15 April 2024: Articles 
Complicated Treatment Course of Severe Asymptomatic Hypertriglyceridemia: A Case Report and Literature Review
Unusual clinical course, Challenging differential diagnosis, Unusual or unexpected effect of treatment, Diagnostic / therapeutic accidents, Adverse events of drug therapy, Educational Purpose (only if useful for a systematic review or synthesis)
Ahmad Wasfi HaddadDOI: 10.12659/AJCR.943858
Am J Case Rep 2024; 25:e943858
Abstract
BACKGROUND: Close observation, statins, fibrate treatment, and lifestyle changes can safely manage asymptomatic individuals with severe hypertriglyceridemia (HTG) and minimal risk of symptom development. However, the risk of medication-induced liver injury in patients taking statin-fibrate makes management more challenging, and may require hospital admission and close monitoring with follow-up.
CASE REPORT: We present a rare case of a 43-year-old man with asymptomatic severe HTG exceeding 11.370 mg/dL with mixed hyperlipidemia, managed initially with high-intensity statins and fibrate. However, due to the concurrent use of statin and fibrates, the patient subsequently developed an acute liver injury. Hence, the oral medications had to be stopped, and the patient was admitted to the hospital for an insulin drip. Even during the hospital course, the patient’s triglyceride (TG) levels showed resistance to the recommended dose of insulin and he required a higher insulin dose. He was discharged on fenofibrate and subcutaneous insulin to keep the TG level under 500. Fibrate was stopped, and high-intensity statin was used as primary prevention with lifestyle modifications.
CONCLUSIONS: This instance highlights the necessity of increased cognizance and cooperative endeavors in handling severe asymptomatic HTG. Our results highlight the significance of further research into the management of severe asymptomatic HTG in cases of injury to the liver. This work adds essential knowledge to the ongoing discussion about managing a rare case complicated by acute liver injury.
Keywords: Chemical and Drug Induced Liver Injury, Cholesterol, LDL, Hypertriglyceridemia
Introduction
In the United States, according to the American Heart Association/American College of Cardiology guidelines, moderate HTG is defined as fasting or non-fasting TG ranging from 175 to 499 mg/dL (2.0 to 5.6 mmol/L). In contrast, severe HTG is fasting TG above 500 mg/dL (≥5.6 mmol/L) [1]. Other lipo-protein abnormalities are often also present. Acute pancreatitis is linked to a significantly raised TG level (>885 mg/dL); this also correlates with having a higher chance of heart problems brought on by atherosclerosis in HTG patients [2,3]. In patients with severe HTG, normalization of TG levels is rarely attained, even with treatment (particularly triglyceride concentrations over 2000 mg/dL [22.60 mmol/L]) [4]. IV insulin infusion is a valuable management tactic since it inhibits lipolysis and lowers the liver’s triglyceride assembly; used with fibrates to reduce TG levels, this combination can reduce TG levels by 30% to 50% while simultaneously raising HDL-C, decreasing VLDL generation, and increasing LPL synthesis [5]. As in our case, asymptomatic HTG with hyperlipidemia can occasionally be managed with statins, fenofibrate, and lifestyle changes, but in cases of medication complications like liver injury, patients may require insulin to lower their TG levels.
Case Report
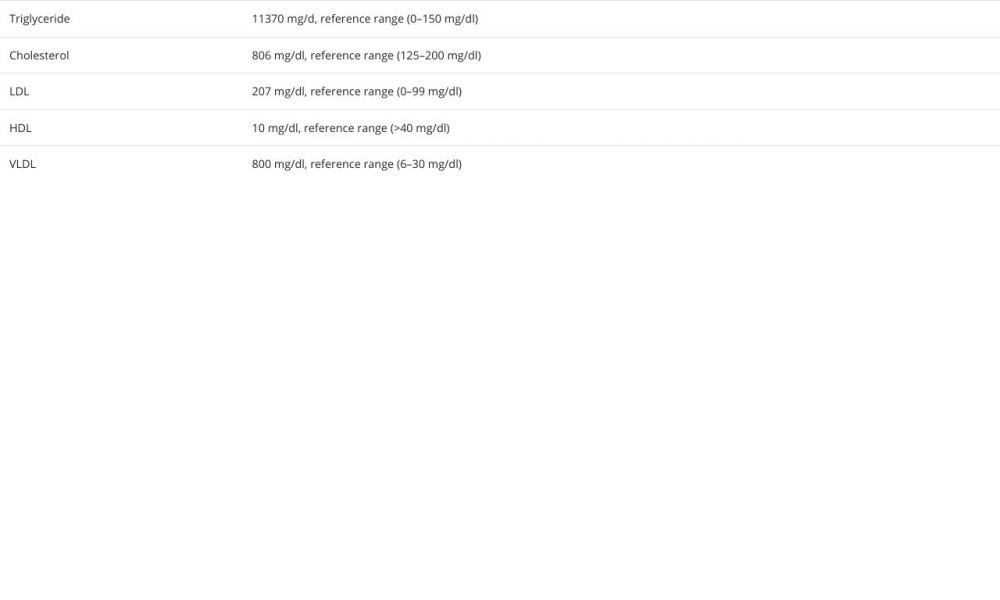
A 43-year-old man with a past medical history of diabetes mellitus type 2 presented to the clinic for a regular check-up. The patient was doing well with no acute concerns, but he needed to be more compliant with the follow-up appointments. The patient denied any chest pain, SOB, abdominal pain, nausea, or vomiting upon reviewing his chart. A lipid profile 8 years ago showed elevated cholesterol at 358 (reference range: 125–200 mg/dl), and his triglyceride level was 1463 mg/dl (reference range: 0–150 mg/dl). At that time, he underwent multiple genetics tests (APOA5, APOC2, APOE, LPL, LMF1, GPIHBP1) with enzyme-linked immunosorbent assay (ELISA), which were all negative, and high-intensity statin was started, but he stopped after 6 months and did not follow up. He had a strong family history of diabetes, but no family history of familial hyper-cholesterolemia or lipid disorder. He had no previous athero-sclerotic events, and denied any smoking or alcohol history. He was not currently on any medications. On physical examination, his vital signs were normal, and there were no signs of distress or pain. There was no tenderness on abdominal examination and no xanthelasmata, xanthomas, or corneal arcus. His weight was 79 kg with a height of 175.3 cm. A lipid panel was done, as shown in Table 1. His hemoglobin A1C was 7.7 with a point-of-care glucose of 232. His ASCVD score was 12.8%.
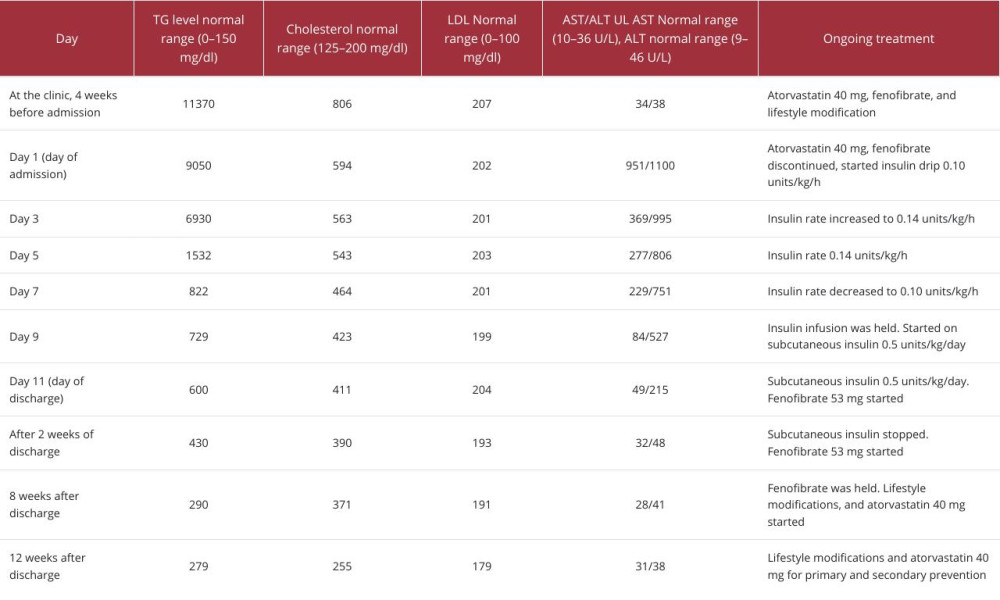
The patient was instructed about lifestyle modifications and was started on a high-intensity statin with fenofibrate and omega 3 for his mixed hyperlipidemia. A follow-up lipid panel 1 month later showed minimal improvement, but there was a significant elevation in his AST/ALT, as shown in Table 2. All the lipid-lowering agents were stopped, and he was admitted to the hospital for insulin infusion. Abdominal US was unre-markable on admission, with normal INR, albumin, and bilirubin levels. The hepatic panel, antinuclear antibodies (ANA), alkaline phosphatase (ALP), creatine phosphokinase (CPK) levels, and anti-smooth muscle antibodies were normal.
He was started on an insulin infusion with a hypoglycemic protocol in place. For the first 3 days, the decrease in TG levels was not as expected, so the insulin dose was increased to 0.14 units/kg/h during hospital days 3–7, then was reduced to 0.1 units/kg/h on day 7, after which his liver enzymes were trending down nicely. The insulin drip was held on day 9 and transitioned to subcutaneous insulin at 0.5 units/kg/day). When the TG levels reached 600 mg/dl on day 11, he was discharged on subcutaneous insulin (0.5/kg/day), and the fenofibrate was started. He was instructed on exercise and referred to the dietician. Two weeks later, his TG fell below 500 mg/dl, so the insulin was discontinued, and an oral hypoglycemic agent was used while keeping the fenofibrate. His liver enzymes returned to normal levels at that time. Eight weeks after discharge, his TG levels decreased to 290 mg/dl, so the fenofibrate was stopped, and high-intensity statin was started for primary and secondary prevention. Twelve weeks after discharge, he was doing well. His lipid profile was more controlled, with TG levels of 279 mg/dl and normal liver enzymes.
Discussion
Hypertriglyceridemia (HTG) is one of the most common lipid abnormalities – 35% of men and 25% of women have TG levels >150 in the United States. There are more than 2.1 million adults in the United States who have severe HTG, which is TG levels >500 [6]. HTG is classified into mild: TG level 150–199 mg/dL, moderate: 200–499 mg/dL, and high or severe: TG >500 mg/dL. HTG is usually asymptomatic until triglycerides are over 1000–2000 mg/dL, and asymptomatic severe hypertriglyceridemia is extremely rare. Symptoms like pain in the mid-epigastric, chest, or back regions, nausea, vomiting, dyspnea, xanthomas, corneal arcus, and xanthelasmas are usually present once TG levels exceed 1000 mg/dl. Serum triglyceride levels above 500 mg/dL (5.6 mmol/L) are associated with a progressive increase in the risk of acute pancreatitis, which increases significantly above 1000 mg/dL (11.3 mmol/L) [7]. Around 5% of cases of acute pancreatitis are associated with serum triglyceride elevations >1000 mg/dL (11.3 mmol/L), and 10–20% are associated with triglyceride elevations >2000 mg/dL (22.6 mmol/L) [8]. Conditions and factors that may cause or exacerbate HTG should be addressed, as it is frequently induced or made worse by potentially treatable causes. For patients with uncontrolled diabetes, improved glycemic control is the first line of treatment [9]. It is best to avoid medications that increase serum TG levels. It is recommended to manage the risk factors for ASCVD, which include addressing a sedentary lifestyle, quitting smoking, and managing hypertension optimally. Regular aerobic exercise is advised, preferably for at least 150 min per week of moderate-intense exercise, 75 min per week of vigorous-intense exercise, or a similar combination. For patients with elevated TG, weight loss of up to 10% of body weight is usually advised [10].
TG levels are usually lowered by 5–15% with statins; however, in individuals with fasting TG levels <400 mg/d, high-intensity statin treatment can reduce TG levels by 25–30% [6]. When treated with a moderate- to high-intensity statin, more notable decreases in TG levels of 40% have been observed in patients with fasting TG levels as high as 800 mg/dL [6]. Ezetimibe lowers TG levels by approximately 7–8%, and pro-protein convertase subtilisin/kexin type 9 (PCSK9) inhibitors lower fasting TG levels by 2–23% [7]. The FDA has authorized fenofibrate for the treatment and management of mixed dyslipidemia, primary hypercholesterolemia, and hypertriglyceridemia; it raises high-density lipoprotein cholesterol in adults while lowering total cholesterol, triglycerides, and low-density lipoprotein. If dietary changes and exercise alone have not reduced cholesterol, fenofibrate should also be administered [11].
There is no doubt that statins, in a few instances, can cause liver injury, which often takes the form of a hepatocellular pattern. In 3% of cases, an extended increase surpassing by 3 times the upper limit of normal for aminotransferase was seen [12]. Discontinuation of the offending statin is essential for preventing the progression of liver injury and monitoring subsequent hepatic injury evolution. Thankfully, severe liver damage associated with statin usage is rare and usually reversible, with no additional treatment needed other than stopping the medication [13]. When statin-induced liver impairment is suspected, it can help to identify the condition early and take the proper steps to prevent severe damage [13].
The use of ezetimibe has increased, especially in the United States. According to specific recommendations, ezetimibe could replace statins as the primary option for those who cannot take them [14]. According to randomized clinical studies, 1% of the treatment group experienced substantial changes in liver function caused by ezetimibe. Ezetimibe, alone or associated with statins, can produce toxic severe hepatitis [15]. Fenofibrate and niacin are also reported to rarely cause acute liver injury [11,16]. Another effective method for decreasing the TG is plasmapheresis, which is indicated when serum triglycerides exceed 1000 mg/dL with high-risk complications [17]. Although plasmapheresis seems like a reasonable option for patients with acute pancreatitis, it is a more costly and invasive procedure, and our patient showed no signs of pancreatitis at all.
When chylomicronemia is unexplained, the GPIHBP1 autoantibody syndrome should be considered. According to recent studies, Rituximab is an effective treatment for the GPIHBP1 autoantibody syndrome. This leads to the elimination of the autoantibodies and a return of plasma triglyceride and LPL levels to normal [18]. Our patient tested negative for GPIHBP1 ELISA autoantibody.
Insulin is a powerful triglyceride-reducing drug that stimulates lipoprotein lipase production, an essential enzyme for TG breakdown [19]. Insulin infusion can be used to immediately reduce the TG level in individuals with severe HTG to less than 1000 mg/dL. In addition to other pharmaceutical treatments, insulin infusion therapy is a less invasive and effective way to quickly treat severe hypertriglyceridemia, particularly in cases with elevated TG levels [20]. Subcutaneous insulin can immediately lower the TG levels and lower the risk of pancreatitis caused by severe hypertriglyceridemia. At the same time, long-term maintenance therapy can be provided by fenofibrates [21]. Various articles in the literature have discussed the appropriate insulin dose for HTG and its effect on TG levels over time – 0.07 units/kg/h, up to 0.1 units/kg/h, are recommended to decrease TG levels lower than 1000 mg/dL in 2 days and lower than 500 mg/dL in approximately 3 days [22]. Our patient needed a higher dose of insulin and a longer time to reach the target, around 500 mg/dl.
Conclusions
Although lifestyle changes are essential in the management of hypertriglyceridemia, medication may also be required in some instances, mainly if HTG is resistant to lifestyle modifications, or if there are concurrent high cholesterol levels or high-risk complications. However, treatment of HTG carries the risk of complications, including drug-induced liver injury. In these cases, management can be complex and challenging. This case report highlights challenges that can face healthcare providers when treating severe asymptomatic HTG. Early recognition and close monitoring are required for successful management.
References:
1.. Sandesara PB, Virani SS, Fazio S, Shapiro MD, The forgotten lipids: Triglycerides, remnant cholesterol, and atherosclerotic cardiovascular disease risk: Endocr Rev, 2019; 40(2); 537-57
2.. Sandhu S, Al-Sarraf A, Taraboanta C, Incidence of pancreatitis, secondary causes, and treatment of patients referred to a specialty lipid clinic with severe hypertriglyceridemia: A retrospective cohort study: Lipids Health Dis, 2011; 10; 157
3.. Shafiq S, Patil M, Gowda V, Devarbhavi H, Hypertriglyceridemia-induced acute pancreatitis – course, outcome, and comparison with non-hypertriglyceridemia associated pancreatitis: Indian J Endocrinol Metab, 2022; 26(5); 459-64
4.. Oh RC, Lanier JB, Management of hypertriglyceridemia: Am Fam Physician, 2007; 75(9); 1365-71
5.. Berglund L, Brunzell JD, Goldberg AC, Endocrine society. Evaluation and treatment of hypertriglyceridemia: An Endocrine Society clinical practice guideline: J Clin Endocrinol Metab, 2012; 97(9); 2969-89 [Erratum in: J Clin Endocrinol Metab. 2015;100(12):4685]
6.. Fan W, Philip S, Granowitz C, Hypertriglyceridemia in statin-treated US adults: The National Health and Nutrition Examination Survey: J Clin Lipidol, 2019; 13(1); 100-8
7.. Lindkvist B, Appelros S, Regnér S, Manjer J, A prospective cohort study on risk of acute pancreatitis related to serum triglycerides, cholesterol and fasting glucose: Pancreatology, 2012; 12(4); 317-24
8.. Miller M, Stone NJ, Ballantyne C, Triglycerides and cardiovascular disease: A scientific statement from the American Heart Association: Circulation, 2011; 123(20); 2292-333
9.. Gotto AM, Hypertriglyceridemia: Risks and perspectives: Am J Cardiol, 1992; 70(19); 19H-25H
10.. Virani SS, Morris PB, Agarwala A, 2021 ACC Expert consensus decision pathway on the management of ASCVD risk reduction in patients with persistent hypertriglyceridemia: A Report of the American College of Cardiology Solution Set Oversight Committee: J Am Coll Cardiol, 2021; 78(9); 960-93
11.. Kayıkçıoğlu M, Shahbazova S, İbrahimov F, Can LH, Cumulative non-HDL-cholesterol burden in patients with hypertriglyceridemia receiving long-term fibrate therapy: Real life data from a lipid clinic cohort: Turk Kardiyol Dern Ars, 2020; 48(4); 359-67
12.. Bhardwaj SS, Chalasani N, Lipid-lowering agents that cause drug-induced hepatotoxicity: Clin Liver Dis, 2007; 11(3); 597-613 , vii
13.. Averbukh LD, Turshudzhyan A, Wu DC, Wu GY, Statin-induced liver injury patterns: A clinical review: J Clin Transl Hepatol, 2022; 10(3); 543-52
14.. Civeira F, Guidelines for the diagnosis and management of heterozygous familial hypercholesterolemia: Atherosclerosis, 2004; 173(1); 55-68
15.. Castellote J, Ariza J, Rota R, Serious drug-induced liver disease secondary to ezetimibe: World J Gastroenterol, 2008; 14(32); 5098-99
16.. Etchason JA, Miller TD, Squires RW, Niacin-induced hepatitis: A potential side effect with low-dose time-release niacin: Mayo Clin Proc, 1991; 66(1); 23-28
17.. Joglekar K, Brannick B, Kadaria D, Sodhi A, Therapeutic plasmapheresis for hypertriglyceridemia-associated acute pancreatitis: Case series and review of the literature: Ther Adv Endocrinol Metab, 2017; 8(4); 59-65
18.. Miyashita K, Lutz J, Hudgins LC, Chylomicronemia from GPIHBP1 autoantibodies: J Lipid Res, 2020; 61(11); 1365-76
19.. Sadur CN, Eckel RH, Insulin stimulation of adipose tissue lipoprotein lipase. Use of the euglycemic clamp technique: J Clin Invest, 1982; 69(5); 1119-25
20.. Poonuru S, Pathak SR, Vats HS, Pathak RD, Rapid reduction of severely elevated serum triglycerides with insulin infusion, gemfibrozil and niacin: Clin Med Res, 2011; 9(1); 38-41
21.. Jabbar MA, Zuhri-Yafi MI, Larrea J, Insulin therapy for a non-diabetic patient with severe hypertriglyceridemia: J Am Coll Nutr, 1998; 17(5); 458-61
22.. Hoff A, Piechowski K, Treatment of hypertriglyceridemia with aggressive continuous intravenous insulin: J Pharm Pharm Sci, 2021; 24; 336-42
In Press
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250