24 November 2021: Articles 
Massive Hemorrhage Due to Cervical Endometriotic Cyst Rupture: Two Case Reports and a Literature Review
Management of emergency care, Rare disease
Yusuke Matoba1ABEF, Kosuke Tsuji1ABCEF*, Tohru Morisada1BDE, Mio Takahashi1BD, Yusuke Kobayashi1AEF, Masaru Nakamura1BD, Kouji Banno1EF, Daisuke Aoki1DEDOI: 10.12659/AJCR.934120
Am J Case Rep 2021; 22:e934120
Abstract
BACKGROUND: Endometriosis is defined as the growth of ectopic endometrial tissue beyond the uterine cavity, and endometriosis on the uterine cervix is a rare variant. Although asymptomatic patients with cervical endometriosis or those with minor symptoms are treated conservatively, there are reports of life-threatening hemorrhage due to cervical endometriosis. Here, we report 2 cases of massive genital bleeding caused by cervical endometriotic cysts and we performed a literature review.
CASE REPORT: Case 1: A 32-year-old woman presented to our hospital due to massive genital bleeding on her 11th day of menstruation. An arterial hemorrhage in a cervical endometriotic cyst was suspected. As pressure hemostasis proved difficult, urgent uterine artery embolization (UAE) by interventional radiology was performed. Angiography during the UAE showed extravascular leakage from the branch of the left uterine artery. After embolization, hemostasis was achieved. No further genital bleeding was observed, and transvaginal ultrasound showed the cyst has continued to shrink for 9 months after the UAE with sequential dienogest, a progesterone receptor agonist, treatment. Case 2: A 43-year-old woman presented to our hospital with increasing massive genital bleeding after completing a 12-day course of 0.5 mg of norgestrel and 0.05 mg of ethinyl estradiol as a treatment for irregular intermenstrual bleeding. We suspected cervical endometriotic cyst rupture on imaging and performed an urgent laparoscopic total hysterectomy. In the excised uterine specimen, a cystic lesion that contained old, blood-like fluid was macroscopically observed in the cervix and was diagnosed pathologically as endometriosis.
CONCLUSIONS: Cervical endometriotic cyst rupture is rare; however, it should be kept in mind as a differential diagnosis when treating massive genital bleeding because urgent intervention is sometimes required to control the bleeding.
Keywords: Endometriosis, hormonal contraception, Hysterectomy, Radiology, Interventional, uterine artery embolization, Uterine Cervical Diseases, Cervix Uteri, Cysts, Female, Hemorrhage, Humans, Uterine Hemorrhage
Background
Endometriosis is one of the most common benign gynecologic diseases, defined as the growth of ectopic endometrial tissue beyond the uterine cavity. It occurs in approximately 15% of women of reproductive age [1]. Cervical endometriosis is a rare variant of endometriosis. In a colposcopic examination series, the incidence of cervical endometriosis was reported to be between 0.11% and 2.4% [2] and it can be divided into 2 types: endometriosis on the superficial layer of the cervix and endometrial cell growth deep within the cervical stroma [3].
Asymptomatic patients with cervical endometriosis or those with minor symptoms are often treated conservatively with follow-up or low-dose oral contraceptives; however, there are reports of cases of life-threatening hemorrhage due to cervical endometriosis [4,5]. These patients require surgical treatments [5].
Here, we report 2 cases of massive bleeding due to cervical endometriotic cyst rupture that required blood transfusions and we performed a literature review.
Case Reports
CASE 1:
This was a 32-year-old nulligravida woman. She presented to our hospital’s Emergency Department due to sudden massive genital bleeding on her 11th day of menstruation. Her blood pressure and heart rate were 75/52 mmHg and 82 bpm, respectively, on arrival. Her serum hemoglobin was 11.4 g/dL. She had a negative pregnancy test. Transvaginal ultrasound (TVUS) with color Doppler showed arterial hemorrhage in a cervical cyst. This cyst was demonstrated previously on magnetic resonance imaging (MRI) and was suspected to be a cervical endometriotic cyst (Figure 1). As the patient’s recent cervical pap smear was negative for intraepithelial lesion or malignancy (NILM) and her endometrial cytology was negative, genital bleeding due to her known gynecologic malignancy was considered unlikely. An arterial hemorrhage in a cervical endometriotic cyst was considered most likely. As the pressure hemostasis proved difficult, and dynamic computed tomography demonstrated the same arterial hemorrhage in the cervical cyst, urgent uterine artery embolization (UAE) by interventional radiology was performed. Angiography during the UAE showed extravascular leakage from the peripheral branch of the left uterine artery (Figure 2). Main uterine artery trunk embolization was performed using a gelatin sponge, a temporary embolic material, and hemostasis was achieved. The measurable blood loss was 1000 mL. Two units of red blood cell were transfused intraoperatively. Postoperatively, there was no genital bleeding, and her hemoglobin level was 9.8 g/dL.
No further genital bleeding was observed, and the patient was discharged on the fifth postoperative day. After discharge, she started taking 2 mg of dienogest. The cyst was followed up with TVUS every 3 months at our clinic. Even when she stopped taking dienogest 9 months after the operation because she wanted to fall pregnant, and her menstruation resumed, TVUS every 3 months did not show the cervical cyst recurrence for one and a half years.
CASE 2:
This was a 43-year-old nulligravida woman. She visited our hospital’s Emergency Department due to an increasing amount of genital bleeding which began after she completed hormonal treatment for irregular intermenstrual bleeding. She was prescribed hormonal treatment by an outside clinic, which she visited after experiencing a few days of irregular intermenstrual bleeding. As the patient’s gynecologic examination and TVUS at the clinic did not identify a cause for the bleeding and the patient’s cervical cytology was NILM, she was prescribed a medium-dose oral contraceptive that contained 0.5 mg of norgestrel and 0.05 mg of ethinyl estradiol for 12 days. Five days after stopping this treatment, the patient’s genital bleeding re-started. After 7 days of bleeding, she noticed an increase in the amount of blood, at which point she presented to our Emergency Department. Her blood pressure and heart rate were 161/119 mmHg and 117 bpm, respectively. Her serum hemoglobin was 12.1 g/dL. Although massive uterine bleeding continued, a gynecologic examination including TVUS revealed no obvious uterine lesions. Functional uterine bleeding or withdrawal bleeding was suspected. She eventually lost consciousness. When the patient’s measurable blood loss reached 1200 mL and her hemoglobin level dropped to 8.7 g/dL, 4 units of red blood cell were transfused and pressure hemostasis with gauze was performed.
The gauze was removed the next day; however, she bled out again. An emergency MRI was performed, and bleeding due to cervical endometriotic cyst rupture was suspected (Figure 3). As she did not wish to preserve her fertility, an emergency laparoscopic total hysterectomy was performed. In the excised uterine specimen, a cystic lesion that contained old, blood-like fluid was macroscopically observed in the cervix. Histopathological examination revealed endometrial tissue in the lesion (Figure 4).
The postoperative course was good, and the patient was discharged on the fifth postoperative day.
Discussion
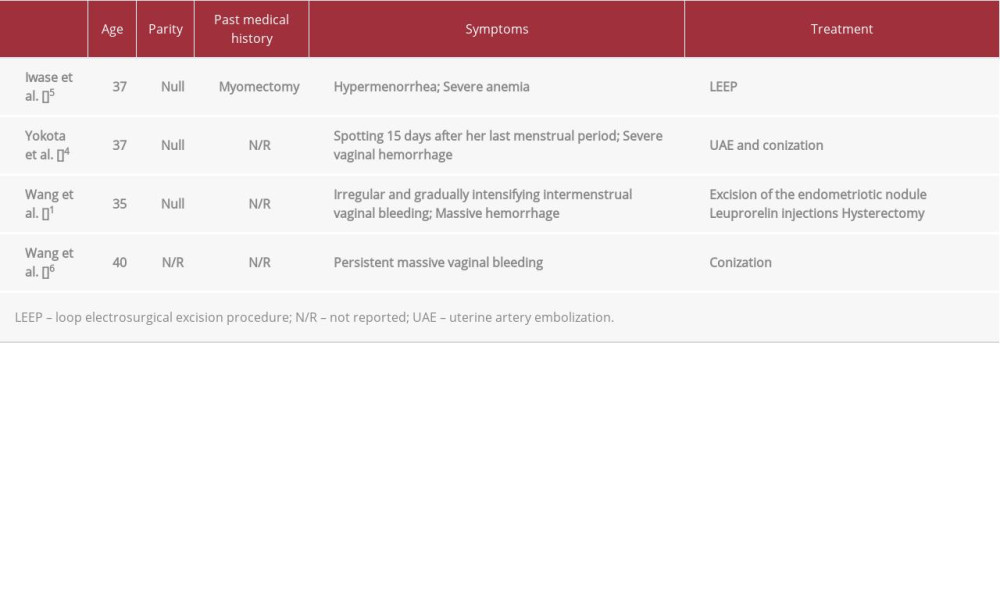
There are few reports of massive bleeding due to cervical endometriosis. We conducted a PubMed search of literature written in English on February 9, 2021, using the following search formula: (cervical[Title/Abstract]) AND ((endometriosis[Title/Abstract]) OR (adenomyotic cyst[Title/Abstract])) AND ((hemorrhage[Title/Abstract]) OR (bleeding[Title/Abstract])) and found 81 articles. A full-text review of each article was performed. Four articles reported on massive genital bleeding due to cervical endometriotic cysts [1,4–6]. In these reports, hysterectomy [1], LEEP [5], conization [4,6], gonadotropin-releasing hormone analog (GnRHa) administration [1], and UAE [4] were performed (Table 1) [1,4–6]. Because the cervical endometriotic cyst was large in our first case, complete cyst excision by LEEP or conization that included the bleeding site proved difficult, and surgery can result in further bleeding. Also, complete lesion excision including the bleeding site requires extensive cervical resection and can cause future perinatal complications in patients of childbearing age. Thus, UAE, where obstetrical complications are similar to the general population [7], was selected as the first intervention. In Case 1, as the causative vessel was identified, UAE achieved hemostasis. The patient was treated with dienogest after embolization with no bleeding, and there was no cervical cyst enlargement. Only 1 previous report included a case of UAE followed by conization [4]. Hormonal therapy after UAE may be a useful conservative treatment for childbearing age patients with cervical endometriotic cyst that causes massive bleeding as in Case 1.
There have been reports on low-dose oral contraceptive and GnRHa treatment for cervical endometriosis with minor symptoms [8]. Contrastingly, there was a report on a patient who was treated with GnRHa who had repeated bleeding that led to a hysterectomy [1]. The patient had received several doses of leuprorelin acetate and had massive bleeding several months after leuprorelin cessation. In our second case, a cervical endometriotic cyst ruptured and caused massive bleeding following medium-dose oral contraceptive treatment for irregular genital bleeding. Considering the pathogenesis of endometriosis, it is possible that the bleeding in the cervical cyst occurred due to withdrawal bleeding from the medium-dose oral contraceptive discontinuation. This may have contributed to rupture. As cervical endometriosis is one of the variants of endometriosis, withdrawal bleeding may trigger the uncontrolled bleeding as in Case 2. A hormonal therapy regimen that does not cause bleeding should be recommended.
Reports have suggested that cervical endometriosis is associated with surgical injuries such as conization and vaginal delivery [9]. However, both of our cases had no cervical surgery or delivery history. This suggests that there was little possibility that the cervical endometriotic cysts were caused by cervical injury. Studies have proposed that endometriosis lesions located deep in the cervix may be caused by residual endometrial cells in the cervical stroma, such as Müllerian duct tissue remnants[8, 10]. Both our cases and the previously reported cases were of deep cervical endometriosis. Considering the disease course in these cases, we propose that deep cervical endometriosis rarely causes minor symptoms such as post-coital bleeding or spotted bleeding; however, it may cause more serious symptoms if there is rupture. Since there have been few reports of similar cases, further research is needed to understand the origin and frequent manifestations of deep cervical endometriosis.
Cervical endometriosis is a cause of genital bleeding; however, bleeding can also be caused by cervical and endometrial cancers. In Case 1, cervical and endometrial cytology were negative; however, biopsy was not performed. In Case 2, pathological testing of the hysterectomy specimen confirmed that there were no malignant findings. As there has been a report of cervical adenocarcinoma arising from cervical endometriosis [11], cervical endometriosis lesions should be checked for potential malignant disease, especially in cases of heavy bleeding. However, a comprehensive pathological search may be difficult when the patient is of childbearing age or when the cervical endometriosis lesion is large, as in Case 1. For such cases, a strict follow-up, including image tests and observation of response to hormone therapy, must be required. As there is no consensus on the conservative management of patients with cervical endometriosis, further studies are needed.
Conclusions
Cervical endometriotic cyst rupture is rare; however, it causes massive, life-threatening bleeding which is, in some cases, hard to control without urgent intervention. As a result, cervical endometriotic cyst rupture should be kept as a differential diagnosis when treating massive genital bleeding.
Figures
References:
1.. Wang S, Li XC, Lang JH, Cervical endometriosis: Clinical character and management experience in a 27-year span: Am J Obstet Gynecol, 2011; 205(5); 452.e1-5
2.. Veiga-Ferreira MM, Leiman G, Dunbar F, Margolius KA, Cervical endometriosis: Facilitated diagnosis by fine needle aspiration cytologic testing: Am J Obstet Gynecol, 1987; 157(4 Pt 1); 849-56
3.. Phadnis SV, Doshi JS, Ogunnaike O, Cervical endometriosis: A diagnostic and management dilemma: Arch Gynecol Obstet, 2005; 272(4); 289-93
4.. Yokota N, Yoshida H, Sakakibara H, A severe vaginal hemorrhage caused by cervical endometriosis: Am J Obstet Gynecol, 2008; 199(1); e12-13
5.. Iwase A, Goto M, Kurotsuchi S, Successful management of a massive hemorrhage due to rupture of cystic cervical endometriosis by a loop electrosurgical excision procedure: Fertil Steril, 2008; 89(4); 991.e13-5
6.. Wang Y, Zhuge Y, Zhang Y, Massive vaginal hemorrhage caused by cervical endometriosis: Taiwan J Obstet Gynecol, 2018; 57(6); 903-5
7.. Ghanaati H, Sanaati M, Shakiba M, Pregnancy and its outcomes in patients after uterine fibroid embolization: A systematic review and meta-analysis: Cardiovasc Intervent Radiol, 2020; 43(8); 1122-33
8.. Kano H, Kanda H, Cervical endometriosis presented as a polypoid mass of portio cervix uteri: J Obstet Gynaecol, 2003; 23(1); 84-85
9.. Pollastro M, [Cervical endometriosis: Findings on a case secondary to diathermocoagulation.]: Minerva Ginecol, 1986; 38(12); 1013-14 [in Italian]
10.. Hoang NM, Smadja A, Orcel L, [Endometriosis of the uterine cervix. A hypothesis on its histogenesis.]: J Gynecol Obstet Biol Reprod (Paris), 1987; 16(5); 587-93 [in French]
11.. Uehara T, Yoshida H, Kondo A, Kato T, A case of cervical adenocarcinoma arising from endometriosis in the absence of human papilloma virus infection: J Obstet Gynaecol Res, 2020; 46(3); 536-41
Figures
In Press
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250