07 January 2024: Articles 
Graves’ Disease Exacerbation with Impending Thyroid Storm After SARS-CoV-2 Infection: A Case Report
Challenging differential diagnosis, Management of emergency care, Rare coexistence of disease or pathology
William P. Sebastian1BDEF, Aijaz Parisa2EF, Mansi Pandya1EF, Amna Anees23ABCDEF*DOI: 10.12659/AJCR.941311
Am J Case Rep 2024; 25:e941311
Abstract
BACKGROUND: Since the COVID-19 pandemic, several cases of COVID-19 have been linked to the development of autoimmune disorders, including of the thyroid. Graves’ disease (GD) is a rare complication that can occur following SARS-CoV-2 infection. Reports have linked COVID-19 to new onset and exacerbation of GD. We present a case of a 42-year-old woman with a history of GD presenting with impending thyroid storm 3 weeks following a diagnosis of COVID-19.
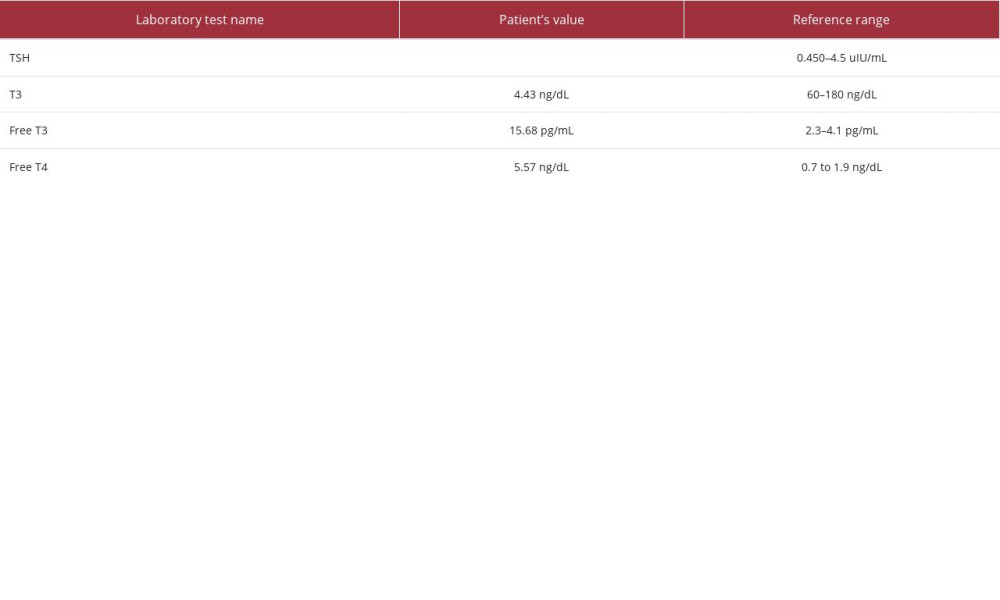
CASE REPORT: A 42-year-old woman with a history of GD presented to the Emergency Department (ED) for an acute exacerbation of hyperthyroidism 3 weeks after SARS-CoV-2 infection was diagnosed on a home test. Symptoms included daily headaches, increased bilateral eye pressure, fatigue, muscle weakness, episodes of confusion and agitation, persistent heart palpitations, and goiter. Elevated free T4 of 5.57, free T3 of 15.68, total T3 of 4.43, and near-absent thyroid stimulating hormone were noted. The Burch-Wartofsky scale was 40, which was concerning for an impending thyroid storm; however, at the time of admission, she was not in a thyroid storm. Treatment included propylthiouracil, potassium iodide oral solution, and propranolol, with symptom improvement. Due to prior history of intolerance to antithyroid medications and recent exacerbation, a thyroidectomy was performed once she was in a euthyroid state.
CONCLUSIONS: Our case demonstrates the importance of recognizing COVID-19 as an etiology or a trigger for new onset or exacerbation of GD. Our case highlights that being vigilant to recognize the association between COVID-19 and thyroid abnormalities for early diagnosis and treatment is imperative.
Keywords: Adult Multisystem Inflammatory Disease, COVID-19 Related, Graves Disease, hyperthyroidism
Background
Since the emergence of the COVID-19 pandemic, there has been a surge of reports linking the effects of SARS-CoV-2 infection with the development of various autoimmune diseases, including rheumatologic conditions [1], hematologic conditions [2], Guillain-Barré syndrome [3], and type 1 diabetes [4]. We are still elucidating the effects of SARS-CoV-2 on the thyroid gland, but several reports have demonstrated a spectrum of thyroid ailments, including Hashimoto disease, Graves’ disease (GD), postpartum thyroiditis, and subclinical thyroid abnormalities [5,6]. Patients with a history of thyroid disease or a genetic disposition can experience a more severe infection [7]. New onset or exacerbation of GD is a rare complication that can occur from SARS-CoV-2 infection [8,9]. We report a case of a 42-year-old woman with a history of GD, with an impending thyroid storm, following a diagnosis of COVID-19.
Case Report
A 42-year-old woman with a past medical history significant for tobacco use disorder and recent diagnosis of GD presented to the Emergency Department (ED) with a 10-day history of worsening daily headaches. During this time, she also had increased bilateral eye pressure with evidence of mild proptosis (but no vision changes), fatigue, muscle weakness, episodes of confusion and agitation, increased appetite, heat intolerance, and persistent heart palpitations. She and close members of her family tested positive for SARS-CoV-2 infection 3 weeks before her visit to the ED. The patient had conducted a home test for SARS-CoV-2 and unfortunately did not know the exact brand of the test she used. She was diagnosed with GD 6 months before the current presentation. At the time of her diagnosis, she had negative TSH receptor antibodies, and a positive thyroglobulin radioactive iodine uptake test, with a 76% 24-h uptake, consistent with the diagnosis of GD. The ultrasounds at that time demonstrated no evidence of thyroid nodules or cysts. She had previously tried propylthiouracil and methimazole, with slight intolerance to both medications, as they lead to fatigue. On the current presentation to the ED, she had an elevated free T4 level of 5.57 ng/dL, free T3 level of 15.68 ng/mL, total T3 level of 4.43 pg/mL, and near-absent TSH level of.01 uIU/mL. These values are compared with the reference ranges in Table 1. On the physical examination, the patient was anxious overall, with a non-tender palpable goiter and no evidence of a bruit. She had mild, non-tender proptosis, with a negative lid lag test. The skin was warm and moist, with no observable dermatological abnormalities. The patient had tachycardia and hypertension. Electrocardiogram showed sinus tachycardia. Her calculated Burch-Wartofsky scale at presentation was 40, which was concerning for an impending thyroid storm. The patient was treated with propylthiouracil, potassium iodide oral solution, and propranolol until euthyroid. She then underwent a curative thyroidectomy. She tolerated the procedure well and was discharged home 2 days after surgery.
Discussion
Our case highlights the impact of the pandemic on clinical outcomes following infection with SARS-CoV-2 and the association with autoimmune diseases. Autoimmune disorders are known to occur following viral infections, but the rate and varying degrees at which these disorders have presented following SARSCoV-2 infections are quite variable. Although our patient had a history of GD before the infection, her symptoms were controlled even with her having slight intolerance to anti-thyroid medications. The exacerbation of GD following COVID-19 disease is rare, as the most common thyroid-related complication in such an illness is subacute thyroiditis [9]. When comparing our patient with other cases previously published, she had a similar presentation, with tachycardia, headache, and bilateral eye pressure; however, it is interesting to note that she had impending but not actual thyroid storm at presentation [10,11].
Hashimoto thyroiditis is a more commonly reported autoimmune disorder associated with viral illnesses. The vast spectrum of thyroid disorders proceeding the infection further highlights the many unknowns of SARS-CoV-2. When SARS-CoV-2 enters the host, it binds to angiotensin-converting enzyme 2 (ACE2) receptors via its spike protein [6]. Although ACE2 is most notably associated with lung tissue, many other human cells express it as well, including those in the pancreas, thyroid, testis, ovary, adrenal glands, and pituitary gland [12].
There is still uncertainty on how SARS-CoV-2 may directly impact the thyroid gland. However, several studies have found that the virus affects the follicular epithelial and parafollicular cells, limiting T3 and T4 production. A subgroup analysis of SARS-CoV-2-infected patients found that the subsequent depression in thyroid function via measured T3 levels inversely correlates with the severity of SARS-CoV-2 infections [13].
Even in less severe cases, the prevalence of subclinical and euthyroid alterations in thyroid function is common, demonstrating the association between the two. TSH and free T3 levels might be a marker for clinical outcomes in infected patients. A study by Durgun et al revealed that thyroid hormone changes were linked to the severity and mortality in patients with COVID-19 [14]. A study of 541 patients found those with lower levels of TSH and free T3 demonstrated higher rates of lymphopenia and subsequent deterioration during infection [15]. Long-term complications of COVID-19, such as chronic fatigue, have become common. These complications might stem from the disruption of the hypothalamus-pituitary-thyroid axis. The thyroid may be pivotal in regulating homeostasis during host SARS-CoV-2 infections. One study found the virus was associated with pro-inflammatory cytokines; inter-feron-γ and tumor necrosis factor-α were found to increase the thyroid’s ACE2 receptor expression. An increase in these cytokines is associated with higher ACE2 expression in the thyroid [16]. The higher expression can modulate the resultant immune response, affect the spectrum of severities seen in SARS-CoV-2 infections, and lead to the disposition to acquire thyroid-related disorders. This phenomenon was observed in a separate study demonstrating that higher ACE2 expression resulted in a higher CD8+ T cell response in patients. The expression of ACE2 is associated with other comorbidities that increase the risk and, subsequently, the likelihood of experiencing a worse outcome after SARS-CoV-2 infection, such as cardiovascular disease, hypertension, chronic obstructive pulmonary disease, and obesity [17]. Generally, mild to moderate infections would more likely result in subacute thyroiditis and painless, destructive thyroiditis in hospitalized patients with a more severe infection. Beyond an aberrant host immune response to the infection, there are different pathogenic mechanisms by which the SARS-CoV-2 can induce autoimmunity [18]. One such method is molecular mimicry. Although the mechanism is unknown, there have been reports of shared characteristics between SARS-CoV-2 spike protein and various endocrine cells. One study analyzed 14 pentapeptides shared by the SARS-CoV-2 spike protein with several organs, including the thyroid, pituitary, adrenal cortex, and pancreatic beta islet cells, with the thyroid sharing the highest amount. These similarities and genetic predisposition could explain the underlying pathophysiology in which autoimmunity, especially relating to these organs, could occur [18]. With the association between SARS-CoV-2 and autoimmune diseases, it would not be surprising to observe a shift in the incidence of these disorders.
Although more large-scale data are yet to be published, several reports have investigated the incidence of reported auto-immune cases since the pandemic’s start. In a matched cohort study of 641 704 patients with COVID-19, researchers found the infected groups had a higher likelihood of acquiring autoimmune diseases [19]. A retrospective review found similar results in the onset of GD in a pediatric population, in which the incidence of new GD diagnosis doubled from 1.3% to 2.6% during the pandemic [20]. Although cases like ours suggest a relationship between SARS-CoV-2 infection and autoimmune thyroid disorders after infection, long-term data sets must be analyzed to understand any correlation fully. Until there is a full understanding of the correlation, medical decision-making to initiate an early workup of potential autoimmune disorders should have a lower threshold in the era of COVID-19.
Conclusions
Our case demonstrates the importance of recognizing COVID-19 as an etiology or a trigger for the new onset or exacerbation of GD. Even though our patient presented with typical features of GD, this case highlights the importance of being vigilant to recognize this association between COVID-19 and thyroid abnormalities for early diagnosis, treatment, and appropriate long-term care.
References:
1.. Zacharias H, Dubey S, Koduri G, D’Cruz D, Rheumatological complications of COVID 19: Autoimmun Rev, 2021; 20(9); 102883
2.. Alahyari S, Moradi M, Rajaeinejad M, Jalaeikhoo H, Post-COVID-19 hematologic complications: A systematic review: Expert Rev Hematol, 2022; 15(6); 539-46
3.. Pimentel V, Luchsinger VW, Carvalho GL, Guillain-Barré syndrome associated with COVID-19: A systematic review: Brain Behav Immun Health, 2023; 28; 100578
4.. Nassar M, Nso N, Baraka B, The association between COVID-19 and type 1 diabetes mellitus: A systematic review: Diabetes Metab Syndr, 2021; 15(1); 447-54
5.. Naguib R, Potential relationships between COVID-19 and the thyroid gland: An update: J Int Med Res, 2022; 50(2); 3000605221082898
6.. Mohammed SR, Tripathi M, Mack N, Teelucksingh S, Relapse of Graves’ disease following SARS-CoV-2 infection: A case report and brief literature review: Med Int (Lond), 2021; 1(5); 25
7.. Damara FA, Muchamad GR, Ikhsani R, Thyroid disease and hypothyroidism are associated with poor COVID-19 outcomes: A systematic review, meta-analysis, and meta-regression: Diabetes Metab Syndr, 2021; 15(6); 102312
8.. Inaba H, Aizawa T, Coronavirus disease 2019 and the thyroid – progress and perspectives: Front Endocrinol (Lausanne), 2021; 12; 708333
9.. Brancatella A, Viola N, Santini F, Latrofa F, COVID-induced thyroid autoimmunity: Best Pract Res Clin Endocrinol Metab, 2023; 37(2); 101742
10.. Sullivan K, Helgeson J, McGowan A, COVID-19 Associated thyroid storm: A case report: Clin Pract Cases Emerg Med, 2021; 5(4); 412-14
11.. Milani N, Najafpour M, Mohebbi M, Case series: Rare cases of thyroid storm in COVID-19 patients: Clin Case Rep, 2021; 9(9); e04772
12.. Li MY, Li L, Zhang Y, Wang XS, Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues: Infect Dis Poverty, 2020; 9(1); 45
13.. Chen M, Zhou W, Xu W, Thyroid function analysis in 50 patients with COVID-19: A retrospective study: Thyroid, 2021; 31(1); 8-11
14.. Durgun C, Durgun M, Evaluation of thyroid function tests in patients with COVID-19: Cureus, 2023; 15(6); e40628
15.. Lui DTW, Lee CH, Chow WS, The independent association of TSH and free triiodothyronine levels with lymphocyte counts among COVID-19 patients: Front Endocrinol (Lausanne), 2022; 12; 774346
16.. Coperchini F, Ricci G, Croce L, Modulation of ACE-2 mRNA by inflammatory cytokines in human thyroid cells: A pilot study: Endocrine, 2021; 74(3); 638-45
17.. Kaseb AO, Mohamed YI, Malek AE, The impact of angiotensin-converting enzyme 2 (ACE2) expression on the incidence and severity of COVID-19 infection: Pathogens, 2021; 10(3); 379
18.. Churilov LP, Normatov MG, Utekhin VJ, Molecular mimicry between SARSCoV-2 and human endocrinocytes: A prerequisite of post-COVID-19 endocrine autoimmunity?: Pathophysiology, 2022; 29(3); 486-94
19.. Tesch F, Ehm F, Vivirito A, Incident autoimmune diseases in association with SARS-CoV-2 infection: A matched cohort study: Clin Rheumatol, 2023; 42(10); 2905-14 [Erratum in: Clin Rheumatol. 2023;42(10):2919–20
20.. Donner JR, Has P, Topor LS, Increased incidence and severity of new Graves disease diagnoses in youth during the COVID-19 pandemic: Endocr Pract, 2023; 29(5); 349-52
In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250