoperative complications and improve the quality of human life.
References:
1.. Yeika EV, Efie DT, Tolefac PN, Fomengia JN, Giant ovarian cyst masquerading as a massive ascites: A case report: BMC Res Notes, 2017; 10(1); 749
2.. Kumar V, Abbas AK, Aster JC: Robbins and Cotran pathologic basis of disease., 2015; 696-98, Philadelphia, PA, Elsevier/Saunders
3.. Katke RD, Huge mucinous cystadenoma of ovary with massive third degree uterovaginal prolapse in postmenopausal woman: Rare case report and review of literature: Int J Reprod Contracept Obstet, 2015; 4(1); 255-58
4.. Deo A, Shrivastava D, Shanoo A, Giant borderline mucinous cystadenoma: A distressing scenario: Cureus, 2022; 14(4); e23968
5.. Rison RA, Kidd MR, Koch CA, The CARE (CAse REport) guidelines and the standardization of case reports: J Med Case Rep, 2013; 27(7); 261
6.. Pilone V, Tramontano S, Picarelli P, Giant mucinous ovarian borderline tumor: A good lesson from an asymptomatic case: Int J Surg Case Rep, 2018; 50; 25-27
7.. Mitragkas P, Synekidou E, Hatzimisios K, Giant ovarian mucinous borderline tumors: A report of two cases and literature review: Maedica (Bucur), 2021; 16(4); 743-46
8.. Salemis NS, Pinialidis D, Karalis G, Giant mucinous borderline ovarian tumour: ANZ J Surg, 2009; 79(10); 766-67
9.. Cîrstoiu MM, Sajin M, Secară DC, Giant ovarian mucinous cystadenoma with borderline areas: A case report: Rom J Morphol Embryol, 2014; 4(55); 1443-47
10.. Lee HM, So KA, Kim MK, A case report of a young girl with mucinous borderline tumor of the ovary: Obstet Gynecol Sci, 2016; 59(4); 333-36
11.. Katke RD, Giant mucinous cystadenocarcinoma of ovary: A case report and review of literature: J Mid-life Health, 2016; 7(1); 41-44
12.. Eisenhauer EL, Abu-Rustum N, Sonoda Y, The effect of maximal surgical cytoreduction on sensitivity to platinum-taxane chemotherapy and subsequent survival in patients with advanced ovarian cancer: Gynecol Oncol, 2008; 108(2); 276-81
13.. Webb MJ, Decker DG, Mussey E, Williams TJ, Factor influencing survival in stage 1 ovarian cancer: Am J Obstet Gynecol, 1973; 116; 222-28
14.. Einenkel J, Alexander H, Schotte D, Giant ovarian cysts: Is a pre and intra operative drainage an advisable procedure: Int J Gynecol Cancer, 2006; 16(6); 2039-43
15.. Matory W, Pretorius RG, Hunter RE, Gonzalez F, A new approach to massive abdominal tumors using immediate abdominal wall reconstruction: Plast Reconstr Surg, 1989; 84(3); 442-48
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250