24 August 2021: Articles 
Stylo-Jugular Venous Compression Syndrome: Lessons Based on a Case Report
Unusual clinical course, Challenging differential diagnosis, Management of emergency care, Rare disease
Renato Farina1ABCDEF*, Pietro Valerio Foti1BEF, Isabella Pennisi1BEF, Andrea Conti2BEF, Gaetano A. Meli2BEF, Tiziana Vasile2BE, Cecilia Gozzo2BE, Eliana Tallamona2BE, Corrado Inì2BE, Stefano Palmucci2BE, Massimo Venturini3BE, Antonio Basile2BEDOI: 10.12659/AJCR.932035
Am J Case Rep 2021; 22:e932035
Abstract
BACKGROUND: Eagle syndrome is a vascular compression syndrome that is caused by a very elongated styloid process and/or calcification of the stylohyoid ligament compressing the vascular or nerve structures of the neck, resulting in vascular congestion, thrombosis, or neurological symptoms (eg, dysphagia, neck pain, ear pain). Stylo-jugular venous compression syndrome is a subtype of Eagle syndrome and is caused by compression of the internal jugular vein. Treatment varies according to the symptoms and the severity of the compression, and it can be pharmacological or surgical, with vascular stenting and/or removal of the styloid process. We describe a rare case of left cerebral venous sinus thrombosis and ipsilateral internal jugular vein stenosis sustained by excessive length of the left styloid process.
CASE REPORT: A 36-year-old woman presented with recurrent episodes of drug-resistant headache and recent memory disturbances. She underwent cerebral and neck multidetector computed tomography-angiography and Doppler ultrasound of the epiaortic vessels that respectively revealed thrombosis of the left cerebral venous sinus and left internal jugular vein stenosis due to a very long styloid process. The patient was treated with anticoagulant drugs and experienced a gradual remission of symptoms.
CONCLUSIONS: Compression of the jugular vein by the styloid process is a rare entity, and it often goes undiagnosed when it is asymptomatic. Doppler ultrasound is a sensitive method for identifying jugular vein stenosis and can provide an estimated degree of stenosis, which is useful for treatment planning. Doppler ultrasound should be combined with multidetector computed tomography-angiography to rule out compression of other vascular structures and other causes of compression. Failure to treat these patients could have serious health consequences for them.
Keywords: Cerebral Veins, Eagle Syndrome, Jugular Veins, multidetector computed tomography, Ultrasonography, Ultrasonography, Doppler, Ossification, Heterotopic, Syndrome, Temporal Bone
Background
Eagle syndrome [1] is a vascular compression syndrome that is caused by a very elongated styloid process (SP) and/or calcification of the stylohyoid ligament compressing arterial vascular structures (carotid arteries) [2], venous structures (internal jugular vein) [3], or nerve structures [4]. Eagle syndrome is uncommon and has a higher incidence in women compared with men, with a ratio of 3: 1 [5]. The asymptomatic presence of 1 or 2 longer SPs occurs in 4% of the population [6]. Eagle syndrome can be unilateral or bilateral, and typical symptoms occur in only 4% of patients with a longer SP [7]. The symptoms most commonly associated with this pathology are recurrent episodes of pain in the face and throat, dysphagia, foreign body sensation in the pharynx, neck pain, and ear pain. The differential diagnosis should therefore be made with all other pathologies that can cause the above symptoms. Discovery occurs very often after routine multidetector computed tomography (MDCT) or Doppler ultrasound (DUS) examination of epiaortic vessels. A recent study suggested that the SP elongation or ossification may be explained by the occurrence of development abnormalities and/or altered bone homeostasis [8].
Eagle syndrome has been classified into subtypes based on the structures that are compressed: classic jugular venous compression syndrome, stylo-carotid syndrome, and stylojugular venous compression syndrome (SJVCS). The classical syndrome involves glossopharyngeal nerves but may also involve the V–VII and X nerves. The range of possible symptoms include tinnitus, otalgia, pharyngeal pain, dysphagia, foreign body sensation, pain on extending tongue, change in voice, and hypersalivation sensation, among others [9]. Stylo-carotid syndrome is caused by impingements of internal carotid arteries and leads to transient ischemic attack and stroke. Neurological symptoms such as hemiparesis and speech disturbance have also been reported [10]. SJVCS (Figure 1) is little known, and only a few reports mention it. The first study was published in 2012 [11], and a proposal was subsequently made to consider it an Eagle syndrome subtype and rename it Eagle-like jugular syndrome [12]. An elongated SP occurs in 4–28% of the population and is more common in women, with a mean age of 50±15 years [13]. Jayaraman et al [14] found that the right and left sides are equally affected, but the incidence of the left side is more common (right 24.1% vs left 30.6%). Compression occurs because the jugular vein wall, which is thinner than that of the artery and devoid of smooth muscle and elastic fibers, is more likely to be compressed by extrinsic structures in the upper neck, such as the transverse process of C1 and SP. SP induces jugular vein compression and causes venous flow congestion, which predisposes to thrombosis [15]. The J3 segment of jugular vein has been found to be the most frequently involved [16]. SJVCS has received more attention in recent years and several comorbidities have been found, including intracranial hypertension and a high-pressure gradient due to stenosis [17], thrombosis of the transverse sigmoid sinus, and perimesencephalic subarachnoid hemorrhage.
Three-dimensional computed tomography (CT) is the best method for evaluating the anatomical relationship between the SP and surrounding structures, such as nerves and blood vessels, and to measure the length and angle of the SP. CT also enables the exclusion of other causes of compression, and it provides details for the surgeon performing any extra- or intraoral excision. Therapy varies according to the symptoms and vascular compression. It can be conservative, with steroid, anticoagulant, or anesthetic drugs [18], or surgical, with SP removal [19] or endovascular stenting, which has been shown to be an effective treatment [20]. In this study, we describe a case of hemodynamically significant unilateral compression of the left internal jugular vein (LIJV) caused by a very long and anteri-orly angled SP that resulted in ipsilateral transverse cerebral venous sinus thrombosis.
Case Report
A 36-year-old woman presented at our hospital owing to increased episodes of drug-resistant headache and recurrent memory disturbances worsening in the past 2 weeks. The patient reported no past episodes of deep vein thrombosis or anemia, recent infections, or kidney or pulmonary disorders. In laboratory tests, the D-dimer value was above normal (1500 mg/L). The patient underwent MDCT-angiography of the brain and epiaortic vessels, DUS of the epiaortic vessels, and conventional X-ray examination of the head. The DUS study was performed with a MyLab 9 XG device (Esaote) using a 5- to 15-MHz linear probe. MDCT was performed with an Optima 64-slice device (GE Healthcare). Ultrasound scans were performed in the laterocervical region and measurements were made at 3 levels of the jugular veins in a cranio-caudal direction: J3, below the jugular foramen before the passage of the internal jugular vein (IJV); J2, at the level of the thyroid gland; and J1, in the segment where the IJV joins the subclavian vein to form the brachiocephalic vein.
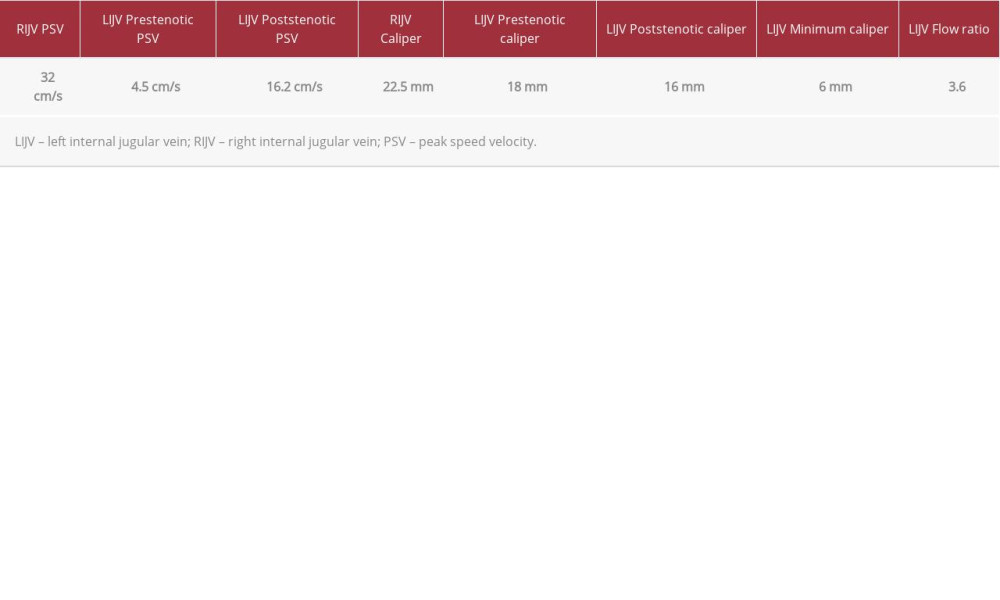
DUS was used to assess the caliber of the jugular veins and carotid arteries and the peak speed velocities (PSVs) of the common, internal, and external carotid arteries and the right and left IJVs (Figures 2, 3). The flow ratio of the LIJV was calculated from the prestenotic PSV divided by the poststenotic PSV). DUS showed stenosis of the LIJV (minimum caliber of 6 mm) with dilation of the prestenotic (maximum diameter of 18 mm) and poststenotic (maximum diameter of 16 mm) tracts and a flow ratio of 3.6 (prestenotic PSV, 4.5 cm/s; poststenotic PSV, 16.2 cm/s), which was equal to 72% stenosis. No morphological or fluximetric changes affecting the carotids bilaterally were highlighted. Compared to the left (Figure 3A, 3B; Video 1), right jugular vein was dilated (maximum diameter: 22.5 mm), with increased flow (Video 2) (PSV 38 cm/s). Ultrasound was performed by an operator with 20 years of experience, and the results are summarized in Table 1. On MDCT examination, the right SP had a length of 14.8 mm (Figure 4A). The left SP was longer than normal at 54.8 mm (Figure 4B) and lay at an angle anterior, compressing the ipsilateral IJV against the trans-verse process of C1 (Figure 4C). CT acquisitions with contrast medium showed a thrombosis of the left cerebral venous sinus, which could be seen in the reconstructions based on the axial (Figure 4D) and coronal (Figure 4E) planes. The patient declined to undergo surgical resection of the SP and was therefore only subjected to conservative drug treatment with low-molecular-weight heparin (100 U/kg subcutaneously twice daily) for 2 weeks followed by long-term oral anticoagulants (6 months). After 1 month the patient had a gradual and significant remission of headache episodes and a restoration of the normal values of D-dimer (<500 mg/L). We therefore advised the patient to continue the drug treatment and after 3 months to undergo cerebral MDCT-angiography.
Discussion
Given the clinical and laboratory data and the patient’s clinical history, particularly the recurrent episodes of headache, memory loss, and high D-dimer values, we suspected a cerebral problem (eg, embolism, ischemia, venous thrombosis) and decided to perform MDCT-angiography. Subsequently, the findings from DUS and the severity of the stenosis (>70%) highlighted vascular hyperflow in the contralateral jugular vein, demonstrating circulatory compensation. The discovery of a longer SP often happens by chance during routine CT or conventional radiographic examinations as it does not always cause compression of the vascular or nerve structures. Moreover, symptoms can also be caused by an SP of regular length but with an anomalous tip deviation [15]. Among the various radiological diagnostic criteria described in the literature, most authors define an SP length greater than 2.5 cm as abnormal [13], while others suggest 4.0 cm [16]. The average length of the SP found in SJCVS is 3.5–3.7 cm and the distance between the transverse process SP and C1 is 3.9 mm. Different imaging modalities can be used for Eagle syndrome study, including conventional head radiographs in lateral projection (Figure 5). However, radiographs do not always allow a correct visualization and measurement of the SP for the superimposition of the images. CT with contrast medium and 3-dimensional CT are the reference examinations that allow correct measurement of the length and angulation of the SP and evaluation of its relationships with the vascular and laterocervical nerve structures. In our case, the severe stenosis of the LIJV and the consequent venous hypertension probably induced the ipsilateral cerebral venous thrombosis. LIJV stenosis was revealed by DUS with a significant reduction or absence of flow in the stenotic tract, predominantly J3, and an increase in the contralateral flow (>30%). In the normal contra-lateral jugular vein, the maximum flow velocity was between 24 and 36 cm/s. A jugular vein contralateral dilation or tortuous vertebral venous plexus can be considered an expression of compensatory flow and may be a sign of SJVCS, but only occurs in 55.6% of severe strictures. Important data emerged in our study from the flow ratio measurement of the LIJV. The ratio was 3.2, corresponding to stenosis of 72%. These values indicate a very high risk of thrombosis, and the therapy of choice should be surgical removal of the SP. Endovascular therapy [17] could be a valid alternative but still requires more extensive case series and long-term data. In our case, the patient declined a styloidectomy, and we were not confident that there were sufficient guarantees for endovascular stenting in accordance with previous claims [18]. Long-term anticoagulant drug therapy should only be reserved for symptomatic cases with a flow ratio less than 2.5 (stenosis <50%).
Conclusions
IJV compression by the SP is a rare entity and can be asymptomatic, and most of the time it goes undiagnosed and treatment is delayed. DUS is a sensitive method for identifying IJV stenosis and can provide an estimate of the degree of stenosis, which is very useful for treatment planning. DUS examination should be combined with MDCT-angiography of the neck to rule out compression of other vascular structures and other causes of compression. In cases with light compression of the IJV and in patients who decline surgical treatment, we recommend a follow-up with DUS at 6 or 12 months. Failure to treat these patients, as in the case of other vascular compression syndromes [19–21], could have very serious consequences for the patients’ health.
Figures
References:
1.. Eagle WW, Elongated styloid processes: Report of two cases: Arch Otolaryngol, 1937; 25; 584-87
2.. Subedi R, Dean R, Baronos S, Dhamoon A, Carotid artery dissection: A rare complication of Eagle syndrome: BMJ Case Rep, 2017; 2017; bcr2016218184
3.. Suzuki Y, Toma N, Kuroda Y, Dural arteriovenous fistula formation as Eagle jugular syndrome: A case report and literature review: World Neurosurg, 2020; 144; 154-61
4.. Badheya A, Jategaonkara A, Kovacsb AJA, Eagle syndrome: A comprehensive review: Clin Neurol Neurosurg, 2017; 159; 34-38
5.. Quereshy FA, Gold ES, Arnold J, Powers MP, Eagle’s syndrome in an 11-year-old patient: J Oral Maxillofac Surg, 2001; 59; 94
6.. Okabe S, Morimoto Y, Ansai T, Clinical significance and variation of the advanced calcified stylohyoid complex detected by panoramic radiographs among 80-year-old subjects: Dentomaxillofac Radiol, 2006; 35; 191-99
7.. Prasad KC, Kamath MP, Reddy KJ, Elongated styloid process (Eagle’s syndrome): A clinical study: J Oral Maxillofac Surg, 2002; 60; 171-75
8.. Zamboni P, Scerrati A, Menegatti E, The eagle jugular syndrome: BMC Neurol, 2019; 19(1); 333
9.. Pokeerbux MR, Delmaire C, Morell-Dubois S, Styloidogenic compression of the internal jugular vein, a new venous entrapment syndrome?: Vasc Med, 2020; 25(4); 378-80
10.. Aydin E, Quliyev H, Cinar C, Eagle syndrome presenting with neurological symptoms: Turk Neurosurg, 2018; 28(2); 219-25
11.. Dashti SR, Nakaji P, Hu YC, Styloidogenic jugular venous compres-sion syndrome: Diagnosis and treatment: Case report: Neurosurgery, 2012; 70(3); E795-99
12.. Li M, Sun Y, Chan CC, Internal jugular vein stenosis associated with elongated styloid process: Five case reports and literature review: BMC Neurol, 2019; 19(1); 112
13.. Bai C, Wang Z, Guan J, Clinical characteristics and neuroimaging findings in eagle syndrome induced internal jugular vein stenosis: Ann Transl Med, 2020; 8(4); 97
14.. Jayaraman MV, Boxerman JL, Davis LM, Incidence of extrinsic compression of the internal jugular vein in unselected patients undergoing CT angiography: Am J Neuroradiol, 2012; 33(7); 1247-50
15.. Zhao X, Cavallo C, Hlubek RJ, Styloidogenic jugular venous compression syndrome: Clinical features and case series: Oper Neurosurg (Hagerstown), 2019; 17; 554-61
16.. Mooney J, Lepard J, Akbari SHA, Johnston JM, Styloidogenic jugular venous compression syndrome: A case report and review of the literature: Childs Nerv Syst, 2020; 36(12); 3135-39
17.. Han MK, Kim DW, Yang JY, Non-surgical treatment of Eagle’s syndrome – a case report: Korean J Pain, 2013; 26(2); 169-72
18.. Hooker JD, Joyner DA, Farley EP, Khan M, Carotid stent fracture from stylocarotid syndrome: J Radiol Case Rep, 2016; 10(6); 1-8
19.. Li M, Gao X, Rajah GB, Styloidectomy and venous stenting for treatment of styloid-induced internal jugular vein stenosis: A case report and literature review: World Neurosurg, 2019; 130; 129-32
20.. Farina R, Foti PV, Conti A, The role of ultrasound in Dunbar syndrome: Lessons based on a case report: Am J Case Rep, 2020; 21; e926778
21.. Farina R, Iannace FA, Foti PV, A case of Nutcracker syndrome combined with Wilkie syndrome with unusual clinical presentation: Am J Case Rep, 2020; 21; e922715
Figures
In Press
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250