20 October 2021: Articles 
Nine-Year Follow-Up of a Huge Retroperitoneal Alveolar Soft-Part Sarcoma: A Case Report
Rare disease
Dawid Janczak1ABDEF*, Tomasz Szydełko1ABDEF, Dariusz Janczak2ABDEFDOI: 10.12659/AJCR.932514
Am J Case Rep 2021; 22:e932514
Abstract
BACKGROUND: Alveolar soft-part sarcoma is an uncommon mesenchymal tumor accounting for approximately 0.7% of soft tissue sarcomas in adults. It mainly affects young adults, with a peak incidence between 15 and 35 years old. Available data indicate that surgical resection with adjuvant therapy using tyrosine kinase inhibitor may be considered the standard treatment. The rarity of the disease and resultant data scarcity makes it difficult to establish treatment guidelines.
CASE REPORT: We present the 9-year follow-up of a 24-year-old patient with an initially advanced (stage IV), huge, 21-cm alveolar soft-part sarcoma of the retroperitoneum. During the observation period, the patient developed pulmonary, brain, and bone metastases. In the course of treatment, she underwent excision of the main tumor, excision of satellite tumors, and brain metastasectomies, and was treated with sunitinib, pazopanib, and radiotherapy. No similar case reports were found in the PubMed database.
CONCLUSIONS: Our multimodal approach resulted in a long period of stable disease. Late progression may occur; therefore, frequent and thorough imaging evaluation of such patients is crucial. Our case is one of the largest ASPS tumors reported, and her long-term successful treatment makes this report valuable, considering the scarcity of data regarding treatment of ASPS. Further large-cohort, multi-center studies are necessary to establish the best treatment.
Keywords: Pazopanib, Sarcoma, Alveolar Soft Part, Soft Tissue Neoplasms, Adolescent, Bone Neoplasms, Female, Follow-Up Studies, Humans, young adult
Background
Alveolar soft-part sarcoma (ASPS) is an uncommon mesenchymal tumor accounting for approximately 0.7% of soft tissue sarcomas in adults [1,2]. The first report describing this type of neoplasm was published in 1952 [3]. It affects mainly young adults, with a peak incidence between 15 and 35 years old. Among patients younger than 30 years old females are more likely to be affected, and there are fewer cases in older patients. Recent studies have shown promising results with the use of tyrosine kinase inhibitors (TKI), but data on the use of novel treatment approaches is emerging. The rarity of the disease and resultant data scarcity makes it difficult to establish treatment guidelines [2,4,5].
The initial report about this patient, along with pathology figures and different CT scan figures, with 2 year follow-up, was published in 2014 [6]. Here, we present the 9-year follow-up of this patient with an initially advanced (stage IV), huge 21-cm retroperitoneal ASPS.
Case Report
A gradually enlarging bulge in the left groin was accidentally noticed by a 24-year-old woman, which was confirmed as a painless, palpable mass during medical examination. It was the only concern of the patient. No other abnormalities were present. Laboratory tests results were all within the standard limits. A CT scan showed a huge tumor that was 21 cm CC (craniocaudal)×9×6.5 cm AP (anteroposterior) occupying the left retroperitoneal space from the left kidney through the inguinal canal into the left groin (Figure 1). Another 2 tumors of the same morphology were found in the left pelvic area (4.7×4×5.8 cm and 2.4×1.8×2.3 cm). A lung CT scan showed multiple metastases with maximum size of 1.4 cm (Figure 2). No biopsy was performed preoperatively. Initial surgical treatment of the main tumor was chosen to avoid the effect of the tumor mass on the surrounding organs and to obtain the result of a histopathological examination. Due to good intra-operative surgical conditions, a complete R0 resection of the primary tumor was performed in May 2012. Unfortunately, excision of some lumbar plexus nerve branches was necessary to maintain the negative margin. Due to extension of the surgery, removal of satellite masses was postponed for a second operation. The histopathological examination found the tumor to be ASPS. A detailed description of the initial tumor resection and histopathological findings was published previously [6]. No genetic tests of the tumor were performed. With no signs of disease progression, sunitinib therapy was initiated 2 months after surgery (0.0375 g/day).
The first year of observation found no complications. On CT scans, metastases did not show any signs of progression, and the pelvic satellite masses showed slight regression. CT scans showed no recurrence of the primary tumor, slow regression of satellite masses, and no changes in the lung metastases. The patient had paresis of the left lower extremity and atrophia of adductor muscles of the left thigh. In May 2013, she experienced headaches of high intensity, which were caused by a 3.5×3.5×3.4 cm mass found on a CT scan of the brain (Figure 3). Excision of the tumor was performed and histo-pathological examination confirmed the diagnosis of ASPS metastasis. In July 2013, satellite masses in the pelvis were removed and histopathological examination again confirmed the diagnosis of ASPS metastasis.
During the next 2 years of follow-up, the patient was treated with sunitinib and no disease progression was detected by chest CT and abdominal or pelvis MRI every 3 months, and multiple brain MRIs. Three years after the initial surgery, she developed left hip pain, which was confirmed by MRI to be a metastasis in the left iliac bone (Figure 4). Due to bothersome symptoms, radiotherapy (39 Gy in 13 fractions) was performed, which achieved complete resolution of symptoms. Because of sunitinib treatment failure, the Oncology Department decided that the medical treatment should be changed. The patient was enrolled in a clinical trial with pazopanib 400 mg twice daily. At that time, the disease was located in the left iliac bone and in the lungs.
After the change of medical treatment regimen, no signs of disease progression were detected on radiological examination for 5.5 years. Multiple imaging tests were performed as a part of a pazopanib treatment program conducted in the Oncology Department, using computed tomography of the chest and abdominal or pelvic magnetic resonance imaging every 3 months. During treatment with pazopanib, the patient reported significant but bearable adverse effects: constant diarrhea, easy fatigability, episodes of abdominal pain or headache, lack of appetite, hair discoloration, and increased photosensitivity of the skin. A slow, constant decrease in BMI was observed, which currently is 16.67 kg/m2 (180 cm height, 54 kg weight).
In December 2020, 103 months since the primary operation, an MRI of the pelvis revealed a progression of iliac bone metastasis. Tumor infiltration in the left iliac bone (5.2×2×3 cm) was confirmed on the next MRI 2 months later (Figure 5). The patient then was asymptomatic and denied pain, which was present prior to radiotherapy.
It was decided to continue the medical treatment regimen with pazopanib and to perform radiotherapy of the metastasis in the left iliac bone. Initiation of radiotherapy was scheduled for March 2021.
The surveillance protocol was established by the Oncology Department and was unchanged since the primary surgery. It consisted of, alternately, an MRI of the abdomen or MRI of the pelvis every 3 months and a chest CT scan every 3 months. There was no imaging of the head before the onset of the headaches, which turned out to be caused by metastasis. After the cerebral metastasectomy, a head CT was performed once a year. A treatment summary is presented in Table 1.
Discussion
Alveolar soft-part sarcoma is an extremely rare type of tumor. According to a review published in JAMA Oncology in 2019, there were only 267 patients identified with ASPS in the USA between 1973 and 2014. It is caused by t(X;17)(p11; q25) translocation, which results in the creation of fusion gene ASPSLTFE3 [2].
The most common locations of primary tumors are the extremities (mainly thighs and buttocks, (58–60%), the trunk (16–28%), and head and neck region (12%). It may also have an origin in unusual sites such as the prostate, uterus, bladder, and breasts. Metastasis is usually to the lungs (90%), bone (26%), and brain (11–19%) [2,7–9]. Published reports showed a 3 times higher frequency of brain metastases compared to other sarcomas [10]. ASPS is characterized by an indolent progression with possible spontaneous stabilization or spontaneous regression of the disease [11]. The first symptom of the disease is usually a painless mass, which explains why in majority of patients the disease is detected at an advanced stadium (stage IV). In a recent paper by Flores et al, 5-year survival was 87% among patients with localized disease and 61% in those with metastatic disease [12]. According to published data, currently recommended treatments are surgical resection of the primary tumor and administration of tyrosine kinase inhibitors, among which pazopanib is most promising. During 19 months of follow-up (median), Stacchiotti et al found that of 30 enrolled patients with ASPS using pazopanib, 17 had stable disease, 7 had partial response, and 1 had complete response [13]. However, Liu et al presented better results with the use of Anlotinib compared to pazopanib, and they also showed that patients with a reduced dose of pazopanib due to adverse effects had significantly shorter progression-free survival [4]. The results of the only randomized trial investigating the treatment of ASPS with TKI were published in 2019 by Judson et al – the CASPS (Cediranib in patients with alveolar soft-part sarcoma) trial, showing significantly better clinical effect of cediranib compared to placebo [14].
Data on the use of new treatment regimens is emerging, combining radiotherapy with TKI and use of immune checkpoint inhibitors, but information is extremely limited [15]. Wilky et al published the results of a phase II study of axitinib plus pembrolizumab in patients with advanced sarcomas, including alveolar soft-part sarcoma. In this study, 6/11 patients with ASPS achieved a partial response and 2/11 achieved stable disease, with a clinical benefit rate of 72.7% [16].
Here, we report one of the largest ASPS tumors reported yet, and our long-term successful treatment makes it a valuable report considering the scarcity of data regarding treatment of ASPS. No similar publication was found in the PubMed database.
Conclusions
ASPS is an extremely uncommon entity. Available data suggest that the results of surgical resection and therapy using tyro-sine kinase inhibitors are satisfactory. Late progression may occur; therefore, frequent and thorough imaging evaluation of patients is crucial. In our case, this approach resulted in long-term period of stable disease, but what was the effect of the treatment applied and what was the impact of the tumor characteristics alone is unknown. Further large-cohort, multi-center studies are necessary to establish the best treatment.
Figures
Tables
Table 1.. Treatment summary.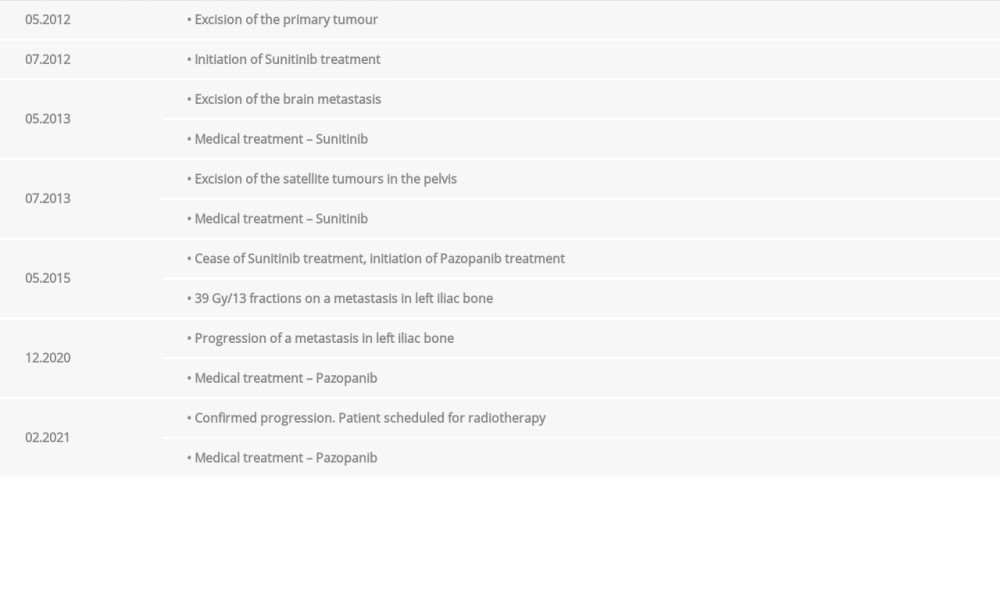
References:
1.. Orbach D, Brennan B, Casanova M, Paediatric and adolescent alveolar soft part sarcoma: A joint series from European cooperative groups: Pediatr Blood Cancer, 2013; 60(11); 1826-32
2.. Paoluzzi L, Maki RG, Diagnosis, prognosis, and treatment of alveolar soft-part sarcoma: JAMA Oncol, 2019; 5(2); 254
3.. Christopherson WM, Foote FW, Stewart FW, Alveolar soft-part sarcomas. Structurally characteristic tumors of uncertain histogenesis: Cancer, 1952; 5(1); 100-11
4.. Liu J, Fan Z, Li S, Target therapy for metastatic alveolar soft part sarcoma: A retrospective study with 47 cases: Ann Transl Med, 2020; 8(22); 1493
5.. Ye C, Wang J, Li W, Effective treatment of advanced alveolar soft part sarcoma with sunitinib: Medicine (Baltimore), 2018; 97(51); e13584
6.. Janczak D, Mimier M, Mimier A, Huge alveolar soft part sarcoma of the retroperitoneum: Polish J Pathol, 2014; 4(10); 327-30
7.. Wang Y, Du B, Yang M, He W, Paediatric orbital alveolar soft part sarcoma recurrence during long-term follow-up: A report of 3 cases and a review of the literature: BMC Ophthalmol, 2020; 20(1); 60
8.. Wang J-R, Rao Q, Li H, Alveolar soft-part sarcoma of the prostate: A case report and review of the literature: Int J Clin Exp Pathol, 2018; 11(10); 5126-32
9.. Asano Y, Kashiwagi S, Takada K, Alveolar soft part sarcoma metastatic to the breast: A case report: BMC Surg, 2019; 19(1); 30
10.. Ogura K, Beppu Y, Chuman H, Alveolar soft part sarcoma: A single-center 26-patient case series and review of the literature: Sarcoma, 2012; 2012; 1-6
11.. Stacchiotti S, Negri T, Zaffaroni N, Sunitinib in advanced alveolar soft part sarcoma: Evidence of a direct antitumor effect: Ann Oncol, 2011; 22(7); 1682-90
12.. Flores RJ, Harrison DJ, Federman N, Alveolar soft part sarcoma in children and young adults: A report of 69 cases: Pediatr Blood Cancer, 2018; 65(5); e26953
13.. Stacchiotti S, Mir O, Le Cesne A, Activity of pazopanib and trabectedin in advanced alveolar soft part sarcoma: Oncologist, 2018; 23(1); 62-70
14.. Judson I, Morden JP, Kilburn L, Cediranib in patients with alveolar soft-part sarcoma (CASPS): A double-blind, placebo-controlled, randomised, phase 2 trial: Lancet Oncol, 2019; 20(7); 1023-34
15.. Shinya Y, Hasegawa H, Kawashima M, Stereotactic radiosurgery as a primary treatment for metastatic skull base alveolar soft part sarcoma: A case report: Acta Neurochir (Wien), 2021; 163(2); 351-55
16.. Wilky BA, Trucco MM, Subhawong TK, Axitinib plus pembrolizumab in patients with advanced sarcomas including alveolar soft-part sarcoma: A single-centre, single-arm, phase 2 trial: Lancet Oncol, 2019; 20(6); 837-48
Figures
In Press
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








