13 July 2021: Articles 
Cavitary Pneumonia Due to Methicillin-Resistant in a Non-Immunocompromised Patient After an Endoscopy: A Case Report
Rare coexistence of disease or pathology
Killen H. Briones-ClaudettDOI: 10.12659/AJCR.930136
Am J Case Rep 2021; 22:e930136
Abstract
BACKGROUND: Methicillin-resistant Staphylococcus aureus (MRSA) pneumonia has well-defined characteristics. We present a case of cavitary pneumonia due to MRSA in a patient who had undergone a recent outpatient gastroscopic procedure.
CASE REPORT: A 32-year-old man presented at the Emergency Department with tonic-clonic seizures of 2 min durations. He had a history of seizures without current treatment or use of psychostimulant drugs. His personal history referred to hypothyroidism treated with levothyroxine, morbid type 3 obesity, gastritis with a gastric ulcer, penicillin allergies, and an ambulatory endoscopy with a biopsy (7 days ago) for erosive gastropathy. On the 3rd day of admission to the Intensive Care Unit (ICU), a bronchoscopy was performed, which showed a reddened mucosa with hemorrhagic points and a cavitary area in the right main bronchus. Multiple polymerase chain reaction and mass spectrometry analyses of samples of bronchioalveolar lavage from the bronchus revealed MRSA with a mechanism of resistance to the mecA gene (1×10⁵ colony-forming unit/mL). The laboratory results for the cerebrospinal fluid were negative for bacterial growth.
CONCLUSIONS: This is a rare case of cavitary pneumonia due to MRSA of clinical and epidemiological characteristics, which is unusual after an outpatient endoscopic procedure.
Keywords: Bronchoalveolar Lavage Fluid, Gram-Positive Bacterial Infections, Methicillin-resistant Staphylococcus aureus, Anti-Bacterial Agents, Intensive Care Units, Pneumonia, Staphylococcal, Polymerase Chain Reaction, Staphylococcal Infections
Background
Methicillin-resistant
HA-MRSA preferentially selects immunocompromised individuals with long hospital stays, and its presence is associated with the insertion of some medical devices, a wide spectrum of clinical conditions associated with the respiratory tree, urinary tract, bloodstream, and postoperative infections with a limited response to antibiotic therapy.
CA-MRSA is seen in young individuals with environmental exposures and socioeconomic characteristics. These include a previous lack of health care, injection of illicit drugs, living in crowded places (prisons, barracks), and sharing of items (by athletes), including towels or razors that are infected or colonized by staphylococci, which are related to skin and soft tissue infections (85% to 90% of cases); <10% of these cause serious infections, especially community pneumonia.
The patients affected with CA-MRSA have less antimicrobial resistance than the strains found in HA-MRSA [4]. The resistance to methicillin in
MRSA has prompted a worldwide medical surveillance effort. In the last 20 years, MRSA strains have affected the community and have become a source of infection in healthy people [2]. The first case of CA-MRSA in Latin America was reported in Argentina, in a male patient with a history of chronic renal failure, active hemodialysis, and osteosynthesis of a hip fracture. He had a persistent fever after a traumatic displacement of the prosthesis [3]. The first MRSA strains were identified in Ecuador in 2017 [4]. Immunosuppression with symptoms of the lower respiratory tree was a common form of presentation of CA-MRSA [5,6]. We present an unusual case of cavitary pneumonia due to MRSA in a patient with antecedents from a gastroscopic procedure at an ambulatory endoscopic center.
Case Report
A 32-year-old man presented at the Emergency Department with tonic-clonic seizures of approximately 2-min durations. He had a previous history of seizures without current treatment or use of psychostimulant drugs. His personal pathological history referred to hypothyroidism treated with levothyroxine, morbid type 3 obesity, gastritis with a gastric ulcer, and penicillin allergies. Seven days before he presented at the Emergency Department, he had undergone an endoscopic procedure in an Outpatient Clinic for erosive gastropathy. There is no record of hospital admission prior to the endoscopic procedure, which was performed in an ambulatory endoscopic center. No adverse events related to the endoscopic procedure were reported. The patient had no history of illegal drug use.
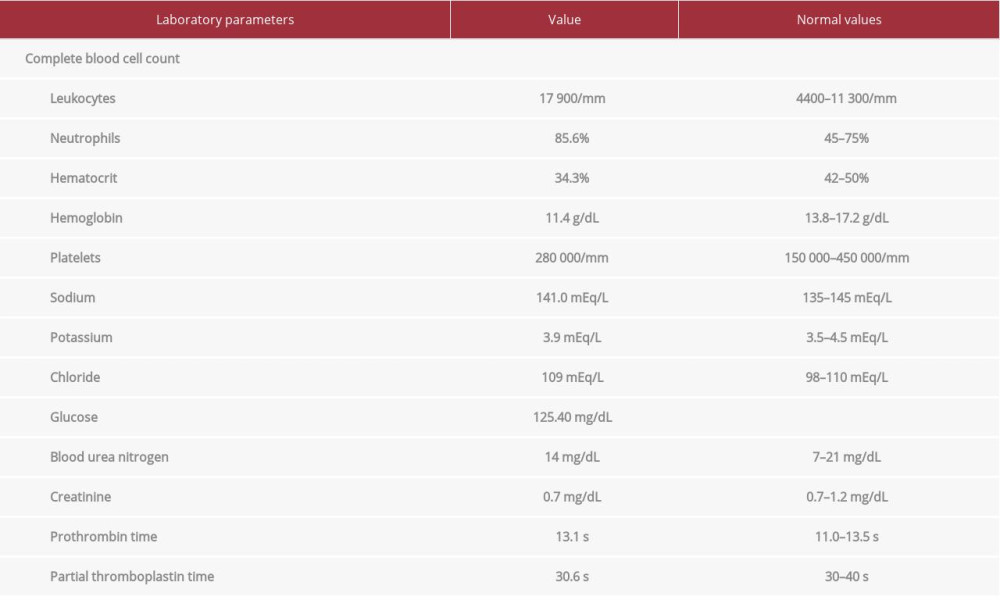
He was admitted to the Intensive Care Unit (ICU) for tonic-clonic seizures with hypoxemia. An endotracheal tube was placed and invasive mechanical ventilation was initiated. He remained under sedation with midazolam (0.25 mg/kg/h) and fentanyl (1.39 mg/kg/h) for analgesia. His laboratory test results are shown in Table 1. The chest X-ray showed a right basal atelectatic band, the computed tomography (CT) scan of the chest showed bilateral basal condensation areas, and the brain CT scan showed a normal brain (Figure 1A–1C).
Rational antibiotic therapy was initiated with piperacillin plus tazobactam and clindamycin before taking sputum, blood, and urine samples for cultures. During day 2 in the ICU, he remained sedated with midazolam (0.25 mg/kg/h) and fentanyl (1.39 mg/kg/h) for analgesia. On day 3 in the ICU, a bronchos-copy was performed, which showed a reddened mucosa with a cavity, hemorrhagic stitches, and active bleeding (Figure 2A–2C).
Samples of bronchioalveolar lavage were analyzed for pathogen identification. This was achieved by an automated system for extracting nucleic acids from the microbes (FilmArray™ multiplex PCR system, bioMérieux, France) and their identification by mass spectrometry (MALDI-TOF VITEK®MS system, bioMerieux, France). Antibiotic susceptibility testing and resistance mechanism was measured by an automated micro-dilution system (VITEK® 2, bioMerieux, France). Microbiological results from the bronchioalveolar lavage analysis showed the presence of MRSA (1×105 colony-forming unit [CFU]/mL) with mecA and luk-PV gene-resistance mechanisms.
Once the pathogen was identified from the bronchioalveolar lavage, the piperacillin plus tazobactam was suspended and he was administered intravenous vancomycin (1 g diluted in 250 mL of 0.9% sodium chloride/12 h). The laboratory results of the cerebrospinal fluid obtained by lumbar puncture on the first day of admission to the ICU showed no bacterial growth. On day 4, he showed significant clinical improvement; therefore, weaning of the sedation and invasive mechanical ventilation was initiated. On day 4, he was extubated with good ventilatory mechanics, 99% saturation, and retained oxygen support with a mask (3 L). The physical examination showed a respiratory rate of 19 breaths/min, he was oriented to time, space, and person, had a Glasgow Coma Scale score of 15/15, and reactive isochoric pupils. On day 5, he remained afebrile, awake, and breathing ambient air. After 6 days, he was discharged from the ICU, although he remained hospitalized. He was sent home after a 10-day hospital stay. He was followed up through the Outpatient Department and 6 months later he remains in general good health. He gave informed consent for the publication of this case report.
Discussion
The present case report is of an unusual presentation of a nonimmunocompromised patient who had MRSA with mecA-resistance mechanism, 1 week after an endoscopic procedure. MRSA can cause severe infections due to its superior ability to penetrate tissues. Our patient had no previous respiratory symptoms and no history of tobacco use, illicit drug use, or other associated diseases, including the human immunodeficiency virus. The Centers for Disease Control and Prevention’s criteria for defining CA-MRSA infection is a positive culture for MRSA as an outpatient or within 48 h after hospital admission, no presence of medical devices or permanent catheters placed through the skin, no history of MRSA infections, and no recent history of hospitalization or residence in nursing homes or long-term care facilities [7]. Many patients with CA-MRSA infections have previous injuries to the skin or soft tissues that are associated with the entry of the pathogen.
On the other hand, staphylococcal infections acquired by HAMRSA are defined as an infection or isolation of the pathogen occurring 72 h after hospital admission in patients with the recognized risk factors [8]. Clinical symptoms are characterized by prior association with an influenza infection with high fever, severe necrotizing pneumonia, leukopenia, respiratory failure, and shock, without any epidemiological link. The patient in the present case had seizures, although he was not on any prescribed antiepileptic medication when he presented in the Emergency Department, and had the history of an endoscopic procedure 7 days earlier in an ambulatory endos-copy center. Studies have shown that prior MRSA colonization of the nasopharynx is often associated with a peristomal infection [9]. However, he did not show nasopharyngeal colonization for
As the endoscopy was performed at an ambulatory endoscopic center, the endoscope cleaning and disinfection protocol could not be accessed due to their policies, practices, and information restrictions. Although models of endoscopic contamination have been reported in the literature [10], the presence of
Studies have observed that patients with infections due to the CA-MRSA-PVL gene-positive strains had a greater tendency toward leukocyte destruction and tissue necrosis, generally producing skin and soft tissue infections, and the most severe cases are associated with necrotizing pneumonia and sepsis [12].
The bronchoscopic study of our patient showed images of cavitary pneumonia that are typical of the aggression of MRSA with mecA-resistance mechanism. His response to the vancomycin was evidence that the clinical diagnosis was correct. It was achieved by sampling the bronchioalveolar lavage using the DNA extraction technique [13], which revealed MRSA with mecA-resistance mechanism.
Conclusions
We present an unusual case of cavitary pneumonia in a nonimmunocompromised patient, caused by methicillin-resistant
Figures
References:
1.. Mohammadi-Berenjestanaki H, Khori V: Microb Drug Resist, 2019; 26(3); 218-226
2.. Grundstad ML, Parlet CP, Kwiecinski JM: mSphere, 2019; 4(4); e00553-19
3.. Seas C, Garcia C, Salles MJ: J Antimicrob Chemother, 2018; 73(1); 212-22
4.. Eells SJ, McKinnell JA, Wang AA: Epidemiol Infect, 2013; 141(10); 2140-48
5.. Zurita J, Barba P, Ortega-Paredes D: Braz J Infect Dis, 2016; 20(6); 525-33
6.. Horan TC, Andrus M, Dudeck MA, CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. [published erratum appears in Am J Infect Control. 2008;36(9):655]: Am J Infect Control, 2008; 36(5); 309-32
7.. Woodhead M, Blasi F, Ewig S, Guidelines for the management of adult lower respiratory tract infections – full version: Clin Microbiol Infect, 2011; 17(Suppl. 6); E1-59
8.. Francis JS, Doherty MC, Lopatin U: Clin Infect Dis, 2005; 40(1); 100-7
9.. Sowash MG, Uhlemann AC: Methods Mol Biol, 2014; 1085; 25-69
10.. Greenwald DA, Ambulatory endoscopy centers: Infection-related issues: Techniques in Gastrointestinal Endoscopy, 2011; 13(4); 217-23
11.. Mainie I, Loughrey A, Watson J, Tham TC: J Clin Gastroenterol, 2006; 40(4); 297-300
12.. Voyich JM, Otto M, Mathema B: J Infect Dis, 2006; 194(12); 1761-70
13.. Labandeira-Rey M, Couzon F, Boisset S: Science, 2007; 315(5815); 1130-33
Figures
In Press
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942921
22 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943346
24 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943560
26 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943893
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250