22 June 2020: Articles 
Acute Opioid Withdrawal Mimicking Postoperative Joint Infection Following Anterior Cruciate Ligament (ACL) Reconstruction: A Case Report
Unusual clinical course, Challenging differential diagnosis, Unusual or unexpected effect of treatment, Unexpected drug reaction
Qingwu Kong12EFG*, Martin Griffis23EG, Brandon J. Shallop2ABCDEF, Amrit S. Khalsa23ABCDEF, Kyle Brougham2CDEF, Paul A. Marchetto4ABCDEFDOI: 10.12659/AJCR.923458
Am J Case Rep 2020; 21:e923458
Abstract
BACKGROUND: A short course of opioid narcotics is often prescribed for postoperative anterior cruciate ligament (ACL) reconstruction pain management. Unfortunately, there is a well-documented incidence of opioid withdrawal syndrome (OWS) following short-term use of these medications. OWS can present with symptoms such as influenza-like illness. It is important to differentiate OWS from infectious illnesses, especially after surgery.
CASE REPORT: We present a case of OWS in a patient who underwent ACL reconstruction 7 days prior. The patient’s OWS symptoms were similar to symptoms of a postoperative infection. The knee was aspirated, and the analysis of the aspirate was not concerning for an infection. The patient’s symptoms spontaneously resolved on postoperative day 10. This is the first documented case of OWS mimicking ACL reconstruction joint infection.
CONCLUSIONS: OWS after surgery may present with symptoms similar to joint infection. It is important to consider OWS as a potential complication after surgery and differentiate it from infection to avoid any further unnecessary invasive treatments for the patient.
Keywords: Analgesics, Opioid, anterior cruciate ligament reconstruction, Arthritis, Infectious, Anterior Cruciate Ligament, Diagnosis, Differential, Joint Diseases, Substance Withdrawal Syndrome, Surgical Wound Infection, young adult
Background
Opioid withdrawal syndrome (OWS) has been well-characterized in the literature. Although it can present in a variety of ways, it has been described as a moderate to severe influenza-like illness [1,2]. It has been well-described that opioid dependence can begin to develop after a single dose of narcotic medications [3,4]. It has also been shown that patients who use narcotics for the short-term management of pain (1 to 2 weeks) commonly complain of signs and symptoms of opioid withdrawal upon cessation of these agents [5,6]. The development of OWS postoperatively can complicate recovery from even minor procedures and provide a diagnostic challenge, as the signs and symptoms can be nonspecific and mimic other postoperative complications, including infection [7].
Over 130 000 anterior cruciate ligament (ACL) reconstructions are performed every year in the United States, and this number has increased over the past decade [8–12]. With the use of arthroscopic surgical techniques, this procedure is commonly performed as an outpatient surgery [13]. Narcotics are also commonly prescribed for pain control upon discharge following inpatient procedures [14].
There are no currently published guidelines for postoperative pain management following arthroscopy-assisted ACL reconstruction; however, most regimens that have been shown to be successful combine a number of different modalities to provide perioperative and postoperative pain relief [15]. These modalities include systemic and/or intra-articular opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), local anesthetics, local anesthetic pumps, regional nerve blocks, and forms of cryotherapy.
While there is a great deal of variability in the modalities employed for perioperative pain management, most physicians opt for a short course of opioid narcotics to be taken as needed for pain with or without an NSAID after discharge [16]. Commonly used opioids include hydrocodone/acetaminophen (5/325 mg) and oxycodone/acetaminophen (5/325 mg) [17,18] Generally, these agents are prescribed to be taken every 4 to 6 hours as needed for pain, with most physicians prescribing enough tablets to be taken 2 to 3 times per day for about 2 weeks. It is therefore important for all orthopedic surgeons to monitor for the development of OWS in patients using these agents for postoperative pain control and to consider this condition in the differential diagnosis of postoperative complications.
While the majority of patients will not develop opioid dependence from this short course of narcotics, regimens that are similar to those that are commonly used following ACL reconstruction have been shown to induce opioid dependence and withdrawal upon cessation of the drugs [5,7].
Here we present the case of a patient who experienced acute OWS after the short-term use of narcotics as prescribed for pain relief following ACL reconstruction. The patient had verbally consented to be the subject of this case report. The patient’s presentation was concerning for a postoperative joint infection. Postoperative joint infection is a serious and morbid diagnosis that occurs in 0.5% of all ACL reconstructions [19]. This postoperative complication requires emergent surgical irrigation and debridement, and may require ACL graft removal [20–24]. This patient’s unusual presentation led to a diagnostic dilemma that nearly resulted in further unnecessary surgical intervention and potential postoperative morbidity.
Despite the frequent use of narcotics for postoperative pain management and the well-documented incidence of OWS following the short-term use of narcotic pain medications, there are no published case reports of OWS in the postoperative period following arthroscopic ambulatory procedures, such as ACL reconstruction, and this condition is rarely discussed in the orthopedic literature. The purpose of this article is to present a case which illustrates the importance of considering OWS as a potential complication in the acute postoperative period from ACL reconstruction.
Case Report
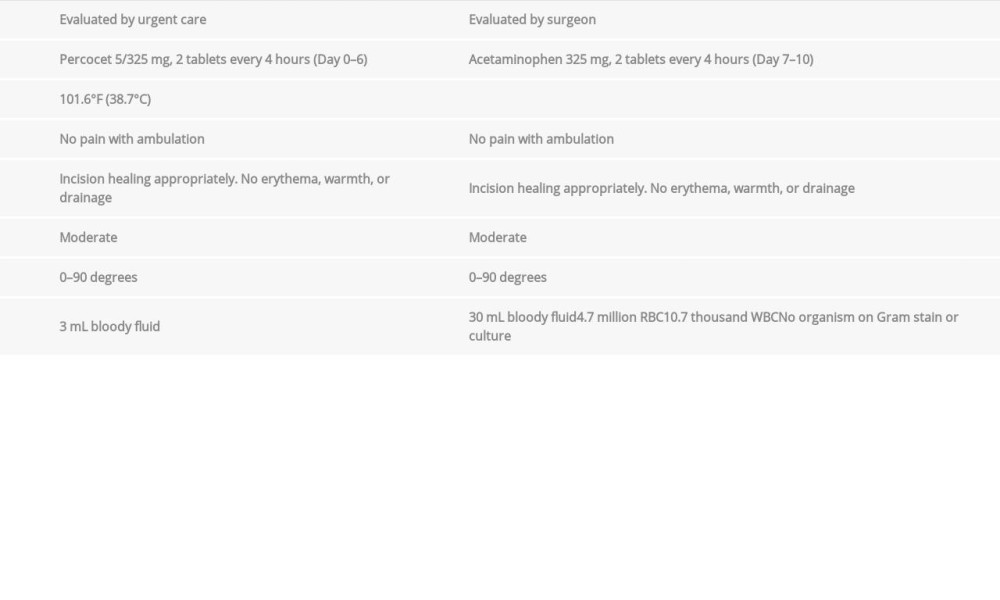
A 19-year-old male presented to a local urgent care center 7 days status post unilateral, primary, arthroscopic right knee ACL reconstruction with hamstring (gracilis and semitendinosus tendon) autograft as well as partial lateral meniscectomy. He had no past medical history. He also did not have a history of cigarette, alcohol, and illicit substance use. His otherwise routine postoperative course was complicated with 24 hours of acute onset of a low-grade fevers, chills, malaise, and nausea. He also noted having residual pain about his right knee that worsened over that period. A review of systems noted an increased frequency of bowel movements but was otherwise negative. He had been taking a total regimen of 2 Percocet 5/325 mg tablets every 4 hours from postoperative day 0 through 6 for postoperative pain until running out of medication the day prior to presentation to the urgent care center. He had not taken additional Percocet since this day. Instead, he took 2 acetaminophen 325 mg tablets every 4 hours starting on postoperative day 7. He did not take any other medications during this postoperative course.
He was evaluated by the urgent care physician and was found to be febrile to 101.6°F (38.7°C) with all other vital signs within normal limits. On examination of his right lower extremity, the patient had a moderate effusion and was able to range his right knee from 0° to 90° of flexion. He was able to weight bear without pain. Incisions were documented to be healing appropriately without erythema, warmth, or drainage.
The urgent care physician attempted to aspirate the right knee for pain control as well as to send for culture; 2 mL of bloody fluid were aspirated from the joint. After discussion with the operative surgeon, the patient was placed on a course of an oral cephalosporin and instructed to follow up with his treating surgeon as soon as possible.
Two days later, on postoperative day 9, the operative surgeon saw the patient in the office setting. Two days into his course of oral antibiotics, the patient again expressed concerns of having subjective fevers, although he reported his measured temperature at home never exceeded 99°F (37.2°C). He also continues to note vague gastrointestinal (GI) upset and flu-like symptoms.
The patient’s knee continued to have a moderate effusion; however, again there were no signs of surgical site infection. His knee range of motion continued to be 0° to 90° of flexion without significant pain. He was able to weight bear without pain.
Based on history and physical, an acute postoperative infection could not be ruled-out. It was also discussed that the patient may be having adverse effects from being on high doses of narcotics. It was thus decided to aspirate the right knee joint and send the specimen for cell count, culture, and Gram stain. A right knee aspirate was performed under sterile conditions, and 30 mL of bloody fluid was retrieved. The concerns of a possible joint infection were expressed to the patient, and it was decided that the patient would be sent home and monitored closely for the next 24 hours while the aspirate results were pending. Based on the results of the joint aspirate and the patient’s symptoms over the next 24 hours, the decision to undergo an arthroscopic right knee irrigation and debridement would be made.
The patient’s symptoms of fevers, chills, and GI upset spontaneously resolved on postoperative day 10. The aspirate results came back showing 4.7 million red blood cells, 10.7 thousand white blood cells, and no organisms seen on Gram stain. The final culture of the aspirate showed no growth at 14 days. The remainder of the patient’s postoperative course was unre-markable. A summary of the patient’s examination and findings are exhibited in Table 1.
Discussion
Opioid withdrawal syndrome is a well-documented complication following narcotic use for the management of acute postoperative pain, though not well-described in the orthopedic literature. The symptoms are generally nonspecific and often resemble an influenza-like illness [1]. Furthermore, young patients who use narcotics for the short-term management of pain (1 to 2 weeks) will commonly complain of severe signs and symptoms of opioid withdrawal upon cessation of these agents [5,6]. This scenario following minor ambulatory procedures and poses a challenging diagnostic dilemma for many surgeons, as symptoms of OWS can often mimic infection [7]. Furthermore, postoperative infection following ACL reconstruction most frequently occurs within the first 2 weeks following surgery, which is similar to the timeframe for the development of OWS in patients using narcotics for 1 to 2 weeks postoperatively, making it all the more important to differentiate between these 2 conditions [25,26].
In our case, the patient presented with symptoms mimicking a postoperative infection on postoperative day 7. He stopped taking narcotic medication 1 day before presentation of symptoms. Infection was ruled out by arthrocentesis fluid analysis. He was diagnosed with OWS after his symptoms spontaneously resolved on postoperative day 10 and thus avoided unnecessary surgical debridement for septic arthritis.
Septic arthritis following ACL reconstruction is a potentially devastating complication; understanding that OWS can mimic the symptoms is invaluable as it may limit further morbidity or undue testing for a patient, such as arthrocentesis or even joint lavage. When the diagnosis of septic arthritis following ACL reconstruction is suspected, immediate initiation of treatment including arthrocentesis, the administration of broad-spectrum antibiotics, and immediate arthroscopic irrigation and debridement is required to prevent rapid joint destruction [20,27]. During the initial irrigation and debridement procedure, extensive lavage and complete synovectomy of all compartments is strongly recommended, which sometimes requires conversion to open arthrotomy and debridement [21]. Some authors recommend an additional debridement procedure even in the absence of unresolving laboratory markers or a failure to improve clinically [23]. In addition, the decision to retain or remove the graft is made during the initial procedure. If the decision is made to remove the graft, all hardware must be removed, and the tibial and femoral tunnels require extensive exploration and debridement [22]. While it is unlikely that a graft would require removal in the absence of a true infection, the initial extensive irrigation and debridement procedure can result in significant unnecessary morbidity in a patient with incorrectly diagnosed septic arthritis following ACL reconstruction.
With many of the patients undergoing ACL reconstruction being from a younger demographic (most commonly between the ages of 10 to 29 years) and opioid-naive, it is possible that acute OWS may be an unforeseen and under-reported complication following this procedure as compared to other ambulatory procedures [28]. It is reasonable to assume that OWS is, in fact, more common than an acute postoperative joint infection following arthroscopy-assisted ACL reconstruction, as the reported incidence of septic arthritis following this procedure is only 0.5% [19].
There is a wealth of literature documenting different modalities used for the treatment of postoperative pain following arthroscopy-assisted ACL reconstruction, but currently there are no accepted or published guidelines for postoperative pain management [15]. Although there is wide variation in the modalities employed for perioperative pain management, most physicians opt for a short course of opioids upon discharge [16]. Despite this, OWS is rarely discussed as a potential complication in the postoperative period following ambulatory arthroscopic procedures. Furthermore, to our knowledge, this is the first published case report of a patient who developed OWS following arthroscopic ACL reconstruction. In addition, there are no other published reports of OWS being potentially mistaken for a postoperative infection; however, this is an important consideration for all surgeons prescribing opioids for pain control in the postoperative period.
The limitation of this case report is the lack of precise data on the patient’s pain level and when he took his pain medication from postoperative day 0 to 6. Although he stated he took 2 tablets of Percocet 5/325 mg every 4 hours, it was unclear for which pain level he took the medication or if he tried to ween down his narcotic use prior to presentation. However, the patient presenting with flu-like symptoms at 1 day after running out of narcotic medication was a big clue to suspect OWS.
Conclusions
Due to the possibility of subjecting a patient to additional, unnecessary testing and procedures, and the associated increased morbidity, it is important for physicians to consider and rule out other conditions that can mimic septic arthritis, such as OWS, in patients who have undergone ACL reconstruction. To our knowledge, this is the first published case report of a patient developing OWS mimicking postoperative infection after ACL reconstruction. This case report provides high educational value for all surgeons who employ the use of narcotics following a surgical procedure and highlights the importance of recognizing symptoms of OWS and differentiating it from postoperative infection.
References:
1.. Farrell M, Opiate withdrawal: Addiction, 1994; 89(11); 1471-75
2.. Wesson DR, Ling W, The Clinical Opiate Withdrawal Scale (COWS): J Psychoactive Drugs, 2003; 35(2); 253-59
3.. Bickel WK, Stitzer ML, Liebson IA, Bigelow GE, Acute physical dependence in man: Effects of naloxone after brief morphine exposure: J Pharmacol Exp Ther, 1988; 244(1); 126-32
4.. Azolosa JL, Stitzer ML, Greenwald MK, Opioid physical dependence development: Effects of single versus repeated morphine pretreatments and of subjects’ opioid exposure history: Psychopharmacology (Berl), 1994; 114(1); 71-80
5.. Miser AW, Chayt KJ, Sandlund JT, Narcotic withdrawal syndrome in young adults after the therapeutic use of opiates: Am J Dis Child, 1986; 140(6); 603-4
6.. Wakim JH, Alleviating symptoms of withdrawal from an opioid: Pain Ther, 2012; 1(1); 4
7.. Higa KD, Ho T, Boone KB, Roubicek MC, Narcotic withdrawal syndrome following gastric bypass – a difficult diagnosis: Obes Surg, 2001; 11(5); 631-34
8.. Buller LT, Best MJ, Baraga MG, Kaplan LD, Trends in anterior cruciate ligament reconstruction in the united states: Orthop J Sports Med, 2015; 3(1); 2325967114563664
9.. Barrington JW, Fast-track recovery and outpatient joint arthroplasty: Am J Orthop (Belle Mead NJ), 2015; 44(10 Suppl.); S21-22
10.. Best MJ, Buller LT, Eismont FJ, National trends in ambulatory surgery for intervertebral disc disorders and spinal stenosis: A 12-year analysis of the national surveys of ambulatory surgery: Spine (Phila Pa 1976), 2015; 40(21); 1703-11
11.. Best MJ, Buller LT, Miranda A, National trends in foot and ankle arthrodesis: 17-year analysis of the national survey of ambulatory surgery and national hospital discharge survey: J Foot Ankle Surg, 2015; 54(6); 1037-41
12.. Patel AA, Buller LT, Fleming ME, National trends in ambulatory surgery for upper extremity fractures: A 10-year analysis of the US National Survey of Ambulatory Surgery: Hand (NY), 2015; 10(2); 254-59
13.. Kim S, Bosque J, Meehan JP, Increase in outpatient knee arthroscopy in the United States: A comparison of National Surveys of Ambulatory Surgery, 1996 and 2006: J Bone Joint Surg Am, 2011; 93(11); 994-1000
14.. Roberts M, Brodribb W, Mitchell G, Reducing the pain: A systematic review of postdischarge analgesia following elective orthopedic surgery: Pain Med, 2012; 13(5); 711-27
15.. Reuben SS, Sklar J, Pain management in patients who undergo outpatient arthroscopic surgery of the knee: J Bone Joint Surg Am, 2000; 82-A(12); 1754-66
16.. Noonan B, Chung KS, A practical review of the mechanisms of pain and pain management following ACL reconstruction: Orthopedics, 2006; 29(11); 999-1005
17.. Beck PR, Nho SJ, Balin J, Postoperative pain management after anterior cruciate ligament reconstruction: J Knee Surg, 2004; 17(1); 18-23
18.. Macdonald SA, Heard SM, Hiemstra LA, A comparison of pain scores and medication use in patients undergoing single-bundle or double-bundle anterior cruciate ligament reconstruction: Can J Surg, 2014; 57(3); E98-104
19.. Kim SJ, Postigo R, Koo S, Kim JH, Infection after arthroscopic anterior cruciate ligament reconstruction: Orthopedics, 2014; 37(7); 477-84
20.. Matava MJ, Evans TA, Wright RW, Shively RA, Septic arthritis of the knee following anterior cruciate ligament reconstruction: Results of a survey of sports medicine fellowship directors: Arthroscopy, 1998; 14(7); 717-25
21.. Indelli PF, Dillingham M, Fanton G, Schurman DJ, Septic arthritis in postoperative anterior cruciate ligament reconstruction: Clin Orthop Relat Res, 2002(398); 182-88
22.. Schulz AP, Götze S, Schmidt HG, Septic arthritis of the knee after anterior cruciate ligament surgery: a stage-adapted treatment regimen: Am J Sports Med, 2007; 35(7); 1064-69
23.. Cadet ER, Makhni EC, Mehran N, Schulz BM, Management of septic arthritis following anterior cruciate ligament reconstruction: A review of current practices and recommendations: J Am Acad Orthop Surg, 2013; 21(11); 647-56
24.. Waterman BR, Arroyo W, Cotter EJ, Septic arthritis after anterior cruciate ligament reconstruction: Clinical and functional outcomes based on graft retention or removal: Orthop J Sports Med, 2018; 6(3); 2325967118758626
25.. Monaco E, Maestri B, Labianca L, Clinical and radiological outcomes of postoperative septic arthritis after anterior cruciate ligament reconstruction: J Orthop Sci, 2010; 15(2); 198-203
26.. Stucken C, Garras DN, Shaner JL, Cohen SB, Infections in anterior cruciate ligament reconstruction: Sports Health, 2013; 5(6); 553-57
27.. Sajovic M, Nič Ar GL, Dernovš Ek MZ, Septic arthritis of the knee following anterior cruciate ligament reconstruction: Orthop Rev (Pavia), 2009; 1(1); e3
28.. Leathers MP, Merz A, Wong J, Trends and demographics in anterior cruciate ligament reconstruction in the United States: J Knee Surg, 2015; 28(5); 390-94
In Press
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250