28 February 2023: Articles 
Improved Balance, Gait, and Lower Limb Motor Function in a 58-Year-Old Man with Right Hemiplegic Traumatic Brain Injury Following Virtual Reality-Based Real-Time Feedback Physical Therapy
Unusual clinical course, Challenging differential diagnosis, Unusual or unexpected effect of treatment, Diagnostic / therapeutic accidents
Kyung Hun Kim1ACDEG*, Dong Hoon Kim1BCDEFDOI: 10.12659/AJCR.938803
Am J Case Rep 2023; 24:e938803
Abstract
BACKGROUND: This report presents the case of a 58-year-old man with right hemiplegia who improved his gait and lower limb motor function following virtual reality (VR)-based physical therapy. The use of augmented reality or VR-based technology is being increasingly used to support physical therapy in patients with motor deficits and to improve gait, and can be used in small hospitals and outpatient departments.
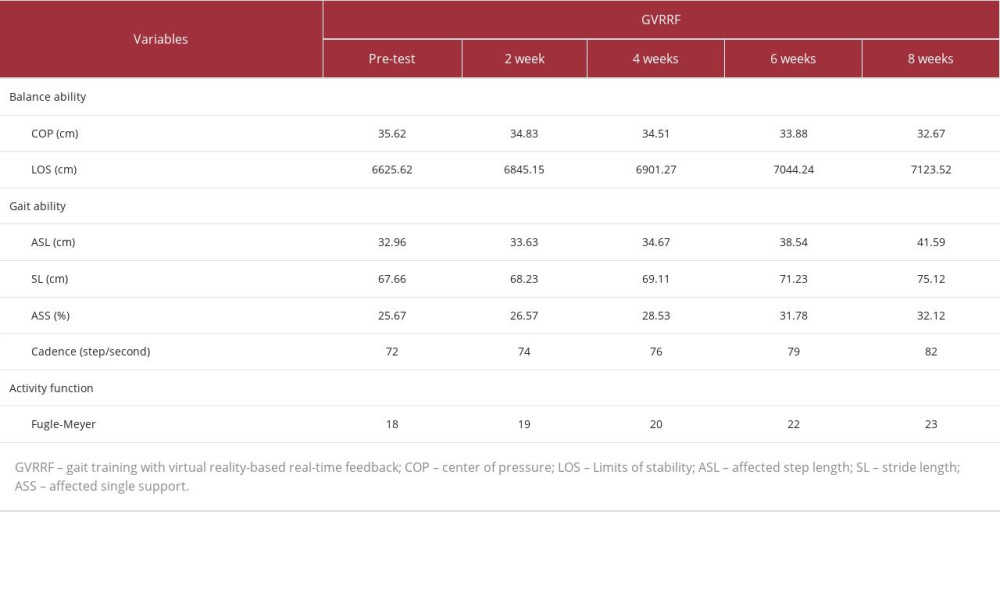
CASE REPORT: A 58-year-old man was diagnosed with left hemiplegia due to traumatic brain injury (TBI). He received 20 minutes of VR-based real-time feedback gait training and 30 minutes of general physical therapy, 5 times a week for 8 weeks. BioRescue was used for measurement of balance, GAITRite was used for measurement of gait, and Fugl-Meyer assessment was used for lower extremity motor function measurement. These were measured before the intervention and at 2, 4, 6, and 8 weeks after the intervention. After the intervention, center of pressure and limits of stability also increased. The affected step length, stride length, affected single support, and cadence were significantly increased after VR-based real-time feedback. Additionally, his lower extremity motor function score increased from 18 to 23 points.
CONCLUSIONS: This case report supports recent studies that have shown the value of VR-based methods as part of a physical therapy program in patients with problems with gait and motor function, including patients with stroke. VR-based real-time feedback showed favorable effects on rehabilitation following a TBI.
Keywords: virtual reality, case reports, Gait, Motor Skills, Physical Therapy Department, Hospital, Male, Humans, Middle Aged, Hemiplegia, Feedback, Brain Injuries, Traumatic, Lower Extremity
Background
Approximately 30% of patients with traumatic brain injury (TBI) have gait, balance, and motor dysfunction which vary depending on the injured area [1,2]. The most common chronic problem in patients with TBI is dysfunction in balance, which negatively affects physical function, independence, and quality of life. Moreover, injury may occur owing to a fall, and community participation may be limited [3–5]. TBI leads to alterations in brain function and pathology caused by a blow or other external force on the head [6]. As a major cause of disability and mortality, acquired brain injuries are increasingly being considered as a public health burden, placing significant economic strain on society [7].
Virtual reality (VR) uses interactive simulation generated by computer hardware and software to provide users an opportunity for involvement in an environment that mimics real objects or events [8]. A study reported that since VR uses multisensory visual, tactile, motor, and proprioceptive stimulation to induce real-world illusions, it allows the human mind to believe that the VR is real and enables functional movement training [9].
VR training has also been suggested to enhance neuroplasticity after stroke through high-intensity multisensory stimulation [10]. VR comprises computer-based real-time stimulation of an environment with user interaction visually displayed on a screen or through head-mounted devices. VR feedback can be mediated through vision, hearing, touch, movement, or smell. The technique provides performance feedback, both directly experienced and objectively quantified; increases exercise motivation; and improves motor performance [11]. VR and augmented reality, which combines real-world perception with computer-generated content, can be used as complementary treatment tools for rehabilitation and physiotherapy [12]. Currently, VR has been introduced to the functional training field for various diseases, including stroke, TBI, arthritis, spinal cord injury, attention deficit disorder, Parkinson’s disease, multiple sclerosis (MS), orthopedic impairment, and Alzheimer disease. Many studies and clinical investigations on its validity and possible therapeutic applications have been conducted [13–18].
Other previous studies have indicated that VR-based exercise could improve quality of life, even assisting in the recovery of mental health in neurologically impaired populations [19,20]. Recently, VR-based training has become an efficient intervention that has been widely used to provide feedback on characteristics of movement, enhanced motor learning, and recovery of muscle strength, balance, and gait ability, including recovery of activities of daily living in patients with brain injury [21]. Afsar et al (2018) reported that VR training led to significant improvement in upper extremity function in stroke patients [22]. In addition, another study demonstrated improvement in the walking ability of patients with hemiplegia by applying VR, in conjunction with partial body weight-supported treadmill training, and suggested that further studies combining VR, which has the advantage of improving motivation of the patients, with other treatments are needed [23].
Many studies are being conducted using VR as a treatment intervention in patients with brain injury, and based on previous studies, VR combined with other treatments was more effective than VR alone [24,25]. A randomized preliminary study by Tefertiller et al (2022) reported that 31 patients with TBI who underwent treadmill combined with VR training for 12 sessions over 4 weeks showed improvement in balance and mobility [26]. In a study that assessed balance ability using a portable VR-based Nintendo Wii system while the physical therapists monitored patients with mild TBI, improvement in both static and dynamic balance was demonstrated [27]. Thus, interventions combined with VR have been reported to be more significantly effective compared with the same interventions without VR.
Unfortunately, there are few studies on gait and balance rehabilitation in patients with TBI compared with studies of gait and balance rehabilitation in patients with nervous system injuries such as stroke and cerebral palsy [28]. In addition, limited evidence exists regarding the use of VR for TBI rehabilitation to improve motor and cognitive functions [29]. Since effective treatments are unknown, resolving gait and balance problems would be greatly helpful for patients with TBI, allowing them to improve their abilities.
Therefore, this case study aimed to investigate the effects of gait training with VR-based real-time feedback on balance and gait abilities and motor functions in patients with TBI.
Case Report
PATIENT HISTORY AND SYSTEMS REVIEW:
A 58-year-old man with TBI was hospitalized in Korea to receive comprehensive rehabilitation. The patient presented with headache, nausea, and vomiting after falling down a flight of stairs around 9: 00 pm on January 12, 2022. The patient presented at the hospital with headache and left-side muscle weakness. The patient had a positive Babinski sign and a recent medical history of asthma. The diagnosis was left-side hemiplegia due to right cerebral epidural hematoma. The numeric rating scale was used to qualify the headache, with the following characteristics: intensity, 8; location, head; type, pressure on the head; frequency, continuous; and duration, 1 h. During admission at the emergency department of the hospital, the patient manifested with altered consciousness, irritability, and left-sided weakness. Computed tomography revealed a large epidural hematoma in the right cerebral convexity (linear fracture in the right parietal bone and right temporal bone, squamous part, with midline shifting) (Figure 1). Moreover, a small intracerebral hemorrhage and contusion were observed in the left temporal lobe. The patient was admitted to the Neurology Department and underwent craniotomy for hematoma removal. After the operation, the patient was admitted to the intensive care unit and received conservative care. He was referred to the Rehabilitation Medical Department for continuing care.
After ≥6 months since the TBI diagnosis, the patient was able to ambulate using a walking assistive device. Further, the patient had no other neurological or orthopedic problems other than stroke, and was able to understand the training since his Korean Mini-Mental Status Examination score was ≥24 points.
The patient’s goals were to gain the ability to ambulate without a walking assistive device, improve his balance, and recover his independent outdoor mobility.
The study intervention was conducted after the patient voluntarily signed the informed consent form for participation. The study was approved by the Institutional Review Board of Gimcheon University (GU-202207-HRa-05-01-P).
MANAGEMENT:
In this case study, a treadmill, an Oculus Rift VR device, and smart insoles (R-C-SPO-Pedisol250, Pedisol, Korea) were used for gait training with VR-based real-time feedback. Regarding gait training with VR-based real-time feedback, the patient wore an Oculus Rift and performed gait training on a tread-mill (Quasar Med, Germany). Gait training was performed by visually confirming feedback information on real-time gait (Figures 2, 3). Treadmill gait speed was set at the patient’s comfortable speed. For VR-based gait training, a 3-dimensional outside gait environment was recorded in advance and uploaded to an online format. The recorded environment was played through the VR device and gait training was performed. A VR-based program session was set, composed of 10 min of walking and 10 min of walking downtown, with a total of 2 sessions. To prevent muscle fatigue and dizziness, a 2-min rest was taken by the patient after 1 session and then the subsequent session was performed [30]. Regarding real-time feedback, the patient with smart insoles on and in standing position performed gait training after ascertaining that the sensor was functional. The patient provided feedback on the center of pressure (COP) excursion and weight bearing on the unaffected and affected sides while performing gait training. The degree of this movement was displayed through bar graphs on both sides to improve weight shift and weight bearing on the unaffected and affected sides. The patient was informed in advance regarding the VR-based real-time feedback training, and it was explained that he needed to fully adapt and practice for 10 min before the intervention. Training with VR-based real-time feedback and general physical therapy were performed for 20 and 30 min, respectively. One physical therapist with 3 years of clinical experience and a master’s degree conducted the VR-based real-time feedback training and general physical therapy. General physical therapy consisted of range of motion exercises, stretching, upper and lower extremity muscle exercises, gait training, cycling training, Bobath therapy, and proprioceptive neuromuscular facilitation [31].
In the present study, general physical therapy and walking training with VR-based real-time feedback were performed. General physical therapy included range of motion exercise, core stability exercises, weight-bearing exercises, stretching, and balance and gait training [31]. The combined intervention was conducted for a total of 50 min, including a 30-min general physical therapy and 20-min walking training with VR-based real-time feedback. An exercise program was conducted for 30 min daily for 5 days a week for 8 weeks.
Balance and gait abilities and motor functions were assessed at baseline; at 2, 4, 6, and 8 weeks after the intervention; and at 2 weeks after followup.
A system for assessing and training balance ability (analysis system using biofeedback, AP1153 BioRescue, France) was used for evaluation. To assess the COP, the patient was asked to stand with his feet apart at approximately 30°, keep his eyes forward, and keep his balance for 1 min. The total travelled distance of the center of the body was also measured. Furthermore, limits of stability (LOS) values were measured using the BioRescue program. The center of gravity was moved to 8 different directions (front, back, left, right, and diagonals) to measure the migration length. Both feet were required to be on the force plate, and if the patient took his foot off the plate, the test was repeated from the beginning. The COP is used as a measure of postural control, and refers to the change in the point where ground reaction force is synthesized. It indicates the average weight of all pressure points in contact with the ground [32].
The GAITRite system (CIR Systems Inc Peekskill, NY, USA) was used to measure the gait ability of the patient. The mean and coefficient of variation for temporal and spatial parameters related to preferred-speed and fast-speed walking were measured twice. The patient was asked to stand in front of the gait mat and walk outside the gait mat at the most comfortable walking speed according to the inspector’s verbal signals. Temporal and spatial gait parameters were measured using the method by Shin et al (2013) [33]. In 2004, van Uden et al calculated rater reliability of this test to be γ=0.90, and correlation coefficients (ICC=0.99) in all gait measurements at comfortable walking speed were ≥0.96 [34].
Fugl-Meyer assessment (FMA) was used to assess the motor function of the patient. It is a tool measuring upper and lower extremity motor function recovery in patients with stroke. In our case, only the lower extremity motor function was measured [35]. The total score of the lower extremity motor function was 34. The test showed good test-retest and inter-rater reliabilities with excellent validity [36,37]. Measurement of balance ability revealed a COP distance of 35.62 cm and LOS of 6625.62 cm2. The gait ability was measured and the measurements of each item were as follows: affected step length (ASL), 32.96 cm; stride length, 67.66 cm; affected single support (ASS), 25.67%; and cadence, 72 step/min. Motor function was assessed and the FMA score was 18 out of 34 points.
The outcome and followup were as follows. Table 1 shows the changes in the motor functions and balance and gait abilities. Regarding balance ability, the COP distance was 35.62 cm at the pretest. It changed to 34.83 cm, 34.51 cm, 33.88 cm, and 32.67 cm at 2, 4, 6, and 8 weeks after the intervention, respectively, showing a gradual decrease. Regarding stability, LOS at pretest was 6625.62 cm2, but changed to 6845.15 cm2, 6901.27 cm2, 7044.24 cm2, and 7123.52 cm2 at 2, 4, 6, and 8 weeks after the intervention, respectively, showing a gradual increase. Regarding gait ability, the ASL at pretest was 32.96 cm. It changed to 33.63 cm, 34.67 cm, 38.54 cm, and 41.9 cm at 2, 4, 6, and 8 weeks after the intervention, respectively, showing a gradual increase. Regarding stride, the stride length at pretest was 67.66 cm. It changed to 68.23 cm, 69.11 cm, 71.23 cm, and 75.12 cm at 2, 4, 6, and 8 weeks after the intervention, respectively, showing a gradual increase. The ASS at pretest was 25.67%, and changed to 26.57%, 28.53%, 31.78%, and 32.12% at 2, 4, 6, and 8 weeks after the intervention, respectively, showing an improvement. The cadence at pretest was 72 steps/min, and increased to 74 steps/min, 76 steps/ min, 79 steps/min, and 82 steps/min at 2, 4, 6, and 8 weeks after the intervention, respectively, showing an improvement.
The FMA score at pretest was 18, and increased to 19, 20, 22, and 23 at 2, 4, 6, and 8 weeks after the intervention, respectively, showing a gradual increase.
Discussion
This is the first case study that investigated balance and gait abilities and motor functions in a middle-aged man with TBI. With respect to post-intervention gait ability, the COP decreased from 35.62 cm to 33.88 cm after 8 weeks, and the LOS increased from 6625.62 cm to 7123.52 cm after 8 weeks. Step length of the affected side and stride length, the measurements of gait ability, increased from 32.96 cm to 41.59 cm and 67.66 cm to 75.12 cm, respectively, after 8 weeks. ASS increased from 25.67% to 32.1% after 8 weeks. Cadence was increased from 72.00 steps/min to 82.00 steps/min after 8 weeks. Additionally, the lower extremity motor function score increased from 18 points to 23 points after 8 weeks. Training with VR-based real-time feedback in this study was performed for 2 weeks, and as the number of interventions increased, balance and gait abilities and motor functions improved.
Using BioRescue to investigate the change in balance after the intervention, we observed an improvement in the COP and LOS. A systematic review by Alashram et al (2022) reported that there is limited evidence on the effects of physical therapy for improving balance ability in patients with TBI [38]. A study by Thornton et al (2005) reported that balance ability, along with airway, breathing, and circulation measurements, in an experimental group who received VR, improved more than those in a control group who received only conventional balance training [39]. The present study has demonstrated that gait training with VR-based real-time feedback could improve the balance ability of patients with TBI. This result is similar to the results of a study by Palma et al (2011), in which VR-based training showed improvement in dynamic balance in pediatric patients with TBI [40]. In another recent study by Duque et al (2013), the balance ability of older people who completed the VR-based training program improved significantly [41]. A study by Song et al (2004) reported that VR-based training using visual feedback greatly affected weight shift and balance detection in healthy adults [42]. Our results confirm that immediate feedback leading to activation of proprioception via visual feedback improved the balance ability in our patient [43].
We used GAITRite to investigate the change in gait after the intervention, and an improvement in the temporal and spatial variation of gait was observed. In TBI, a gait problem occurs due to brain injury from an outside physical force rather than degenerative or congenital causes. Gait problems result from poor posture, difficulty in proper weight movement, stride length asymmetry, and slow gait speed [44,45]. Moreover, muscle imbalance, loss of balance, and ataxia owing to abnormal muscle rigidity may continue and lead to dependence and loss of work; thus, appropriate gait training is definitely required [46]. Studies by Lamontagne et al [47] and Yang et al [48] reported that a VR-based program conducted for patients with brain injury showed an increase in gait speed in all patients. A study reported that VR-based training using visual feedback improved gait ability in patients with MS [49]. Moreover, the results of this study, which are consistent with those from our study, reported that VR-based training using sensory feedback in patients with neurological disorders (MS, stroke, senile gait, and cerebral palsy) greatly improved balance and gait abilities [50]. This supports the result that VR-based training favorably affected gait ability. Our results are also consistent with a study that reported that balance is significantly correlated with gait speed [51].
The present study used FMA to investigate the change in motor function after the intervention, and an improvement in the score was observed. Reduced muscle length of the affected side and increased muscle length of the unaffected side are observed in patients with TBI, and abnormal muscle tightness (spasticity) causes muscle imbalance and poor posture [45]. Muscle function loss and limited joint range of motion cause immobilization, and an efficient recovery exercise program has been proposed to address these [52]. Our study demonstrated that gait training with VR-based real-time feedback could improve the motor functions of patients with TBI. Our study was conducted to investigate the effects of gait training with VR-based real-time feedback on motor functions of patients with TBI. A comparison of our results with results from previous studies is difficult, as there are very few studies on motor functions using VR-based real-time feedback. However, a systematic review reported that VR-based training was effective in improving upper and lower extremity motor functions in patients with stroke [24]. Aramaki et al (2019) used a video game-style VR-based intervention program for rehabilitation, and reported improvements in motor functions, dynamic balance, and quality of life [53]. This supported other findings that visual feedback through training with VR-based real-time feedback increased patients’ motivation, resulting in efficient weight shift and weight bearing on the affected side, and proper body alignment improved muscle use and motor functions on the affected side [23,29,30].
Conclusions
This study demonstrated that gait training with VR-based real-time feedback positively changed balance and gait ability and motor functions in a patient with TBI. This study is of clinical importance in that this is the first study that used gait training with VR-based real-time feedback in a patient with TBI. This case report supports recent studies that have shown the value of VR-based methods as part of a physical therapy program for patients with problems with gait and motor function, including patients with stroke.
Figures
References:
1.. Basford JR, Chou LS, Kaufman KR, An assessment of gait and balance deficits after traumatic brain injury: Arch Phys Med Rehabil, 2003; 84(3); 343-49
2.. Marshall S, Teasell R, Bayona N, Motor impairment rehabilitation post acquired brain injury: Brain Inj, 2007; 21(2); 133-60
3.. Fu TS, Jing R, McFaull SR, Recent trends in hospitalization and in-hospital mortality associated with traumatic brain injury in Canada: A nationwide, population-based study: J Trauma Acute Care Surg, 2015; 79; 449-54
4.. McCulloch KL, Buxton E, Hackney J, Balance, attention, and dual-task performance during walking after brain injury: associations with falls history: J Head Trauma Rehabil, 2010; 25; 155-63
5.. Winkler D, Unsworth C, Sloan S, Factors that lead to successful community integration following severe traumatic brain injury: J Head Trauma Rehabil, 2006; 21; 8-21
6.. Menon DK, Schwab K, Wright DW, Demographics and Clinical Assessment Working Group of the International Interagency Initiative toward Common Data Elements for Research on Traumatic Brain Injury Psychological Health. Position statement: Definition of traumatic brain injury: Arch Phys Med Rehabil, 2010; 91(11); 1637-40
7.. Humphreys I, Wood RL, Phillips CJ, The costs of traumatic brain injury: A literature review: Clinicoecon Outcomes Res, 2013; 5; 281-87
8.. Weiss PL, The potential of virtual reality for rehabilitation: J Rehabil Res Dev, 2004; 41(5); vii-x
9.. Bohil CJ, Alicea B, Biocca FA, Virtual reality in neuroscience research and therapy: Nat Rev Neurosci, 2011; 12(12); 752-62
10.. Hao J, Xie H, Harp K, Effects of virtual reality intervention on neural plasticity in stroke rehabilitation: A systematic review: Arch Phys Med Rehanil, 2022; 103(3); 523-41
11.. Tornbom K, Danielsson A, Experiences of treadmill walking with non-immersive virtual reality after stroke or acquired brain injury – a qualitative study: PLoS One, 2018; 13(12); e0209214
12.. Vinolo Gil MJ, Gonzalez-Medina G, Lucena-Anton D, Augmented reality in physical therapy: systematic review and meta-analysis: JMIR Serious Games, 2021; 9(4); e30985
13.. Broeren J, Rydmark M, Sunnerhagen KS, Virtual reality and haptics as a training device for movement rehabilitation after stroke: A single-case study: Arch Phys Med Rehabil, 2004; 85(8); 1247-50
14.. Christiansen C, Abreu K, Ottenbacher K, Task performance in virtual environments used for cognitive rehabilitation after traumatic brain injury: Arch Phys Med Rehabil, 1998; 79(8); 888-92
15.. Grealy MA, Johnson D, Rushton SK, Improving cognitive function after brain injury: The use of exercise and virtual reality: Arch Phys Med Rehabil, 1999; 80(6); 661-67
16.. Llorens R, Noe E, Colomer C, Effectiveness, usability, and cost- benefit of a virtual reality-based telerehabilitation program for balance recovery after stroke: A randomized controlled trial: Arch Phys Med Rehabil, 2015; 96(3); 418-25
17.. Llorens R, Gil-Gomez JA, Alcaniz M, Improvement in balance using a virtual reality-based stepping exercise: A randomized controlled trial involving individuals with chronic stroke: Clin Rehabil, 2015; 29(3); 261-68
18.. Rizzo AA, Buckwalter JG, The status of virtual reality for the cognitive rehabilitation of persons with neurological disorders and acquired brain injury: Stud Health Technol Inform, 1997; 39; 22-33
19.. Burdea G, Popescu V, Hentz V, Virtual reality-based orthopedic telerhabilitation: IEEE Trans Rehabil Eng, 2000; 8(3); 430-32
20.. Oliveira J, Gamito P, Souto T, Virtual reality-based cognitive stimulation on people with mild to moderate dementia due to Alzheimer’s disease: A pilot randomized controlled trial: Int J Environ Res Pubic Health, 2021; 18(10); 5290
21.. Laver KE, George S, Thomas S, Virtual reality for stroke rehabilitation: Safety, feasibility and application: J Appl Physiol, 2011; 116(11); 1426-34
22.. Ikbali Afsar S, Mirzayev I, Umit Yemisci O, Virtual reality in upper extremity rehabilitation of stroke patients: A randomized controlled trial: J Stroke Cerebrovasc Dis, 2018; 27(12); 3473-78
23.. Waker ML, Ringleb SI, Maihafer GC, Virtual reality enhanced partial body weight-supported treadmill training poststroke; Feasibility and effectiveness in 6 subjects: Arch Phys Med Rehabil, 2010; 91(1); 115-22
24.. Feng H, Li C, Liu J, Virtual reality rehabilitation versus conventional physical therapy for improving balance and gait in Parkinson’s disease patients; A randomized controlled trial: Med Sci Monit, 2019; 25; 4186-92
25.. Zhang B, Li D, Liu Y, Virtual reality for limb motor function, balance, gait, cognitive and daily function of stroke patients: A systematic review and meta-analysis: J Adv Nurs, 2021; 77(8); 3255-73
26.. Tefertiller C, Ketchum JM, Bartelt P, Feasibility of virtual reality and treadmill training in traumatic brain injury: A randomized controlled pilot trial: Brain Inj, 2022; 36(7); 898-908
27.. Cuthbert JP, Staniszewski K, Hays K, Virtual reality-based therapy for the treatment of balance deficits in patients receiving inpatient rehabilitation for traumatic brain injury: Brain Inj, 2014; 28(2); 181-88
28.. McFadyen BJ, Cantin JF, Swaine B, Modality-specific, multitask loco-motor deficits persist despite good recovery after a traumatic brain injury: Arch Phys Med Rehabil, 2009; 90(9); 1596-606
29.. Pietrzak E, Pullman S, McGuire A, Using virtual reality and videogames for traumatic brain injury rehabilitation: A structured literature review: Games Health J, 2014; 3(4); 202-14
30.. Hong SK, Lee GC, Effects of an immersive virtual reality environment on muscle strength, proprioception, balance, and gait of a middle-aged woman who had total knee replacement: A case report: Am J Case Rep, 2019; 20; 1636-42
31.. Yang YR, Chen IH, Liao KK, Cortical reorganization induced by body weight-supported treadmill training in patients with hemiparesis of different stroke durations: Arch Phys Med Rehabil, 2010; 91(4); 513-18
32.. Latash ML, Ferreira SS, Wieczorek SA, Movement sway: Changes in postural sway during voluntary shifts of the center of pressure: Exp Brain Res, 2003; 150(3); 314-24
33.. Shin S, Chung HR, Kistler BM, Walking and talking in maintenance hemodialysis patients: Arch Phys Med Rehabil, 2013; 94(1); 127-31
34.. van Uden CJ, Besser MP, Test-retest reliability of temporal and spatial gait characteristics measured with an instrumented walkway system (GAITRite): BMC Musculoskelet Disord, 2004; 5; 13
35.. Fugl-Meyer AR, Post-stroke hemiplegia assessment of physical properties: Scand J Rehabil Med Suppl, 1980; 7; 85-93
36.. Di Fabio RP, Badke MB, Relationship of sensory organization to balance function in patients with hemiplegia: Phys Ther, 1990; 70(9); 542-48
37.. Duncan PW, Propst M, Nelson SG, Reliability of the Fugl-Meyer assessment of sensorimotor recovery following cerebrovascular accident: Phys Ther, 1983; 63(10); 1606-10
38.. Alashram A, Padua E, Annino G, Virtual reality for balance and mobility rehabilitation following traumatic brain injury: A systematic review of randomized controlled trial: J Clin Neurosci, 2022; 105; 115-21
39.. Thornton M, Marshall S, McComas J, Benefits of activity and virtual reality based balance exercise programmes for adults with traumatic brain injury: Perceptions of participants and their caregivers: Brain Inj, 2015; 19(12); 989-1000
40.. Palma P, McFarling E, Flynn S, Is virtual reality gaming an effective adjunct to traditional therapy in children and adolescents with traumatic brain injury?: J Head Trauma Rehabil, 2011; 26; 409-10
41.. Duque G, Boersma D, Loza-Diaz G, Effects of balance training using a virtual-reality system in older fallers: Clin Interv Aging, 2013; 8; 257-63
42.. Song CG, Kim JY, Kim NG, A new postural balance control system for rehabilitation training based on virtual cycling: IEEE Trans Inf Technol Biomed, 2004; 8(2); 200-7
43.. Grewal GS, Sayeed R, Schwenk M, Balance rehabilitation: Promoting the role of virtual reality in patients with diabetic peripheral neuropathy: J Am Podiatr Med Assoc, 2013; 103(6); 498-507
44.. Ashley MJ: Traumatic brain injury: Rehabilitation, treatment. and case management, 2010, Boca Raton, CRC Press
45.. Ghez C, Posture: Principles of natural science, 1991, New York, Elsevier Michell
46.. Williams G, Morris ME, Schache A, Incidence of 68 gait abnormalities after traumatic brain injury: Arch Phys Med Rehabil, 2009; 90(4); 587-93
47.. Lamontagne A, Fung J, McFadyen BJ, Modulation of walking speed by changing optic flow in persons with stroke: J Neuroeng Rehabil, 2007; 4; 22-29
48.. Yang YR, Tsai MP, Chuang TY, Virtual reality-based training improves community ambulation in individuals with stroke: A randomized controlled trial: Gait Posture, 2008; 28; 201-6
49.. Baram Y, Miller A, Virtual reality cues for improvement of gait in patients with multiple sclerosis: Neurology, 2006; 66(2); 178-81
50.. Baram Y, Virtual sensory feedback for gait improvement in neurological patients: Front Neurol, 2013; 14; 138
51.. Perry J, Burnfield JM: Gait analysis, 2010, Thorofare, NJ, SLACK
52.. Iaccarino MA, Bhatnagar S, Zafonte R, Rehabilitation after traumatic brain injury: Handb Clin Neurol, 2015; 127; 411-22
53.. Aramaki AL, Sampaio RF, Reis ACS, Virtual reality in the rehabilitation of patients with stroke: an integrative review: Arq Neuropsiquiatr, 2019; 77(4); 268-78
Figures
In Press
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250