24 April 2024: Articles 
Laparoscopic Sleeve Gastrectomy with Staple-Line Oversewing in a Patient with Factor XI Deficiency: A Case Report
Challenging differential diagnosis, Diagnostic / therapeutic accidents, Unusual setting of medical care, Congenital defects / diseases
Lorenza Beomonte ZobelDOI: 10.12659/AJCR.942824
Am J Case Rep 2024; 25:e942824
Abstract
BACKGROUND: Bariatric surgery (BS) has a lower percentage of complications than other abdominal surgeries. Hemorrhage in one of the most common complications and can be life-threatening. Hereditary factor XI (FXI) deficiency is a coagulation disorder that can result in excessive bleeding requiring intervention to restore hemostasis. Risks over benefits in patients with morbid obesity with BS indication, as well as those with FXI deficiency, should be carefully evaluated. This article reports the case of an obese woman with FXI deficiency undergoing SG.
CASE REPORT: A 49-year-old woman with a BMI of 51 kg/m² was diagnosed as having severe FXI deficiency during preoperative exams prior to bariatric surgery. Virus-inactivated homo-group plasma 10 ml/kg infusion was administrated 1 h before surgery, during the entire procedure, and continuing until postoperative day (POD) 4. A very low-calorie ketogenic diet (VLCKD) was proposed to the patient 4 weeks before surgery. Laparoscopic sleeve gastrectomy was performed with staple-line reinforcement by oversewing the seromuscular layer using continuous suture. Subcutaneous enoxaparin 4000 U.I. was administered from POD 1 until POD 25 to prevent any thromboembolic event. The patient was discharged on POD 5 in good clinical condition.
CONCLUSIONS: Risks of bleeding and\or thromboembolic events before or after BS are increased in patient with FXI deficiency. Bariatric surgery in these patients is safe in experienced BS centers, and the risks associated with the obesity seem to exceed those of the coagulopathy and surgery. Careful preoperative counseling, extensive hematological checks, and meticulous surgery are essential to reduce BS risks. Sleeve gastrectomy oversewing the stapler line seems a reasonable choice.
Keywords: Bariatric Surgery, Bariatrics, Blood Coagulation Disorders, Factor XI, Factor XI Deficiency
Introduction
Bariatric surgery (BS) is a safe and effective long-term treatment for severe obesity that results in long-term weight loss and improvement and remission of obesity-related comorbid conditions [1].
Bariatric surgery has fewer complications than other abdominal surgeries. Hemorrhage in one of the complications that can be life-threatening, occurring in 1.3–1.7% of bariatric surgeries and being more common in gastric bypass than in sleeve gastrectomy (SG) and gastric banding [2]. Hemorrhagic complications are usually the result of bleeding along the staple line. However, there are other sources of bleeding, typical of BS: the omentum is thicker than usual, often friable and inflamed; the abdominal wall is deep and the abdominal cavity more difficult to access; and for a SG, all the short gastric vessels are divided after coagulation [3].
Despite this recognizable risk of bleeding, thromboembolic complications too continue to be a significative cause of morbidity and mortality after BS [4]. To avoid this risk, the ASMBS guidelines suggests thromboprophylaxis, including unfractionated heparin or low-molecular-weight heparin (LMWH), for all patients after BS [5], to be continued for 15 days after surgery, as recommended by the society for Enhanced Recovery After Surgery (ERAS) [6].
Hereditary FXI deficiency is a coagulation disorder that can result in excessive bleeding requiring intervention to restore hemostasis. It has a variable bleeding phenotype despite the presence of very low levels, and it can be identified by excessive bleeding in association with injury, trauma or surgery, or during routine pre-surgical laboratory evaluation [7,8].
Clinical symptoms include bleeding provoked by a surgical hemostatic challenge, postinjury, epistaxis, and heavy menstrual bleeding. Unprovoked bleeding episodes that are frequently seen in patients with severe deficiency of Factors VIII or X, such as hemarthroses, muscle bleeds, or soft-tissue bleeds, are not frequently observed in severe FXI deficiency [9].
This article reports the case of a woman with FXI deficiency undergoing SG. Clinical indications, perioperative management, and outcomes are discussed.
Case Report
A 49-year-old woman with a BMI of 51 kg/m2 (weight: 128 kg, height: 1.58 m), consulted our obesity outpatient clinic to explore the possibility of having BS. She had never undergone surgery before. She had no history of increased bleeding from the gums or trivial trauma, nor episodes of nosebleeds.
After evaluating her medical history and eating habits, laparoscopic SG was planned. She underwent preoperative exams, including electrocardiogram, chest X-ray, thyroid function tests, lung function tests, sleep study, esophago-gastro-duodenos-copy, and abdominal ultrasound.
The laboratory parameters were within the normal range; routine tests to evaluate hemostasis revealed normal prothrombin time (PT ratio 1.2) and a prolongation of activated partial thromboplastin time (APTT ratio: 2.57); and severe FXI deficiency (9%) was identified. Other coagulation factors (including Factors IX, X, and XII) were within normal ranges. Therefore, she was referred to the Hemophilia Unit for diagnostic investigation. She underwent bleeding time and clotting time tests, resulting in 16-min clotting time (prolonged clotting time) and a bleeding time of 12 min (prolonged bleeding time). The hematological consultation did not contraindicated surgery, but she was prescribed a virus-inactivated homo-group plasma 10 ml/kg to be given in infusion 1 h before surgery and continued during the entire procedure and until the POD 4. A modest weight loss of 5–10% in the immediate preoperative period was suggested to reduce the risk of complications. A very low-calorie ketogenic diet (VLCKD) was proposed to the patient 4 weeks before surgery and she lost 14 kg (BMI 45 kg/m2, weight 114 kg).
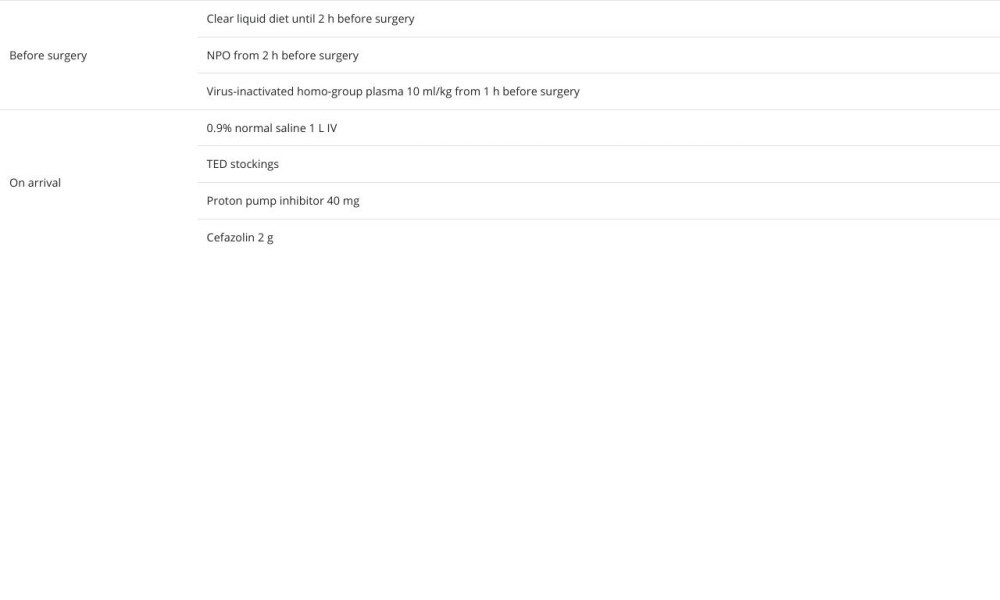
Before surgery, she wore TED compression stockings. Preoperative optimization was done with proton pump inhibitor 40 mg, Cefazolin 2 g, and starting intravenous plasma infusion from 1 h before starting the procedure (total amount, 1.1140 L). Approximately 500–700 mL of Ringer’s lactate were given intravenously during the procedure, with boluses given depending on intraoperative vital signs [10] (Table 1).
Laparoscopic sleeve gastrectomy was performed under general anesthesia, with the patient in a supine position (Video 1): a pneumoperitoneum of 14 mmHg induced through Veress’ needle in Palmer’s point was maintained throughout the entire procedure to allow optimal surgical exposure without significant modifications of hemodynamics. The operation was carried out using 4 operative trocars: one 12-mm port each in the right and left flank, one 5-mm port below the xyphoid, and one below the 12-mm port in the left flank. A camera was inserted in the 12-mm port in the epigastrium. Commencing 5 cm from pylorus, all the short gastric vessels were divided using advanced bipolar energy. The stomach was stapled over a calibrating bougie (38F) from the port at the right upper quadrant. Traction from the left trocar was important to clear the fundus from the gastric tube. Staple-line reinforcement was done by oversewing the seromuscular layer using 3/0 continuous barbed suture. The hemostasis was further ensured by bipolar electrocoagulation. Methylene blue test at the end of the procedure confirmed no signs of leaks nor stenosis. The transected stomach was removed via the port on the left flank. In all the 10-mm ports, the abdominal fascia was sutured using absorbable sutures. Skin incisions were approximated using monofilament. The operative time was 67 min and intraoperative blood loss was scant; nevertheless, 1 g\L of hemoglobin was lost in the first postoperative day and remained stable throughout the 5 days of her hospital stay.
The postoperative course was uneventful. The patient remained stable, with her intravenous plasma infusion for the entire in-hospital recovery, as prescribed; full blood count and hemostasis tests were checked twice and before discharge. Subcutaneous enoxaparin 4000 U.I. was administered from POD 1 until POD 25 to prevent thromboembolic events. She did well, without postoperative nausea or vomiting, and was able to tolerate clear fluids from POD 1. Pain control was guaranteed using paracetamol 1 g 3 times a day. She was discharged on POD 5 in good clinical condition, with instructions to change food consistency gradually and progressively, from clear fluids to creamy foods and then to solid chewable items over a period of 2–4 weeks. She was told to stop wearing TED stockings, and mobility and exercise were also recommended. Routine daily multivitamin and mineral supplementation were prescribed, as usual.
One month after discharge, she had lost 14 kg and her BMI fell 40.16 kg/m2. No hematological complications, such as bruises or petechiae were recorded. The patient stopped taking enoxaparin 21 days after discharge. After 3 months, she had lost 19 kg and her BMI was 32.53 kg/m2.
Discussion
Excessive body weight has adverse effects on cardiovascular, respiratory, and musculoskeletal systems; it also affects the metabolism of both non-hemophilic and hemophilic patients. Bariatric surgery in patients with FX1 deficiency is not contraindicated and patients with this condition should not be discouraged to undergo BS, because their obesity is the most morbid of the 2 conditions; furthermore, there are limited data on BS in patients with clotting disorders. One patient with hemophilia A underwent a successful SG [11], and 1 had a one-anastomosis gastric bypass (OAGB) [12]. Davulcu et al reported SG performed in a patient with severe hemophilia A who underwent re-operation on POD 1 because of hemoperitoneum [13].
There is only 1 other report of BS in a patient with FXI deficiency: a 40-year-old woman with a severe FXI deficiency who died from a stroke due to bilateral internal carotid arteries occlusion after GB for morbid obesity. However, this stroke was probably secondary to a pulmonary embolism with a paradoxical embolism through a previously unknown foramen ovale [14].
FXI deficiency presents distinct difficulties in management. The limited evidence of an association between FXI levels and the bleeding manifestation hinders the ability to predict bleeding results. Individuals with severe deficiency have only a mild bleeding tendency, which is typically provoked by surgery, but the risk of bleeding is not restricted to individuals with severe deficiency, and the bleeding tendency varies among individuals with similar factor XI levels [15]. This makes preoperative assessment of bleeding risk very challenging, especially in patients who have never undergone surgery before.
Preoperative hematological counseling is essential to adequate clotting factor adjustment to avoid bleeding complications and excessive FXI consumption [16].
In fact, the heightened risk of thrombosis and fluid overload in obese patients adds complexity to perioperative hemostatic management. Since FXI concentrates are not readily available, it becomes necessary to resort to FFP infusions, typically at a rate of 10–20 mL/kg, to supplement FXI during the peri-operative period [17]. This, however, raises concerns regarding the increased risk of thrombosis and volume overload, as administering large volumes of FFP is a significant contributor to circulatory overload. In major surgery in these patients, comprehensive FXI replacement and substantial plasma volumes may be required, which in turn pose a notable risk. To mitigate this risk, therapeutic plasma exchange has been used as an alternative approach and should be considered as a potentially safer method for correcting the FXI deficiency [18]. There are no official guidelines regarding the use of postoperative anticoagulants in patients with coagulation disorders. Although FXI deficiency offers some antithrombotic protection, these patients still have indications for anticoagulation therapy due to their obesity, which is a severe risk factor. A retrospective review by Bravo-Perez et al of 15 patients with mild-to-moderate FXI deficiency under anticoagulation therapy recorded 2 mild bleeding episodes in 2 patients, and no major or fatal events [19].
Nevertheless, surgical strategies to decrease the risk of intra-operative and postoperative bleeding are essential. Adequate nutritional management is especially important in the preoperative phase with the intervention of experienced nutrition-ists and dieticians. A modest weight loss of 5–10% with VLCD in the immediate preoperative period has been suggested to facilitate surgery and reduce the risk of complications [20]. Furthermore, VLCKD improves surgical outcomes, influencing drainage output, postoperative hemoglobin levels, and hospital stay [21].
Regarding the choice of the operation, a retrospective study by Zafar et al compared 36 925 patients undergoing GB and 20 020 patients undergoing SG, showing that patients undergoing GB have 38% higher risk of postoperative bleeding than those undergoing SG [22].
Staple line reinforcement (SLR) seems to play a protective role on the incidence of post- operative hemorrhage. Different techniques for SLR have been described: Suture oversewn (SR) includes full-thickness-suturing invagination of the staple line with continuous seromuscular sutures. It seems to be associated with a reduced risk of postoperative bleeding, staple line leaks, and overall complications without significant differences in sleeve stricture, surgical site infections, risk of re-operation, and 30-day mortality [23,24].
Conclusions
Bariatric surgery in patient with FXI deficiency is safe in experienced BS centers, and the risks of obesity seem to over-weight those of the coagulopathy and surgery. Prehabilitation is particularly important in these patients and hematological counseling is essential, since preventive treatments are available. SG seems to be the operation of choice. Suture over-sewn seems a reasonable means to reduce the risk of bleeding from the staple line.
References:
1.. Gentileschi P, Camperchioli I, Benavoli D, Laparoscopic single-port sleeve gastrectomy for morbid obesity: Preliminary series: Surg Obes Relat Dis, 2010; 6(6); 665-69
2.. Buchwald H, Avidor Y, Braunwald E, Bariatric surgery: A systematic review and meta-analysis: JAMA, 2004; 292(14); 1724-37
3.. Janik MR, Walędziak M, Brągoszewski J, Prediction model for hemorrhagic complications after laparoscopic sleeve gastrectomy: Development of SLEEVE BLEED calculator: Obes Surg, 2017; 27(4); 968-72
4.. Daigle CR, Brethauer SA, Tu C, Which postoperative complications matter most after bariatric surgery? Prioritizing quality improvement efforts to improve national outcomes: Surg Obes Relat Dis, 2018; 14(5); 652-57
5.. Mechanick JI, Apovian C, Brethauer S, Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures – 2019 update: Cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists – executive summary: Endocr Pract, 2019; 25(12); 1346-59
6.. Stenberg E, Dos Reis Falcão LF, O’Kane M, Enhanced recovery after surgery (ERAS) society recommendations: A 2021 update: World J Surg, 2022; 46(4); 752
7.. James P, Salomon O, Mikovic D, Peyvandi F, Rare bleeding disorders – bleeding assessment tools, laboratory aspects and phenotype and therapy of FXI deficiency: Haemophilia, 2014; 20(Suppl. 4); 71-75
8.. Wheeler AP, Hemingway C, Gailani D, The clinical management of factor XI deficiency in pregnant women: Expert Rev Hematol, 2020; 13(7); 719-29
9.. Lewandowska MD, Connors JM: Factor XI deficiency, Hematology/Oncology Clinics of North America, 2021; 35; 1157-69
10.. Yerrabothala S, McKernan L, Ornstein DL, Bariatric surgery in haemophilia: Haemophilia, 2016; 22(3); e232-e34
11.. Beomonte Zobel L, Dhimolea S, Billeci F, Same-day discharge bariatric surgery: A pilot experience from an Italian center: Il Giornale di Chirurgia– Journal of the Italian Surgical Association, 2023; 43(4); e33
12.. Plamper A, Goldmann G, Lingohr P, First case of laparoscopic mini-gastric bypass for the treatment of morbid obesity in severe haemophilia A: Hamostaseologie, 2019; 39(2); 208-10
13.. Davulcu EA, Demirci Z, Fırat Ö, Sleeve gastrectomy in a severe hemophilia A patient: One of the very rare cases: Turk J Haematol, 2020; 37(4); 304-6
14.. Rossi P, Sileri P, Gentileschi P, Delayed symptomatic hemobilia after ultrasound-guided liver biopsy: A case report: Hepatogastroenterology, 2002; 49(48); 1659-62
15.. Boehlen F, Casini A, Pugin F, de Moerloose P, Pulmonary embolism and fatal stroke in a patient with severe factor XI deficiency after bariatric surgery: Blood Coagul Fibrinolysis, 2013; 24(3); 347-50
16.. Seligsohn U, Bolton-Maggs P: Factor XI deficiency in: Textbook of Hemophilia, 2010, Hoboken (NJ), Wiley-Blackwell
17.. Shalabi A, Kachel E, Kogan A, Cardiac surgery in patients with hemophilia: Is it safe?: J Cardiothorac Surg, 2020; 15(1); 76
18.. Alsammak MS, Ashrani AA, Winters JL, Pruthi RK, Therapeutic plasma exchange for perioperative management of patients with congenital factor XI deficiency: J Clin Apher, 2017; 32(6); 429-36
19.. Bravo-Pérez C, Serna MJ, Esteban J, Anticoagulant therapy in patients with congenital FXI deficiency: Blood Adv, 2021; 5(20); 4083-86
20.. Van Nieuwenhove Y, Dambrauskas Z, Campillo-Soto A, Preoperative very low-calorie diet and operative outcome after laparoscopic gastric bypass: A randomized multicenter study: Arch Surg, 2011; 146(11); 1300-5
21.. Gils CA, Bonada SA, Montero JM, Effects of two preoperatory weight loss diets on hepatic volume, metabolic parameters, and surgical complications in morbid obese bariatric surgery candidates: A randomized clinical trial: Obes Surg, 2018; 28(12); 3756-68
22.. Zafar SN, Shockcor N, Prasad N, Laparoscopic sleeve gastrectomy has a lower risk of postoperative bleeding than laparoscopic Roux-en-Y gastric bypass: Surg Laparosc Endosc Percutan Tech, 2019; 29(1); 53-57
23.. Aiolfi A, Gagner M, Zappa MA, Staple line reinforcement during laparoscopic sleeve gastrectomy: Systematic review and network meta-analysis of randomized controlled trials: Obes Surg, 2022; 32(5); 1466-78
24.. Özgen G, Çalıkoğlu İ, Acunaş B, Yerdel MA, Staple-line reinforcement using barbed sutures in 1008 sleeve gastrectomies: s.l.: Langenbecks Arch Surg, 2021; 406(5); 1683-90
In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943174
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943136
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943645
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250