17 April 2024: Articles 
Successful Treatment Strategy for Duplicate Inferior Vena Cava and Deep Venous Thrombosis: Filter Placement and Thrombolysis Approach
Unusual clinical course, Rare coexistence of disease or pathology
Xu LanDOI: 10.12659/AJCR.942578
Am J Case Rep 2024; 25:e942578
Abstract
BACKGROUND: Duplicate inferior vena cava (IVC) accompanied by deep venous thrombosis is rare. The optimal treatment plan is determined according to the results of imaging, including venography. In this report, we present a case of successful treatment of a patient with duplicate IVC and deep venous thrombosis (DVT).
CASE REPORT: An 84-year-old man with history of hypertension was admitted to the hospital because of 4 days of moderate left lower-limb edema. A thorough examination led to the diagnosis of the DVT. The duplicate IVC was discovered during venography. As the blood from the left common iliac vein mainly flowed to the left IVC, and there were no other communicating branches before the convergence of the left and right IVCs, which was located above the 1st lumbar vertebrae body near the junction of the hepatic vein and the IVC, the strategy of placing only 1 filter in the left inferior vena cava were chosen, rather than placing 1 filter above the confluence of bilateral IVC, or placing a filter in each IVC below the level of renal veins on each side. Following that, the DVT was safely treated with thrombolysis and aspiration without the risk of pulmonary embolism.
CONCLUSIONS: This case report presented the complete evaluation and management of a patient with lower-limb DVT accompanied by the malformation of duplicate IVC. The filter placement strategy with duplicate IVC in the literature was summarized. We concluded that even in emergency situations, with comprehensive consideration, it is possible to perform endovascular intervention successfully and achieve satisfactory treatment results.
Keywords: Venous Thrombosis, Vena Cava, Inferior, Vena Cava Filters, Mechanical Thrombolysis
Introduction
Duplicate inferior vena cava (IVC) is rare, with an incidence rate of 0.2–3%. This congenital vascular malformation is caused by incomplete regression of abdominal veins in the embryonic period. There are 2 main types of duplicate IVC on imaging pattern [1]. Generally, 2 IVCs are located on both sides of the abdominal aorta [2]. It generally has no obvious symptoms, and is often incidentally discovered during surgery or examination [3]. There is also risk of deep venous thrombosis (DVT) and pulmonary embolism (PE) in patients with congenital IVC malformations [4].
Lower-limb DVT is known to occur in patients with major surgery, trauma, limb immobilization, long-term bed rest, and malignant tumors. Lower-limb edema is the predominant symptom. If the thrombus dislodges, it can cause acute PE, which in serious situations can be fatal. Delayed treatment of lower-limb DVT can result in long-term complications, such as chronic thromboembolic pulmonary hypertension and post-thrombotic syndrome, which have a significant negative impact on a patients’ quality of life [5]. Early thrombolysis and aspiration treatment can successfully reduce symptoms such as lower-limb edema, pain, high skin temperature, and dilation of superficial veins in patients with acute lower-limb DVT. Additionally, the likelihood of long-term venous problems such as post-thrombotic syndrome can usually be decreased by early deep venous recanalization in the lower limbs. By blocking the embolization caused by the patient’s activity or thrombolytic aspiration, the placement of the IVC filter can avoid fatal PE [6].
However, for patient with lower-limb DVT accompanied by duplicate IVC, there are different strategies for placing IVC filters based on the type of IVC malformations: 1 filter above the confluence of bilateral IVC, 1 filter in each IVC below the level of renal veins on each side, or 1 filter in blood and thrombus reflux IVC below the level of the renal veins. For the selection of the placement strategy, an adequate analysis of the patient’s condition and anatomy is required before placement of an IVC filter.
Case Report
An 84-year-old man was admitted to the hospital with 4 days of moderate left lower-limb edema and sensation of heaviness. He denied any history of trauma. He had a past history of hypertension, without regular medication administration. The rest of the review of systems was negative. He had no family history of heart, kidney, or other diseases. He denied use of any medications, tobacco, alcohol, or other substances.
Physical examination on admission showed the heart rate was 88 beats per minute, the blood pressure was 142/79 mmHg, the respiratory rate was 20 breaths per minute, and the pulse oximetry was 99%. No abnormalities were found in the cardiac, pulmonary, and abdominal examinations. The skin color of the left lower limb was slightly purple and dark, without skin ulcers or pigmentation. The skin temperature of the left lower limb was normal. Only edema of the ankle and dorsum of the foot was found. The skin color and temperature of the right lower limb were normal, without edema. The laboratory examination showed that the white blood cell count was 4.56 (normal value: 3.5–9.5)×109/L with 52.5% neutrophils (normal value: 40–75%), hemoglobin 105 (normal value: 130–175) g/L, platelets 112 (normal value: 125–350)×109/L, C reactive protein 7.9 (normal value: 0–3) mg/L, and albumin 36 (normal value: 40–55) g/L. The coagulation and thrombosis examination showed D-Dimer was 5.46 (normal value: 0–0.55) mg/L, fibrinogen degradation product 13.7 (normal value: 0–5) μg/mL, thrombin-antithrombin complex 6.98 (normal value: 0–4.08) ng/mL, and plasmin-antiplasmin complex 1.32 (normal value: 0–0.85) μg/mL.
The electrocardiogram, echocardiography, and abdominal ultrasound were normal. A lower-limb venous ultrasound found that the left common femoral vein, femoral vein, and popliteal vein lumen were dilated, with poor internal sound transmission. The inner diameter of the intermuscular vein in the left calf has widened by about 0.6 cm, with poor internal sound transmission and hypoechogenicity. No ultrasound abnormalities were found in the right lower limb. The patient was diagnosed with extensive deep vein thrombosis of the left lower limb.
After subcutaneous injection of the low-molecular-weight heparin, IVC filter placement and left lower-limb deep venous thrombolysis were performed. With the patient in a supine position, the right femoral vein was selected for access. During IVC venography, we found that the patient’s IVC was divided into 2 branches, located on both sides of the spine. The right IVC was notably narrow compared to the left IVC. The 2 branches formed a connection at the level of the 5th lumbar vertebral body, and the left communicating branch was higher than the right branch. Venography showed that there were no other communicating branches before the convergence of the left and right IVCs. The blood from the right common iliac vein simultaneously flowed to both IVCs, while the blood from the left common iliac vein mainly flowed to the left IVC (Figure 1A). The venography showed that the left renal vein converged into the left IVC below the 1st lumbar vertebrae body, and merged to the right IVC (Figure 1B). Based on the above, we decided to place an IVC filter (Option Retrievable Vena Cava Filter System, Rex Medical, Conshohocken, PA, USA) in the left IVC below the junction of the renal vein between the 3rd and 4th lumbar vertebrae (Figure 2A). Figure 2B is a pattern diagram showing the shape of the IVC and the placement of the IVC filter.
Subsequently, the patient was transitioned to prone position and the left lower-limb popliteal vein was accessed. Venography revealed extensive thrombosis in the left popliteal vein, fem-oral vein, external iliac vein, and common iliac vein. Contrast was unable to pass through the deep venous system, but many collateral veins were noted (Figure 3A). The AngioJet Ultra AVX Thrombectomy Set (Boston Scientific, Marlborough, MA, USA) was used for thrombolysis and aspiration treatment of DVT in the left lower limb. After treatment, the venography showed contrast flowing through the now patent left lower-limb deep veins (Figure 3B). IVC venography after treatment showed some thrombus under the filter. The blood flow from the left iliac vein returned only to left IVC, and no communicating branches were found between the left and right IVCs (Figure 3C). After surgery, anticoagulant therapy with rivaroxaban (20 mg, once a day) was given. One week after surgery, the left lower-limb edema had significantly alleviated, and the coagulation indicators were rechecked, showing D-Dimer 2.08 mg/L and the fibrinogen degradation product was 6.01μg/mL. Extensive evaluations for chronic infections and possible cancers found no positive results.
Discussion
We present the diagnosis and treatment of a case of DVT in the left lower limb with duplicate IVC. In this case, the patient was elderly and admitted due to unilateral lower-limb edema. The symptoms of DVT in the lower limb were quite typical, and diagnosis was made by ultrasound of the lower-limb veins. Due to the acute presentation of DVT, to prevent the occurrence of potentially fatal PE, urgent surgery was considered after surgical contraindications were excluded. As a result, preoperative assessment of the IVC was deferred; instead, intraoperative venography was used for IVC evaluation. Therefore, the patient’s IVC abnormality was not identified before, resulting in failure to conduct more in-depth examinations and surgical planning.
Intraoperative venography showed the left IVC was larger than the right and was mainly responsible for the venous return of the left lower limb and relatively high venous return to the heart. However, in this case, the thrombus had formed in the left lower limb. The reason for this may be related to the location of the left IVC confluence. The left IVC of this patient crossed midline between the abdominal aorta and the superior mesenteric artery, converging with the right IVC at the position of the 1st lumbar vertebral body. As a result, the left IVC may have been compressed and stenotic, leading to poor, slow, or stagnant venous blood flow [7]. Since the left IVC was responsible for draining the venous return from left lower limb, the poor blood flow may have ultimately lead to formation of the thrombosis [5].
The treatment plan for lower-limb DVT is well defined. However, the discovery of rare cases of duplicate IVC during intervention poses more challenges for treatment. In this case, besides the current filter placement strategy employed, there were 2 other strategies that can be considered: place 1 filter above the confluence of bilateral IVC [8], or place 1 filter in each IVC below the level of the renal veins on each side [9].
For the first strategy, the advantage was that 1 filter could fully intercept thrombi from both IVC veins and avoid the occurrence of PE. However, in this case, the confluence of the bilateral IVC was located above the 1st lumbar vertebrae body requiring the filter be placed above the 12th thoracic vertebrae body. If the thrombus embolized, there would be a possibility of renal vein embolism causing venous obstruction and renal dysfunction. Also, if the filter was placed at the junction of the hepatic vein and the IVC, this might lead to the filter placement failure or reflux obstruction of hepatic vein. Therefore, this strategy was not chosen.
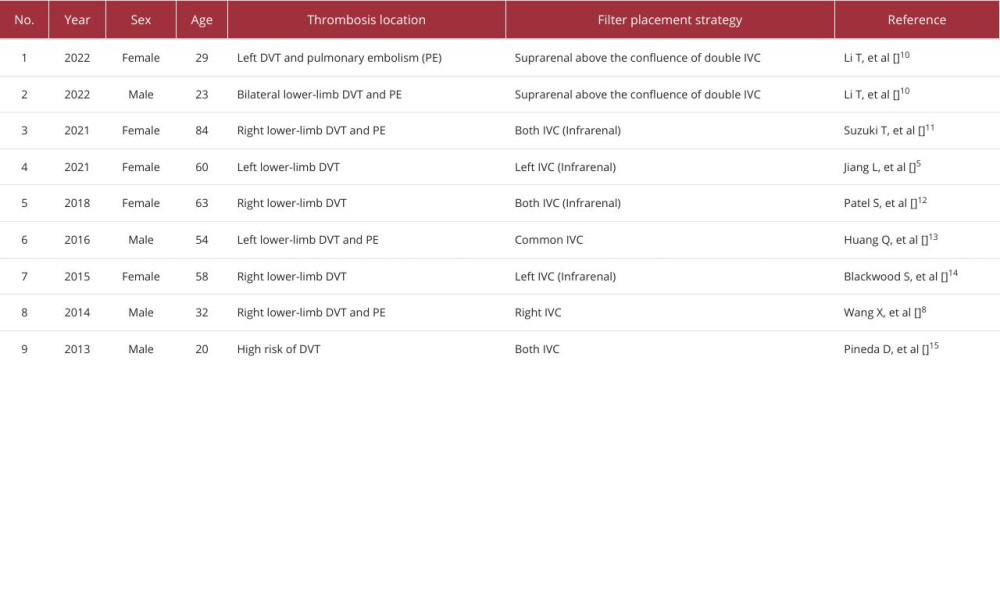
For the second strategy, the advantage was that thrombus embolization from the lower-limb deep veins could be fully intercepted without affecting venous return from the renal veins. However, in this case the right IVC was very narrow, which could limit full filter expansion and there was no small filter that could be used in an emergency. Based on the above reasons and after comprehensive consideration, we chose our specific treatment plan. Other patients with different anatomy or different thrombotic events will require customized treatment regimens. We have summarized the literature of the case reports on filter placement strategy with duplicate IVC in Table 1.
After placement of the filter, thrombolysis and aspiration treatment were performed through the popliteal vein to help preserve deep venous valve function. However, the thrombosis below the popliteal vein was difficult to clear, which required postoperative anticoagulant therapy. For the anticoagulant therapy, low-molecular-weight heparin and rivaroxaban were used before and after surgery, respectively, as the adverse effects of bleeding and hepatic-induced thrombocytopenia caused by these drugs are relatively minor. The treatment was successful and there was no occurrence of pulmonary, other embolism, or bleeding. With deep vein recanalization and postoperative anticoagulation, the residual thrombus gradually resolved, lower-limb edema was alleviated, and the long-term risk of DVT syndrome was greatly reduced.
Our study has certain limitations. Firstly, for the diagnosis of disease, decreased hemoglobin and platelets, as well as slightly elevated C reactive protein, all suggest the possibility of immune diseases. Although the treatment of DVT is important, the etiology of thrombosis still needs to be determined through relevant examinations to prevent disease progression and recurrence of thrombosis. Secondly, for the right IVC, the possibility of an ascending lumbar vein cannot be ruled out in this case, but this hypothesis was difficult to confirm because we were unable to perform a CT scan after the treatment. Compared to normal IVC, our patient’s right IVC was relatively narrow, but if it was an ascending lumbar vein, no communicating branches would be found with the other lumbar vein.
However, regardless of which vessel it was, the assisting effect of this vessel on the right lower-limb blood return would be the same. Thirdly, although no other communicating branches were found before the convergence of the left and right IVCs under venography, small communicating branches were difficult to detected under the background of the spine.
Conclusions
In this case report we present the entire diagnosis and treatment process of a patient with lower-limb DVT in the presence of congenital IVC duplication. Through adequate analysis of the patient’s lower-limb venous return with venography, a suitable endovascular strategy was quickly formulated, and a satisfactory treatment result was ultimately achieved. Although similar cases have been reported before, our successful treatment could provide new treatment ideas for duplicate IVC with DVT.
Figures
References:
1.. Ang WC, Doyle T, Stringer MD, Left-sided and duplicate inferior vena cava: A case series and review: Clin Anat, 2013; 26(8); 990-1001
2.. Mutavdzic P, Dragas M, Galun D, Recurrent deep venous thrombosis of lower extremities as a result of compression of large horseshoe kidney cysts in double inferior vena cava – successfully treatment with sclerotherapy: Vascular, 2023; 31(3); 603-7
3.. Chaud GJ, Lacombe L, Dagenais F, Double inferior vena cava systems during retroperitoneal surgery: Description of a systematic approach to a rare and challenging anatomic variant: J Vasc Surg Cases Innov Tech, 2022; 8(1); 81-84
4.. Li WR, Feng H, Jin L, Duplication of the inferior vena cava: A case series: J Int Med Res, 2022; 50(5); 3000605221100771
5.. Jiang L, Yang CF, Lin J, Filter implantation for double inferior vena cava: A case report and literature review: World J Emerg Med, 2021; 12(4); 332-34
6.. Qi YH, Wang T, Wang J, Yuan D, Inferior vena cava filter reduces pulmonary embolism but does not increase deep venous thrombosis: A systematic review and meta-analysis: Asian J Surg, 2022; 45(1); 592-93
7.. Omori A, Katayama K, Saiki R, Disruption of the glomerular basement membrane associated with nutcracker syndrome and double inferior vena cava in Noonan syndrome: A case report: BMC Nephrol, 2022; 23(1); 65
8.. Wang X, Chen Z, Cai Q, Catheter-directed thrombolysis for double inferior vena cava with deep venous thrombosis: A case report and literature review: Phlebology, 2014; 29(7); 480-83
9.. Sartori M, Zampieri P, Andres A, Double vena cava filter insertion in congenital duplicated inferior vena cava: A case report and literature review: Haematologica, 2006; 91(6); e85-e86
10.. Li T, Wang Q, Wang W, One filter may be enough for duplicate inferior vena cava filter implantation in patients with deep venous thrombosis: Two cases report: Medicine (Baltimore), 2022; 101(52); e32480
11.. Suzuki T, Fujino S, Aoyama T, Double inferior vena cava filter implantation in a patient with duplication of the inferior vena cava: J Vasc Surg Cases Innov Tech, 2021; 7(3); 520-23
12.. Patel S, Cheema A, Karawadia T, Carson M, Management of acute lower extremity deep venous thrombosis in a patient with duplicated inferior vena cava and contraindication to anticoagulation: case and review of the literature: BMJ Case Rep, 2018; 2018; bcr2017222974
13.. Huang Q, Zhang Q, Xu H, Catheter-directed thrombolysis for massive pulmonary embolism resulting from thrombosis in a duplicated inferior vena cava: A case report: Ann Vasc Surg, 2016; 33; 231.e1-4
14.. Blackwood S, Hsu R, Angiojet thrombolysis and vena cava filter insertion in a case of a duplicated inferior vena cava: SAGE Open Med Case Rep, 2015; 3; 2050313 X15570649
15.. Pineda D, Moudgill N, Eisenberg J, An interesting anatomic variant of inferior vena cava duplication: Case report and review of the literature: Vascular, 2013; 21(3); 163-67
Figures
In Press
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250