18 August 2020: Articles 
Malignant Otitis External: Our Experience and Literature Review
Unusual clinical course, Challenging differential diagnosis, Unusual or unexpected effect of treatment, Patient complains / malpractice, Unexpected drug reaction, Educational Purpose (only if useful for a systematic review or synthesis)
Antonella M. Di Lullo12ACDEF*, Camilla Russo3DEF, Piera Piroli1BC, Alessandra Petti1BC, Pasquale Capriglione1BC, Elena Cantone1BC, Gaetano Motta4AD, Maurizio Iengo1ADE, Andrea Elefante3ADE, Michele Cavaliere1ACDEFDOI: 10.12659/AJCR.925060
Am J Case Rep 2020; 21:e925060
Abstract
BACKGROUND: Malignant external otitis (MEO) is an invasive infection that can involve the external auditory canal and the skull base up to the contiguous soft tissues. Considering the changing face of MEO, we reviewed cases of MEO treated in our Ear Nose Throat (ENT) clinic – University Federico II of Naples between 2018 and 2019 to evaluate the current epidemiology of the condition and to assess the state of art on diagnosis, therapeutic and follow-up management in our patients.
CASE REPORT: We present the cases of three male patients with Type 2 diabetes mellitus who complained of long-lasting otorrhea and pain, with clinical suspicion of MEO. In all cases, ear swab was positive for Pseudomonas aeruginosa. All our patients received a 6-week course of intravenous ciprofloxacin, piperacillin, and tazobactam, with rapid clinical symptoms improvement and complete recovery at 1-year follow-up.
CONCLUSIONS: MEO is difficult to treat due to the lack of standardized care guidelines. Patients with MEO often present with severe otalgia, edema, otorrhea, and facial nerve paralysis. Clinicians must suspect MEO in elderly diabetic and immunocompromised patients with persistent otalgia after external otitis. Imaging (computed tomography and magnetic resonance imaging) can play synergistic roles in the management of MEO. To evaluate eradication of the disease, clinicians have to assess clinical symptoms and signs as well as radiological imaging and inflammatory markers.
Keywords: Brain Diseases, Magnetic Resonance Imaging, otitis externa, Tomography, Emission-Computed, Ciprofloxacin, Diabetes Mellitus, Type 2, Pseudomonas aeruginosa
Background
Malignant external otitis (MEO) is an invasive infection. It can affect the external auditory canal up to the temporal bone (mastoid process) and the skull base [1–3]. Diagnosis can be delayed with significant morbidity and mortality [4].
This pathology affects commonly elderly patients with diabetes and impaired immune systems [1,2,5]. In most cases, MEO is caused by
When the index of clinical suspicion is high for MEO, computed tomography (CT) and magnetic resonance imaging (MRI) facilitate diagnosis and evaluation of disease progression [2]. To prevent recurrence after patient’s symptoms have improved, radionuclide scans, such as with Gallium – 67 – citrate (67Ga) or 111 Indium (111 In), can be performed to identify areas of active residual infection [8]. Treatment includes antibiotics (third-generation cephalosporins and fluoroquinolones such as ciprofloxacin) [1,9], local antibiotic washing of the external auditory canal, and finally surgery [2]. Some patients don’t respond to this treatment because of fungal infection (e.g.
Case Reports
CASE 1:
A 74-year-old white male (C.C.) with T2DM presented with hearing loss, right ear discharge, ipsilateral nasal respiratory obstruction, and worsening temporal for the last 5 months. Physical examination revealed a slight facial palsy on the right side - grade II on the House-Brackmann (HB) scale. Blood testing showed uncontrolled diabetes (monitoring HbA1c status), elevation of inflammatory indices including white blood cell (WBC) count, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Otoscopic examination showed bacterial right external otitis. An ear swab was positive for Pseudomonas aeruginosa, sensitive to ciprofloxacin. Rhino-pharyngolaryngoscopic examination with a flexible fiber (Olympus® ENF-V3 Rhinolaryngoscope) revealed right nasopharyngeal swelling. In addition, CT and contrast-enhanced MRI of the petrous bone were performed (Figure 1). CT scan (Figure 1A, 1B) showed asymmetric nasopharynx air lumen due to prominent soft tissue swelling on the right side, with opacification of the mastoid air cells; extensive erosive phenomena of the petrous bone and the pterygoid process were also visible (black arrowheads), along with areas of osteitic thickening of the mastoid (black arrow). MRI (Figure 1C–1F) showed a large area of altered signal within the right temporal bone extending from the pharyngeal mucosal, para-pharyngeal, and retro-pharyngeal spaces to the external auditory canal and retrocondylar fat tissue, with restricted diffusion and inhomogeneous post-contrast enhancement involving pterygoid muscles (white arrowhead) as well as the tensor and elevator muscles of the palatine veil. Local nerves and vascular structures were also involved, with mild reduction of the intra-petrous internal carotid artery flow signal and jugular bulb/upper internal jugular vein obliteration with slow flow in the sigmoid sinus (white arrow), probably due to external compression by the surrounding tissues. Therefore, imaging was consistent with external malignant otitis extending to the cranial base.
The patient received IV antibiotic treatment with ciprofloxacin (500 mg every 12 h) plus piperacillin and tazobactam (2 g+0.25 every 12 h) for 6 weeks. Because response to the therapy was rapid, it was not necessary to perform a nasopharyngeal biopsy.
The patient underwent clinical follow-up without neurological complications or facial nerve dysfunction. His symptoms regressed completed and CT performed 3 months later showed resolution of the inflammatory process of the external ear and the temporal bone. Follow-up at 1 year was negative for recurrence.
CASE 2:
A 76-year-old white male patient (M.E.) with bilaterally hearing aids and T2DM reported worsening otalgia in the left ear associated with itching and otorrhea for 1 month. Physical exam revealed purulent otorrhea and a polypoid neoformation occupying the left external auditory canal. Laboratory tests showed uncontrolled diabetes (monitoring HbA1c status), elevation of inflammatory parameters (WBC, ESR, and CRP). An ear swab was positive for Pseudomonas aeruginosa and sensitive to ciprofloxacin. Because the patient had bilateral middle-ear prosthetic devices after otosclerosis surgery more than 30 years ago (Figure 2A), only unenhanced and post-contrast CT of the petrous bone was performed (Figure 2). Basal CT scan showed secondary opacification of the left mastoid air cells compared to the normally aerated right side (Figure 2A, black arrowhead) and stenosing soft tissue thickening of the external auditory canal (Figure 2B, white arrowhead), with focal bony erosion of the inferior wall; extensive erosive phenomena of the temporal bone as well as the adjacent clivus were also present (Figure 2C, white arrows). After contrast injection (Figure 2D, 2E), there was asymmetrical swelling of the oropharynx on the left side with areas of diffuse contrast uptake extending to retropharyngeal, para-pharyngeal, and carotid space, while the masticator space was spared. Carotid space vessels were displaced, although opacification of the internal carotid artery and the internal jugular vein was preserved (Figure 2E, white circle); lumen reduction due to external compression without thrombosis of the internal jugular vein was present, with normal opacification of the transverse and sigmoid sinus above (Figure 2E, black arrow).
The patient received antibiotic therapy with ciprofloxacin (500 mg every 12 h) plus piperacillin and tazobactam (2 g+0.25 every 12 h) for 6 weeks, and surgery. The procedure was a left mastoidectomy with excision of polypoid neoformation occupying the left external auditory canal. Histological examination of the polypoid neoformation confirmed the inflammatory nature. The patient’s clinical symptoms completely resolved, and imaging follow-up 3 months later showed a reduction of the inflammatory area. Follow-up done recently at 1 year was negative for recurrence.
CASE 3:
A 77-year-old white male (P.R.) with T2DM presented with pain in the left temporal site with itching and otorrhea for 2 months. Otoscopy showed a polypoid neoformation in the left external auditory canal associated with purulent otorrhea. Rhino-pharyngo-laryngoscopy performed with flexible fiber (Olympus® ENF-V3 Rhinolaryngoscope) revealed a rhinopharynx neoformation on the left torus tubarius. An ear swab showed that Pseudomonas aeruginosa was the pathogenic agent of the external otitis, sensitive to ciprofloxacin. Unenhanced CT and contrast-enhanced MRI scans of the petrous bone were also performed to define disease extension (Figure 3). Basal CT scan showed stenosing soft tissue thickening of the left external auditory canal, with partial secondary opacification of mastoid air cells (Figure 3A) and focal erosion of the anterior canal wall (black arrow). MRI performed 2 weeks later showed progression of the radiological picture, with complete opacification of mastoid air cells (Figure 3B) and inhomogeneous diffusion signal restriction within retropharyngeal and parapharyngeal soft tissue (Figure 3C). After gadolinium administration (Figure 3D–3F), intense enhancement of retropharyngeal, carotid, and para-pharyngeal spaces was present, with initial involvement of the masticator space and retro-condylar soft tissues (white arrows) The internal carotid artery and internal jugular vein were patent, with reduced diameter compared to the opposite side (dotted line) due to external compression. Spongious and cortical clivus signal alteration was consistent with incipient skull base involvement (white arrowhead). The left external auditory canal and the rhinopharynx soft tissues were biopsied to assess the inflammatory origin of the lesion and confirm the diagnostic suspicion of MEO.
The patient received IV antibiotic therapy with ciprofloxacin (500 mg every 12h) and piperacillin plus tazobactam (2 g+0.25 every 12h) for 6 weeks. After therapy, he underwent a brain MRI with contrast extending to petrous bone, which was negative. At 1-year follow-up, he had the MEO had not recurred.
Discussion
MEO is an invasive and potentially fatal condition [2]. It is characterized by challenging management because of the need for long-term therapy requiring regular monitoring [1].
Misdiagnosed MEO can involve the skull base and cause major complications such as thrombosis of the lateral sinus or internal jugular vein, meningitis, Bezold’s abscess, and cranial nerves palsies [3]. In the literature, there is no a standardized protocol for management of MEO.
Patients with MEO often present with otalgia, which can be associated with temporal and occipital headache, otorrhea, edema, and granulation tissue, such as in our experience [1].
Today, there is great variability in criteria for diagnosis of MEO, which can result in delayed diagnosis of this serious disease. In the literature, some authors assume that the diagnosis of MEO is based on at least three of five of these signs and symptoms:Persistent external otitis;Granulation tissue in the external auditory canal;Radiographic confirmation of osteomyelitis of the external auditory canal, mastoid air cells and/or skull base;Cranial involvement;Isolation of
To our knowledge, diagnosis of MEO is based on high clinical suspicion. Notwithstanding, some authors such as Cohen and Friedman believe that presence of
Therefore, the most common criteria for diagnosis of MEO remain presence of granulations, otalgia, edema, otorrhea, and resistance to local therapy for at least 8 to 10 days, associated with diabetes, cranial nerve involvement, positive imaging, abnormal hematological parameters, immunocompromised status, and geriatric age [2,12,16].
Indeed, our patients had symptoms for at least 1 to 4 months without resolution and they were older than age 70 years.
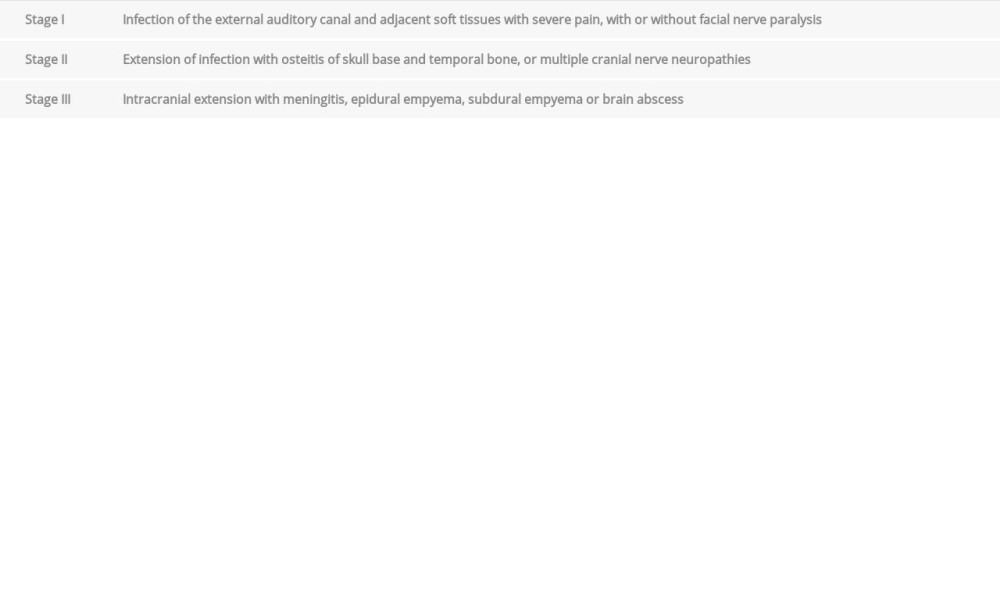
The progression of MEO has been divided into three clinical stages (Table 1) [6,17]. In our case series, all patients presented with stage II MEO.
MEO can be associated with other comorbidities such as diabetes, hypertension, and kidney and heart disease. In our study, all the patients were diabetic, and two had uncontrolled diabetes (monitoring HbA1c status). In fact, 80% diabetic patients have an increased risk of developing MEO [4]. That is owing to endarteritis, obliterating microangiopathies, and the high rate of infection that can cause ischemia and hypoxia of soft tissue in diabetic subjects [16]. In addition, pain sensitivity can be compromised in the elderly and in diabetic patients and can affect early diagnosis because real pain corresponding to the extent of disease becomes evident only in the advanced stage of MEO, contributing to diagnostic delay with this pathology.
At initial diagnosis, facial nerve palsy may be noted. It is often a characteristic of long-lasting MEO, with severe outcomes and irreversibility [2]. In our case series, one patient had mild facial palsy (HB degree II) from which he recovered.
According to the literature, patients with suspected MEO resistant to antibacterial regimens after 7 to 10 days should be switched to empirical antifungal treatment to reduce mortality, morbidity, and the eventual need for surgical intervention [2]. In general, MEO caused by fungal infections presents with fewer symptoms (pain, aural fullness) and affects immunocompromised patients, leading to diagnostic delays and more severe cases in this population [2].
The MEO treatment of choice remains third-generation cephalosporin, ceftazidime, fluoroquinolone, and carbapenems [1,18]. Oral ciprofloxacin should be prescribed early and at full dose for 6 to 8 weeks (as indicated for osteomyelitis) [20,21]. For late-stage, IV rather than oral therapy is preferable. Failure to respond to quinolone therapy should raise suspicion of
In severe cases that are unresponsive to medical treatment, surgical interventions are frequently proposed. Two of our patients underwent surgery, without complete control.
Moreover, Amaro CE et al. 2019 [2] reported on a small group of patients (16 subjects) treated for MEO with hyperbaric oxygen therapy (HBOT) in conjunction with antimicrobial therapy with good results.
Generally, the role of imaging techniques in MEO is to confirm diagnosis by defining disease extension and involvement of adjacent intra/extra-cranial structures and also providing useful information for post-treatment follow-up. Imaging assessment largely relies on unenhanced CT scan to evaluate bone remodelling and erosion, complemented by contrast-enhanced MRI examination to assess soft tissue involvement and possible complications such as intracranial extension, vascular compression or thrombosis and cranial nerve palsy.
Data from the literature show that high-resolution CT scan with multiplanar reformat is most commonly used as the first diagnostic approach [4], as it reveals bone erosion and demineralization. However, in early stages of MEO, bony erosion may not be evident [19]. Although CT scan can be used to assess soft tissue swelling and upper airway obstruction, contrast-enhanced MRI is the gold standard for soft tissue evaluation for a variety of head and neck and skull base disorders [4,25–32]. MRI (with reference to post-contrast volumetric T1w images) is particularly effective in assessing retrocondylar, parapharyngeal, masticator, parotid, and paraclival soft tissue invasion, and intracranial extension. With MRI, all four main routes of infection spread (anteriorly by temporomandibular joint, masticator space, and parotid gland; posteriorly by mastoid bone; medially by ipsilateral parapharyngeal fatty tissue and paraclival soft tissue; superiorly with dural involvement and intracranial extension) can be easily assessed [4]. With this background, all our patients underwent CT and then contrast-enhanced MRI to confirm diagnosis and for follow-up.
Published reports suggest that patients with MEO should be followed up for at least 1 year after therapy because of the high risk of recurrence [2,16]. In our clinical experience, no recurrences of this pathology have been seen after 1 year.
Furthermore, the follow-up may be possible with nuclear imaging. Indeed, Technetium-99m can reveal clinical improvement by mapping osteoblastic activity. Gallium-67 can be used to monitor treatment response, but it is expensive, time-consuming, and requires a high dose of radiation. FDG does not provide anatomical details because it binds rapidly to dividing cells such as leukocytes. In addition, positron emission tomography-CT (PET-CT) or PET-MRI have wide applications in oncology and can also be used to study infectious processes such as MEO [4].
Reports in the literature and our experience with MEO indicate that disease resolution is characterized by absence of pain, otorrhea and granulation and normalization of imaging and inflammatory markers (WBC, ESR, CRP) [2,16]. In the literature, the mortality rate for MEO has been estimated as approximately 42% [2].
Conclusions
MEO remains a pathology for which management is challenging because of the lack of a standardized care protocol. In our series, patients with MEO had severe otalgia, edema, otorrhea of the external auditory canal, and sometimes facial nerve paralysis. They were commonly elderly and had diabetes and were immunocompromised. In patients like this who have persistent severe otalgia after otitis externa, clinicians should have a high index of suspicion for MEO.
When MEO is diagnosed at a late stage, IV antibiotics are preferable for management.
CT and MRI have synergistic roles in the diagnosis and follow-up of patients with MEO. In fact, CT scans can underestimate the early stage of MEO and not reveal soft tissue changes. If clinical suspicion of MEO persists, however, it is crucial to perform MRI. To properly manage MEO and eradicate it, clinicians must assess clinical symptoms and signs and also evaluate results of radiological imaging and assays for inflammatory markers.
Figures
References:
1.. Marina S, Giutham MK, Rajeshwary A, A retrospective review of 14 cases of malignant otitis externa: J Otology, 2019; 14; 63-66
2.. Amaro CE, Espiney R, Radu L, Guerreiro F, Malignant (necrotizing) externa otitis: the experience of a single hyperbaric centre: Eur Arch Otorhinolaryngol, 2019; 276(7); 1881-87
3.. Singh A, Al Khabori M, Hyder MJ, Skull base ostemyelitis: Diagnostic and therapeutic challenges in atypical presentation: Otolaryngol Head Neck Surg, 2005; 133(1); 121-25
4.. Lau K, Scotta G, Wu K, A review of thirty-nine patients diagnosed with necrotising otitis externa over three years: Is CT imaging for diagnosis sufficient?: Clin Otolaryngol, 2020; 45(3); 414-18
5.. Liu XL, Peng H, Mo TT, Liang Y, Malignant otitis externa in a healthy non-diabetic patient: Eur Arch Otorhinolaryngol, 2016; 273(8); 2261-65
6.. Bovo R, Benatti A, Ciorba A, Pseudomonas and Aspergillus interaction in malignant external otitis: Risk of treatment failure: Acta Otorhinolaryngol Ital, 2012; 32(6); 416-19
7.. Ali T, Meade K, Anari S, Malignant otitis externa: Case series: J Laryngol Otol, 2010; 124(8); 846-51
8.. Courson AM, Vikram HR, Barrs DM, What are the criteria for terminating treatment for necrotizing (malignant) otitis externa?: Laryngoscope, 2014; 124(2); 361-62
9.. Vadish B, Ajaz A, Satheesh KB, Malignant otitis externa – a retrospective study of 15 patients treated in a tertiary healthcare center: J Int Adv Otol, 2015; 11(1); 72-76
10.. Hasibi M, Ashtiani MK, Motassadi Zarandi M, A treatment protocol for management of bacterial and fungal malignant external otitis: A large cohort in Tehran, Iran: Ann Otol Rhinol Laryngol, 2017; 126(7); 561-67
11.. Kraus DH, Rehm SJ, Kinney SE, The evolving treatment of necrotizing external otitis: Laryngoscope, 1988; 98(9); 934-39
12.. Cohen D, Friedman P, The diagnostic criteria of malignant external otitis: J Laryngol Otol, 1987; 101(3); 216-21
13.. Chen C, Chen Y, Yeh T: Acta Otolaryngol, 2010; 130(1); 89-94
14.. Cavaliere M, Bartoletti G, Capriglione P: Case Rep Med, 2020; 2020; 1710271
15.. Di Lullo AM, Scorza M, Amato F: Acta Otorhinolaryngol Ital, 2017; 37(3); 207-13
16.. Chawdhary G, Liow N, Democratis J, Whiteside O, Necrotising (malignant) otitis externa in the UK: A growing problem. Review of five cases and analysis of national Hospital Episode Statistics trends: J Laryngol Otol, 2015; 129(6); 600-3
17.. Davis JC, Gates GA, Lerner C, Adjuvant hyperbaric oxygen in malignant external otitis: Arch Otolaryngol Head Neck Surg, 1992; 118(1); 89-93
18.. Carfrae MJ, Kesser BW, Malignant otitis externa: Otolaryngol Clin North Am, 2008; 41(3); 537-49
19.. Loh S, Loh WS, Malignant otitis externa an Asian perspective on treatment outcomes and prognostic factors: Oltolaryngol Head Neck Surg, 2013; 148(6); 991-96
20.. Carek PJ, Dickerson LM, Sack JL, Diagnosis and management of osteomyelitis: Am Fam Physician, 2001; 63(12); 2413-20
21.. Lew DP, Waldvogel FA, Osteomyelitis: N Eng J Med, 1997; 336(14); 999-1007
22.. Hooper DC, Emerging mechanisms of fluoroquinolone resistance: Emerg Infect Dis, 2001; 7(2); 337-41
23.. Parsek MR, Singh PK, Bacterial biofilms: An emerging link to disease pathogenesis: Annu Rev Microbiol, 2003; 57; 677-701
24.. van Kroonenburgh AMJL, van der Meer WL, Bothof RJP, Advanced imaging techniques in skull base osteomyelitis due to malignant otitis externa: Curr Radiol Rep, 2018; 6(1); 3
25.. Cavaliere M, Di Lullo AM, Caruso A, Diffusion-weighted intensity magnetic resonance in the preoperative diagnosis of cholesteatoma: J Otorhinolaryngol Relat Spec, 2014; 76(4); 212-21
26.. Cavaliere M, Di Lullo AM, Cantone E: Eur Arch Otorhinolaryngol, 2018; 275(9); 2237-43
27.. Russo C, Elefante A, Di Lullo AM, ADC benchmark range for correct diagnosis of primary and recurrent middle ear cholesteatoma: Biomed Res Int, 2018; 2018; 7945482
28.. Russo C, Elefante A, Cavaliere M, Apparent diffusion coefficients for predicting primary chilesteatoma risk of recurrence after surgical clearance: Eur J Radiol, 2020; 125; 108915
29.. Elefante A, Cavaliere M, Russo C, Diffusion weighted MR imaging of primary and recurrent middle ear cholesteatoma: An assessment by readers with different expertise: Biomed Res Int, 2015; 2015; 597896
30.. Mesolella M, Iengo M, Testa D, Mucoepidermoid carcinoma of the base of tongue: Acta Otorhinolaryngol Ital, 2015; 35(1); 58-61
31.. Ottaviano G, Cantone E, D’Errico A, Sniffin’ Sticks and olfactory system imaging in patients with Kallmann syndrome: Int Forum Allergy Rhinol, 2015; 5(9); 855-61
32.. de Divitiis O, Elefante A, Cervical spinal brucellosis: A diagnostic and surgical challenge: World Neurosurg, 2012; 78(3–4); 257-59
Figures
In Press
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250