29 June 2020: Articles 
Associated Peritonitis with CAPD Successfully Treated Using a Linezolid and Tedizolid Containing Regimen Suggested Immunomodulatory Effects
Challenging differential diagnosis, Unusual or unexpected effect of treatment, Patient complains / malpractice, Rare disease
Masafumi SekiACDEFG, Yasuhiro KamiokaBC, Kazuki TakanoBCD, Haruka ImaiBC, Mai ShojiBC, Maya HariuBCD, Yukari KabutoyaB, Yuji WatanabeABCDDOI: 10.12659/AJCR.924642
Am J Case Rep 2020; 21:e924642
Abstract
BACKGROUND: Mycobacterium abscessus is one of the most important mycobacteria, but its associated peritonitis in patients on continuous ambulatory peritoneal dialysis (CAPD) appears relative rare, and the treatment regimen of the antibiotics are still unclear.
CASE REPORT: A 38-year-old female with chronic glomerulonephritis on CAPD who was diagnosed with M. abscessus-associated peritonitis. Symptoms exacerbated despite treatment with a 3-antibiotic regimen combining clarithromycin, imipenem/cilastatin (IPM/CS), and minocycline (MINO). However, after changing IPM/CS and MINO to linezolid (LZD), her condition and inflammation improved, and she was able to be maintained on oral tedizolid (TZD).
CONCLUSIONS: Oxazolidinones such as LZD and TZD might be candidate antibiotics for the treatment of M. abscessus-associated diseases with chronic renal failure due to their immunomodulatory effects and non-renal excretion.
Keywords: Antibiotics, Antitubercular, Immunocompromised Host, Mycobacterium Infections, Nontuberculous, Renal Insufficiency, Chronic, Anti-Bacterial Agents, Chronic Disease, Glomerulonephritis, linezolid, Mycobacterium abscessus, Oxazolidinones, Peritoneal Dialysis, Continuous Ambulatory, peritonitis, Tetrazoles
Background
Non-tuberculous mycobacteria (NTM)-associated peritonitis during continuous ambulatory peritoneal dialysis (CAPD) is considered relative rare although peritonitis is one of the most serious complications associated with peritoneal dialysis [1].
Peritonitis is a frequent complication of CAPD and most of the episodes of peritonitis are caused by touch contamination of the dialysis tubing or by extension of the catheter exit site or tunnel infection [2]. Coagulase-negative and coagulase-positive staphylococci are the 2 most common organisms, accounting for 50% or more of all CAPD peritonitis, and other Gram-positive and Gram-negative bacteria and fungi account for the rest. Intraperitoneal antibiotic treatments are usually effective in eradicating the infection, and the choice of antibiotics depends on organisms isolated from cultured dialysate.
Furthermore, Tian et al. reported that they had 31 patients die among 2917 CAPD patients during the study period from 2002 to 2014 and that the most common causes of CAPD-related death were cerebrovascular disease (29.0%) and infection (19.4%) [3]. They also found similar common pathogens, such as Gram-positive bacteria followed by Gram-negative bacteria in CAPD peritonitis
Here, we report a case of definite
Case Report
A 38-year-old female developed renal failure and glomerulonephritis and mainly received immunosuppressive agents such as prednisolone, tacrolimus, and cyclophosphamide. However, extensive chronic renal failure subsequently developed.
During the 2 years following onset of chronic kidney disease, she experienced repeated infectious diseases, including cytomegalovirus and aspergillosis. Kidney function was gradually worsened due to long-term administration of nephrotoxic agents, including tacrolimus (controlled concentration range: 5–10 ng/mL), voriconazole, and valganciclovir. CAPD was started after 2 years of follow-up on an outpatient basis.
The patient experienced bacterial peritonitis several times mainly due to
She was admitted to our hospital because of turbidity in the peritoneal drainage fluid with fever and abdominal pain after 18 months on CAPD administration although levofloxacin was received orally in the outpatient clinic for 1 week. Physical examination showed slight tenderness around the umbilicus in abdomen. Her blood pressure was 120/70 mmHg, temperature of 37.2°C, respiratory rate of 18 breaths per minute, and consciousness level of E4V5M6 on the Glasgow coma scale (GCS). Laboratory data were as follows: white blood cell (WBC) count, 6.1×103/µL with 76.5% neutrophils, 11.3% lymphocytes, 9.3% monocytes, 0.6% basophils, and 2.3% eosinophils; platelet count, 224×103/µL; hemoglobin, 7.6 g/dL; serum creatinine, 7.85 mg/dL; blood urea nitrogen, 51 g/L; uric acid, 5.1 mg/dL; and C-reactive protein, 2.16 mg/dL. Peritoneal fluid contained WBCs (2234/µL; 4% mononuclear cells, 96% polymorphonuclear cells). We found slight pus and erythema at the peritoneal dialysis catheter exit site and the ascites and thickening of the peritoneum with edema were shown in the computed tomography of the abdomen (Figure 1).
We did not find the other pathological changes, including the intra-abdominal abscess and the perforation of intestines, therefore, CAPD-associated peritonitis was diagnosed and peritoneal fluid from the peritoneal tube and blood were collected as culture specimens. Treated with 1 g of intravenous meropenem on alternate days in combination with intraperitoneal administration of cefazolin 1 g/day and ceftazidime 1 g/day were started empirically. Although these antibiotic were continued for a week, WBC in the peritoneal fluid were increased to 2796/µL and the condition of the patient deteriorated with vomiting and abdominal pain, and high fever of 38.3°C was found, although her blood pressure of 116/60 mmHg, respiratory rate of 19 breaths per minute, and consciousness level was E4V5M6 of GCS had not worsen. Peritoneal fluid showed WBC counts in her peritoneal fluid and serum C-reactive protein were increased to 3463/µL and 3.72 mg/dL, respectively.
Bacterial cultures, including blood and sputum, which are collected on admission routinely to rule out the bacteremia and pneumonia due to resistant pathogens, yielded negative results on day 3 post-admission, but acid-fast bacilli were identified from smears of peritoneal fluid (Figure 2).
Because a severe condition of the patient was suspected, the peritoneal dialysis catheter was removed, and she was started on hemodialysis. In addition, the combination antibiotic therapy comprising oral CAM at 800 mg, intravenous imipenem/cilastatin (IPM/CS) 1 g, and minocycline (MINO) 200 mg was started and continued for more 1 week. However, her condition and laboratory data worsened, and intra-abdominal fluid cell numbers were still high at 3014/µL. We then changed 2 of the 3 antibiotics, removing IPM/CS and MINO, and adding intravenous LZD at 1.2 g/day because the agent was known as immunomodulation, and non-dose adjustment necessary even in patients with renal failure.
Her condition subsequently improved, and WBC in the perito-neal fluid decreased to 1876/µL and C-reactive protein in the serum returned to 1.26 mg/dL. More than 2 weeks later, we found decreased of platelet counts in the blood from 2.2×105/µL to 1.0×105/µL, which is a well- known side effect of LZD, therefore, we changed intravenous LZD to oral TZD, an oxazolidinone similar to LZD but not associated with thrombocytopenia, and found that her condition remained stable and her WBC in the peritoneal fluid and C-reactive protein in the serum decreased to 1072/µL and 0.17 mg/dL, respectively, although the drug sensitivity of
Discussion
We previously reported
Abdominal
Moxifloxacin, azithromycin, and cefoxitin might be good alterative candidates, however, we had already use levofloxacin, which was similar to moxifloxacin, and found less improvement. In addition, azithromycin is a macrolide, as is CAM which was already used, and cefoxitin is a beta-lactams as is IPM/CS which was already used, too. Therefore, we selected LZD, which was very different from the other agents we had already used that had poor effects clinically, although LZD showed less susceptibility
LZD has been used as an emerging treatment option for systemic NTM infections. Susceptibility of
LZD, one of the oxazolidinone antibiotics, is known as an immunomodulatory drug, and inhibitory effects on cytokines and inflammation have been reported [13]. Decreased levels of chemokines KC and MIP-2, and proinflammatory cytokine IFN-γ, TNFα, and IL-1β were found in the lungs of influenza-related community-acquired MRSA pneumonia mice models after treatment with LZD as compared to vancomycin [8].
These effects might have been sufficient in the present case, in addition to macrolides antibiotics such as CAM and azithromycin which are also known to exert immunomodulatory effects [14,15]. Furthermore, LZD is known to show very good penetration into most tissues in humans, and a full dose can be used even in patients with renal failure, including patients on CAPD as in the present case [16,17].
In addition, TZD has become available as an oxazolidinone with immunomodulatory effects similar to LZD but offering greater effectiveness at only half the dose of LZD [18,19]. We might be able to treat
Conclusions
We report a
References:
1.. Chen J, Zhao L, Mao Y: Front Microbiol, 2019; 10; 1977
2.. Saktayen MG, CAPD peritonitis. Incidence, pathogens, diagnosis, and management: Med Clin North Am, 1990; 74; 997-1010
3.. Tian Y, Xie X, Xiang S, Risk factors and outcomes of high peritonitis rate in continuous ambulatory peritoneal dialysis patients: A retrospective study: Medicine (Baltimore), 2016(2); e5569 95
4.. Bostan C, Slim E, Choremis J: J Cataract Refract Surg, 2019; 45; 1032-35
5.. Shen Y, Wang X, Jin J: Biomed Res Int, 2018; 2018; 4902921
6.. Miyashita E, Yoshida H, Mori D: Pediatr Int, 2014; 56; e96-98
7.. Song Y, Wu J, Yan H, Chen J, Peritoneal dialysis-associated nontuberculous mycobacterium peritonitis: A systematic review of reported cases: Nephrol Dial Transplant, 2012; 27; 1639-44
8.. Ding LW, Lai C, Lee LN, Hsueh PR, Abdominal nontuberculous mycobacterial infection in a university hospital in Taiwan from 1997 to 2003: J Formos Med Assoc, 2006; 105; 370-76
9.. Kleinpeter MA, Krane N, Treatment of mycobacterial exit-site infections in patients on continuous ambulatory peritoneal dialysis: Adv Perit Dial, 2001; 17; 172-75
10.. Yoshimura R, Kawanishi M, Fujii S: BMC Nephrol, 2018; 19(1); 341
11.. Ruth MM, Sangen J, Pennings LJ: Antimicrob Agents Chemother, 2018; 62; e01208-18 pii:
12.. Kim SY, Jhun B, Moon SM: Diagn Microbiol Infect Dis, 2019; 94; 38-40
13.. Bhan U, Podstad A, Kovach MA, Linezolid has unique immunomodulatory effects in post-influenza community acquired MRSA pneumonia: PLoS One, 2015; 10(1); e114574
14.. Seki M, Sakata T, Toyokawa M: Intern Med, 2016; 55; 307-10
15.. Kakeya H, Seki M, Izumikawa K, Efficacy of combination therapy with oseltamivir phosphate and azithromycin for influenza: A multicenter, open-label, randomized study: PLoS One, 2014; 14; e91293
16.. Bogard KN, Peterson N, Plumb TJ, Antibiotic dosing during sustained low-efficiency dialysis: Special considerations in adult critically ill patients: Crit Care Med, 2011; 2(39); 56-70
17.. El-Naggari M, El Nour I, Al-Nabhani D: J Infect Public Health, 2016; 9(2); 192-97
18.. Housman ST, Pope J, Russomanno J, Pulmonary disposition of tedizolid following administration of once-daily oral 200-milligram tedizolid phosphate in healthy adult volunteers: Antimicrob Agents Chemother, 2012; 56; 2627-34
19.. Lemaire S, Van Bambeke F, Appelbaum PC, Tulkens PM, Cellular pharmacokinetics and intracellular activity of torezolid (TR-700): studies with human macrophage (THP-1) and endothelial (HUVEC) cell lines: J Antimicrob Chemother, 2009; 64; 1035-43
20.. Tang YW, Cheng B, Yeoh SF: Front Microbiol, 2018; 9; e20950
Figures
Tables
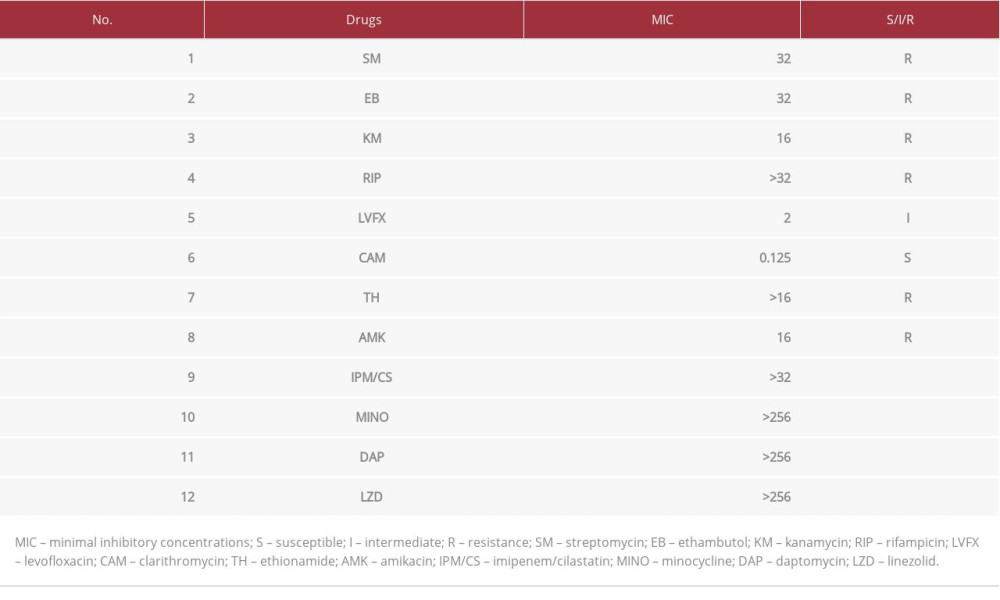 Table 1.. Drug susceptibilities of Mycobacterium abscessus isolated from peritoneal fluid.
Table 1.. Drug susceptibilities of Mycobacterium abscessus isolated from peritoneal fluid.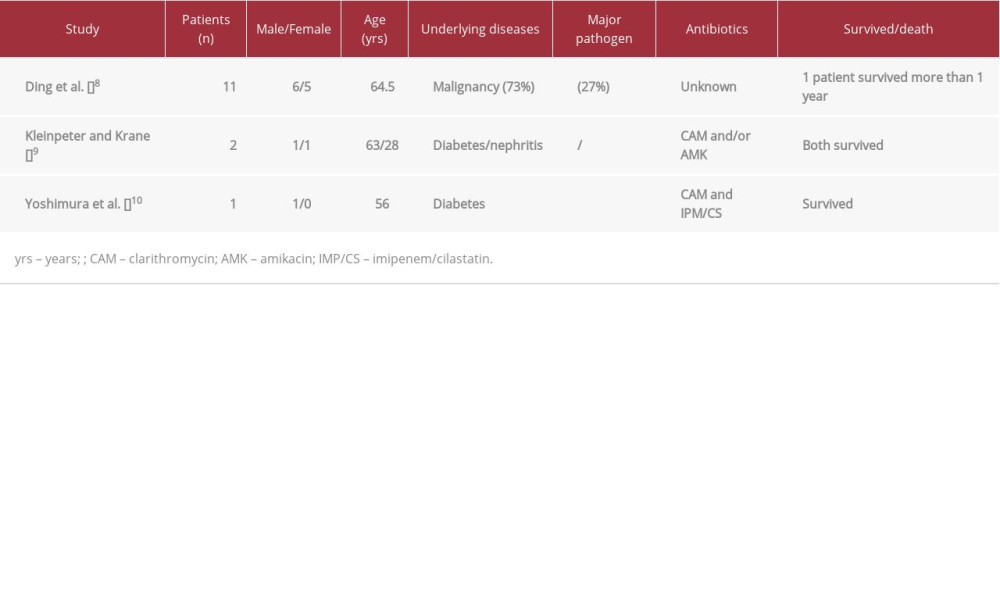 Table 2.. Reported peritonitis cases where Mycobacterium abscessus was isolated.
Table 2.. Reported peritonitis cases where Mycobacterium abscessus was isolated.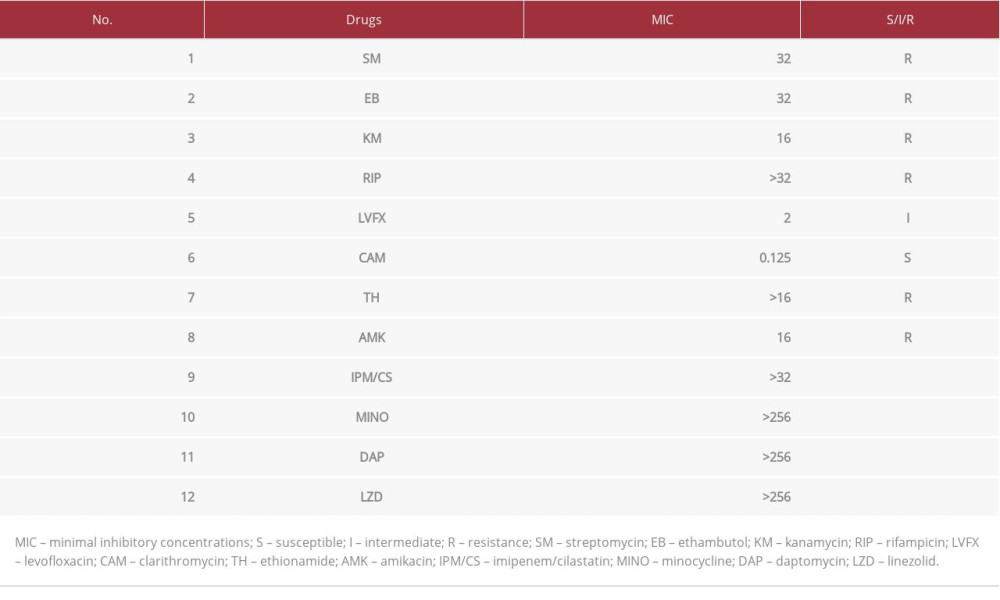 Table 1.. Drug susceptibilities of Mycobacterium abscessus isolated from peritoneal fluid.
Table 1.. Drug susceptibilities of Mycobacterium abscessus isolated from peritoneal fluid.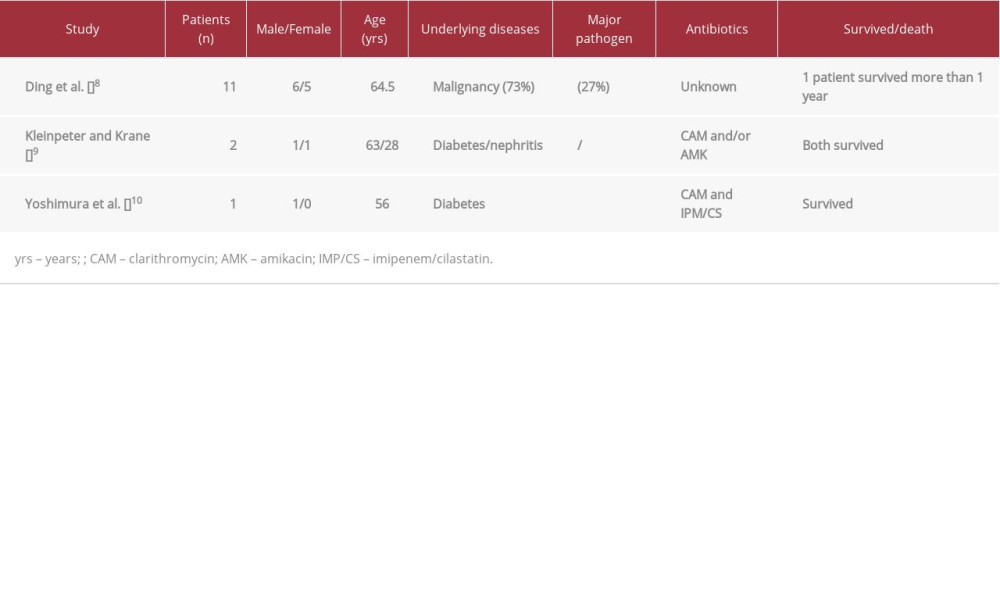 Table 2.. Reported peritonitis cases where Mycobacterium abscessus was isolated.
Table 2.. Reported peritonitis cases where Mycobacterium abscessus was isolated. In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








