15 April 2024: Articles 
A 25-Year-Old Man with a History of Substance Abuse Presenting with Pneumomediastinum Due to Methamphetamine Vapor Inhalation
Challenging differential diagnosis, Diagnostic / therapeutic accidents, Unusual setting of medical care, Educational Purpose (only if useful for a systematic review or synthesis), Rare coexistence of disease or pathology
Anahita Shahnazi1ABCDEF*, Keenan Bayrakdar1BDEF, Prospero Cortorreal1D, Katharine Burmaster1D, Gretchen Junko1DFDOI: 10.12659/AJCR.941509
Am J Case Rep 2024; 25:e941509
Abstract
BACKGROUND: There has been an increase in the use of inhalation methods to abuse drugs, including freebasing crack cocaine (alkaloid) and inhaling methamphetamine vapor. This report is of a 25-year-old man with a history of substance abuse presenting with pneumomediastinum due to methamphetamine vapor inhalation. Acute pneumomediastinum is an extremely rare complication of methamphetamine use.
CASE REPORT: A 25-year-old man was treated for polysubstance abuse following 9 days of methamphetamine abuse. EKG did not show any ST &T change. D-dimer was normal, at 0.4 mg/L, so we did not do further work-up for pulmonary embolism. His chest pain worsened in the Emergency Department (ED), and a physical exam demonstrated crepitation of the posterior neck, trapezius, and right scapula. A portable chest X-ray revealed subcutaneous air over the right scapular region, in addition to pneumomediastinum. The urine drug screen test was positive for methamphetamine. A chest CT was ordered, which showed a moderate-volume pneumomediastinum with soft-tissue air tracking into the lower neck and along the right chest wall. The patient underwent an esophagogram, which showed no air leak, and Boerhaave’s syndrome was ruled out. His symptoms improved and he did not require any surgical intervention.
CONCLUSIONS: Considering the higher rates of illicit substance use, especially methamphetamine, it is important to pay attention to the associated pathologies and to keep spontaneous pneumomediastinum on the list of differentials for patients using methamphetamine, particularly those who inhale it, which can cause pneumomediastinum, even without Boerhaave’s syndrome.
Keywords: illicit drugs, Methamphetamine, Pneumomediastinum, Diagnostic
Introduction
There has been an increase in the use of inhalation methods to abuse drugs, including freebasing crack cocaine (alkaloid) and inhaling methamphetamine vapor. Pneumomediastinum is defined as the presence of air in the mediastinum. Acute pneumomediastinum is a benign condition usually caused by alveolar rupture with subsequent air tracking along the tracheobronchial tree [1]. Acute pneumomediastinum is rare, with an incidence of 0.001–0.01% among all adult patients [2] and it is an extremely rare complication of methamphetamine use caused by the Valsalva maneuver after inhalation [2–4]. Changes in intrathoracic pressure can lead to alveolar rupture and dissection of air along the tracheobronchial tree [5]. Intravenous methamphetamine use increases several inflammatory markers that can make the alveolar wall more fragile and increase the risk of acute pneumothorax and pneumomediastinum [6,7]. This report is of a 25-year-old man with a history of substance abuse presenting with pneumothorax and pneumomediastinum due to methamphetamine vapor inhalation.
Case Report
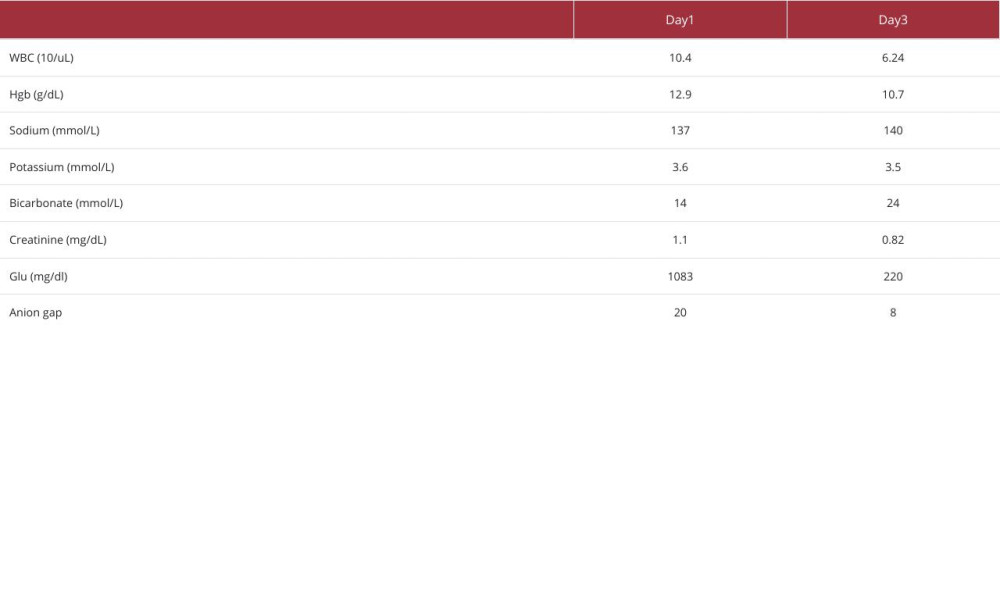
A 25-year-old man with a past medical history of polysubstance abuse presented to the ED for evaluation of weakness, depression, and pleuritic chest pain following a 9-day substance abuse binge with methamphetamine. He did not take any medicines at home. He claimed he did not sleep during this time. While awaiting psychiatric evaluation, basic laboratory test results revealed WBC 10 400/uL, Hgb 12.9, Plt 426, Na 137 mmol/L, K 3.6 mmol/L, Cr 1.1 mg/dL, and troponin 4 ng/L. EKG did not show any changes in ST or T waves. A urine drug test was positive for methamphetamine.
The patient was treated with IV fluids and pain medicine. D-dimer was in the normal range, so we did not do further work-up for pulmonary embolism. He began having worsening chest pain and dyspnea. The physical exam demonstrated crepitation of the posterior neck, right trapezius, and right scapula. Further work-up of chest pain was done with portable chest X-ray equipment, which revealed subcutaneous air over the right scapular region and pneumomediasti (Figure 1).
A chest CT was ordered on the first day, which showed a moderate-volume pneumomediastinum extending into the supraclavicular fossa along the right chest wall. The central airways were patent, and there was no pleural separation suggestive of pneumothorax (Figure 2). The patient had vomited several times the day before admission, raising concerns about Boerhaave’s syndrome. The gastrointestinal service was consulted on day 2, and the patient underwent a Gastrografin esophagogram that showed no contrast leak, and Boerhaave’s syndrome was ruled out. His symptoms improved during admission, and he did not need surgical intervention. The results of lab work at discharge on day 3 is shown in Table 1.
Discussion
The importance of taking a drug abuse history, especially the method used, cannot be overstated. Several pulmonary complications are associated with drug abuse, including pneumonia, septic emboli, and pneumothorax. However, acute pneumomediastinum is a rare complication of methamphetamine abuse and there are few in the literature. Pulmonary adverse effects, even rare ones, need to be considered when evaluating patients who inhale illicit drugs [2,3].
A chest X-ray or CT is sufficient for the diagnosis of acute pneumothorax in the absence of high-risk factors. It is necessary to perform an esophagogram when high-risk features are present. A contrast swallow study should be performed for patients with emesis, dysphagia, gastrointestinal disease, trauma, hemodynamic instability, fever, leukocytosis, pleural effusion, or pneumoperitoneum [8].
Our patient had vomited repeatedly on the day before admission, so we were concerned about Boerhaave’s syndrome contributing to pneumomediastinum, but the esophagogram did not confirm Boerhaave’s syndrome and we did not find any other etiology for his acute pneumomediastinum, which appears to have been drug-induced pneumomediastinum in the setting of vomiting without Boerhaave’s syndrome. Management is generally conservative with pain control, rest, and oxygen as needed. Surgical intervention in the case of an esophageal rupture may include a stent or esophageal repair [2].
Conclusions
Considering the higher rates of illicit substance abuse, especially methamphetamine, it is important to pay attention to the associated pathologies. It is important to keep acute pneumomediastinum on the list of differentials for patients using this drug, particularly those who inhale methamphetamine, which can cause pneumomediastinum even without Boerhaave’s syndrome. A thorough history of abuse of drugs such as methamphetamine and whether inhalation methods were used is very important for these patients.
Figures
References:
1.. Caceres M, Ali S Z, Braud R, Spontaneous pneumomediastinum: A comparative study and review of the literature: Ann Thorac Surg, 2008; 86(3); 962-66
2.. Albanese J, Gross C, Azab M, Spontaneous pneumomediastinum: A rare complication of methamphetamine use: Respir Med Case Rep, 2017; 21; 25-26
3.. Luck D, Munyon R, Bilateral spontaneous pneumothoraces with spontaneous pneumomediastinum: An intravenous methamphetamine complication: Respir Med Case Rep, 2018; 25; 4-5
4.. Lee JS, Overview of pulmonary disease in people who inject drugs: UpToDate April, 2023 Available from URL: https://www.uptodate.com/contents/overview-of-pulmonary-disease-in-people-who-inject-drugs
5.. Agustin M, David G, Kang JY, Spontaneous pneumomediastinum and diffuse subcutaneous emphysema after methamphetamine inhalation: Case Rep Pulmonol, 2020; 2020; 7538748
6.. Chen GA, Chen Y, Late diagnosis of methamphetamine inhalation related pneumothorax, pneumomediastinum and diffuse subcutaneous emphysema: A case report: J Acute Med, 2018; 8(1); 30-33
7.. Fajardo LL, Association of spontaneous pneumomediastinum with substance abuse: West J Med, 1990; 152(3); 301-4
8.. Al-Mufarrei BJ, Badar J, Gharagozloo F, Spontaneous pneumomediastinum: Diagnostic and therapeutic interventions: J Cardiothorac Surg, 2008; 3; 59
Figures
In Press
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250