01 April 2023: Articles 
A Rare Nasopharyngeal Adenoid Cystic Carcinoma: Case Report and Literature Review
Unusual clinical course, Challenging differential diagnosis, Unusual or unexpected effect of treatment, Rare disease
Nawaf M. AlsubaieDOI: 10.12659/AJCR.938858
Am J Case Rep 2023; 24:e938858
Abstract
BACKGROUND: Adenoid cystic carcinoma (ACC) is a malignant tumor that involves the salivary glands and is rarely seen in the nasopharynx. It is characterized by pain, a high rate of recurrence, and poor survival rate and poor prognosis as it tends to invade the perineurium. Due to the ambiguity of patient presentations, most patients present at a late stage, at which point metastasis has already occurred.
CASE REPORT: The patient in this case report was an otherwise healthy 56-year-old male smoker who presented to the clinic in March 2022 complaining of nasal obstruction, mouth breathing, recurrent epistaxis, headache, and facial pain. He reported significant weight loss in the past 6 months. The nasal scope showed nasopharyngeal fullness and biopsy-confirmed ACC exhibiting tubular, solid, and focal cribriform growth patterns. Further work-up showed an advanced form of nasopharyngeal ACC with intracranial extension and lung metastasis. The patient received concurrent radiotherapy and chemotherapy. After 6 months, the patient reported an improvement in the pain, and repeated images showed regression of the tumor size.
CONCLUSIONS: ACC is a malignant disease that is rarely seen in the nasopharynx. Currently, the most commonly agreed upon management for resectable ACCs in the literature is through surgical resection with adjuvant radiotherapy. However, most of the reported cases received radiation and chemotherapy due to the difficulty and risk of radical surgical excision of nasopharyngeal malignant tumors. Patients should be followed up to rule out any local recurrence or distant metastasis.
Keywords: Carcinoma, Adenoid Cystic, Nasopharyngeal Neoplasms, Salivary Gland Neoplasms, Salivary Glands, Minor, Male, Humans, Middle Aged, nasopharyngeal carcinoma, Radiotherapy, Adjuvant, Pain
Background
Adenoid cystic carcinoma (ACC) is a malignant tumor that involves the salivary glands and is rarely seen in the nasopharynx [1]. ACC was first described in 1856 by Theodor Billroth as “cylindroma” due to its long amorphous compartments, which look like cylinders [2]. ACC accounts for about 4% of all epithelial salivary neoplasms and 1% of all head and neck malignancies [3,4]. Previous studies have concluded that nasopharyngeal ACC accounts for 0.48% of all nasopharyngeal cancers [5,6]. ACC is characterized by pain, a high rate of recurrence, poor survival rate, and poor prognosis as it tends to invade the perineurium [7].
Although ACC is considered a rare disease, the purpose of the present study is to highlight the discrepancy and complexity of patients’ presentations and the intricacy of its management approach. In this paper, we report a case of a nasopharyngeal mass diagnosed as ACC. Also, a comprehensive literature search was conducted using the PubMed, Web of Science, Google Scholar, and Saudi Digital Library databases. The articles were examined to extract information on treatment modalities and outcomes for ACC.
Case Report
The patient in this case report was an otherwise healthy 56-year-old male smoker who presented to the clinic in March 2022 complaining of nasal obstruction, mouth breathing, recurrent epistaxis, headache, and facial pain. He reported significant weight loss in the past 6 months. The nasal scope showed nasopharyngeal fullness due to an intact mass in the mucus with no ulceration or asymmetry. The tympanic membranes and cranial nerves were bilaterally intact. Computed tomography (CT) of the nasopharynx and sinuses with intravenous contrast reported a large nasopharyngeal mass with necrotic changes and invasion of the skull base, sphenoid, and pterygoid bones; more extensive destruction was seen on the right side; and abutment of the inferior aspect of the temporal lobe on the right side, with invasion of the sphenoid air sinus. An intraoperative biopsy was thus warranted and arranged; it was done on the mass located in the pharyngeal recess (Rossen Müller fossa). The results confirmed intermediate- to high-grade ACC. The biopsy confirmed that the tumor exhibited tubular, solid, and focal cribriform growth patterns (Figure 1). Magnetic resonance imaging (MRI) of the neck was then performed, and it showed a locally advanced nasopharyngeal carcinoma measuring 5.7×4.8×4.4 cm with parapharyngeal invasion of the clivus and base of the skull with intracranial extension. Invasion was also seen into the left cavernous sinus and left carotid canal, associated with multiple sites with small upper cervical lymphadenopathy (Figure 2). CT of the chest abdomen and pelvis revealed innumerable bilateral lung nodules in keeping with metastasis (Figure 3). There was no evidence of metastasis in the abdomen or pelvis.
The final staging of the mass was an advanced nasopharyngeal carcinoma with parapharyngeal invasion and intracranial extension with multiple sites of small upper cervical lymph-adenopathy and innumerable bilateral lung nodules, indicating lung metastasis suggestive of T4N1M1 (stage IVb). A board meeting was held, and a decision was made for palliative concurrent radiotherapy and chemotherapy. The patient was started on 1480 cGy in 4 fractions to the nasopharynx and skull base and was administered cisplatin, doxorubicin, and cyclophosphamide. In addition, the patient was referred to a pain management service.
In the 1-year followup period, the patient demonstrated significant improvement with regard to pain and discomfort. Also, he tolerated the chemoradiation sessions with minimal adverse effects. A followup MRI after therapy showed an interval decrease in the size of the invasive nasopharyngeal mass and a reduced enhancement pattern, with signal characterization of the central aspect of the tumor as well as the skull base indicating good local response (Figure 2). A fluorodeoxyglucose-positron emission tomography (PET) scan was performed after therapy showed significant interval decreases in size and number of previous multiple pulmonary nodules (Figure 3). As a result of this good initial response, additional high-dose radiation consisting of 5000 cGy in 20 fractions was offered to the patient. However, although this further measure might improve the disease control, it was still considered a component of a palliative management strategy. The patient agreed and is continuing his therapeutic plan, with satisfactory symptomatic control.
Discussion
ACC is a malignant epithelial tumor that commonly affects patients in the fifth decade of life [1]. Some studies have concluded that ACC accounts for 0.5–4% of all carcinomas in the nasopharynx [8,9]. Genetic susceptibility is thought to play a role in the development of ACC. Translocations resulting in fusion of the v
The typical histopathological features of ACC show 3 growth patterns: cribriform, tubular, and solid. Tubular patterns display the best prognosis, while solid patterns usually have the worst prognosis and a high incidence of distant metastasis [12,13]. Frequently, more than one subtype is seen, and occasionally, the 3 subtypes are seen together, which led Szanto et al to classify ACC into 3 grades: Grade 1, with tubular and crib-riform patterns without the solid pattern; Grade 2, mainly involving the cribriform pattern, with a less than 30% solid pattern; and Grade 3, which is mainly solid [14]. According to the World Health Organization, ACC tumors have “the propensity for perineural invasion,” “facial nerve paralysis may occur,” and ACC “can extend along nerves for a considerable distance beyond the clinically apparent boundaries of the tumor” [15].
The main challenge with regard to ACC is that it has an insidious onset and a slow growth rate. Thus, the tumor may go unnoticed as it can commonly present with nonspecific symptoms, such as epistaxis, aural fullness, nasal obstruction, or headaches. The interval between the onset of the disease and the onset of the first complaint is around 2–5 years [16,17].
ACC tumors tend to metastasize but seldom involve the lymph nodes [18]. Distant metastasis is present in about 30–60% of the cases, with the lung as the most involved site [1,19,20]. ACC is among the most common malignancies and is prone to perineural invasion (PNI). When PNI is present, it is considered a poor prognostic factor as it is sometimes believed to be the fourth pathway of metastasis after hematogenous spread, lymphatic spread, and direct invasion of the adjacent organs by the tumor [21].
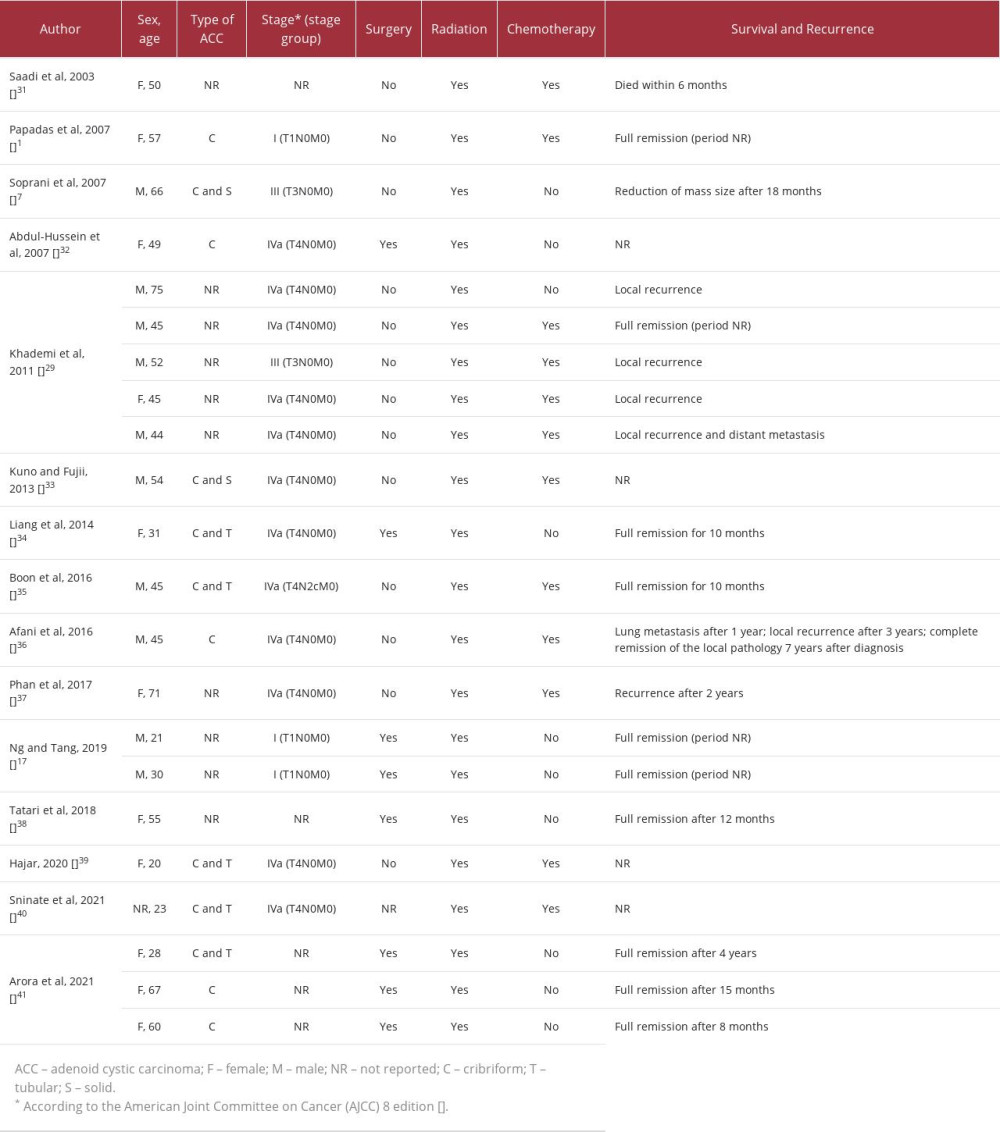
A retrospective study performed by Liu et al concluded that the optimal therapy for patients with nasopharyngeal ACC should involve surgical intervention, followed by radiotherapy; this approach has been shown to be most beneficial in patients with local infiltration and neural extension [19]. This approach has also been supported by many other authors [22–24]. A study conducted in 1993 on patients with ACC of the head and neck investigated the use of neutron radiotherapy for ACC. The results showed the superiority of the combined surgical-radio-therapeutic approach over surgical management alone [25]. However, radical surgical resection of malignant tumors in the nasopharynx is considered to be technically challenging and carries a high risk of morbidity and mortality due to presence of vital adjacent structures. This explains why most of the patients in the literature received chemotherapy and radiation rather than radical surgical excision (Table 1). Some reports have revealed good results and remission when chemotherapy was used concurrently with radiotherapy; however, the role of chemotherapy in ACC is not well understood, and no clear consensus exists [1].
In the presented case, the short-term outcome of concurrent chemoradiation was excellent in terms of symptom control and local regression of the tumor. As a result of this, in ACC cases where the tumor is surgically unresectable, concurrent chemoradiation may be offered as an alternative.
Radical surgical resection of ACC is challenging as it carries a high risk of morbidity and mortality due to the invasive nature of the tumor to adjacent structures, such as the cranial nerves and other vital organs [8,26,27]. However, the reported cases in the literature in which surgical management was undergone had a good disease-free interval (Table 1).
The prognosis of ACC depends on multiple factors, including tumor size, histopathologic characteristics, primary location of the tumor, metastasis, and cranial nerve involvement [14]. The 5-year survival rate ranges from 54.8% to 100% [19,27], while in cases with cranial nerve involvement or skull base invasion, the prognosis is generally dire [28].
Conclusions
ACC is a malignant disease that is rarely seen in the nasopharynx. When a mass is encountered in the nasopharynx alongside a clinical suspicion of ACC, MRI should be performed to determine the invasiveness of the mass. A biopsy is mandatory to confirm the diagnosis. Currently, the most commonly agreed upon management for resectable ACC cases in the literature is through surgical resection with adjuvant radiotherapy. However, in our reported case, the patient received concurrent chemoradiation and showed excellent results after 6 months in terms of symptom control and local regression of the tumor. Patients should be followed up to rule out any local recurrence or distant metastasis.
Figures
References:
1.. Papadas T, Chorianopoulos D, Mastronikolis N, Nasopharyngeal adenoid cystic carcinoma: A rare nasopharyngeal tumor: Eur Rev Med Pharmacol Sci, 2007; 11(1); 55-57
2.. Vidyalakshmi S, Aravindhan R, Adenoid cystic carcinoma of the buccal mucosa: A case report with review of literature: J Clin Diagn Res, 2014; 8(3); 266
3.. Spiro RH, Huvos AG, Strong EW, Adenoid cystic carcinoma of salivary origin. A clinicopathologic study of 242 cases: Am J Surg, 1974; 128(4); 512-20
4.. Ellis GL, Atlas of tumor pathology: Tumors of the salivary glands: Third Series, Fascicle 17 [online], 1996; 268 [cited 2022 Oct 18]; 17:
5.. He JH, Zong YS, Luo RZ, [Clinicopathological characteristics of primary nasopharyngeal adenocarcinoma.]: Ai Zheng, 2003; 22(7); 753-57 [in Chinese]
6.. Guo ZM, Liu WW, He JH, A retrospective cohort study of nasopharyngeal adenocarcinoma: A rare histological type of nasopharyngeal cancer: Clin Otolaryngol, 2009; 34(4); 322-27
7.. Soprani F, Armaroli V, Venturini A, A rare case of adenoid cystic carcinoma of the nasopharynx manifesting as Horner’s syndrome: Discussion and review of the literature: Acta Otorhinolaryngol Ital, 2007; 27(4); 216-19
8.. Lee DJ, Smith RR, Spaziani JT, Adenoid cystic carcinoma of the nasopharynx. Case reports and literature review: Ann Otol Rhinol Laryngol, 1985; 94(3); 269-72
9.. Mitani Y, Rao PH, Futreal PA, Novel chromosomal rearrangements and break points at the t(6;9) in salivary adenoid cystic carcinoma: association with MYB – NFIB chimeric fusion, MYB expression, and clinical outcome: Clin Cancer Res, 2011; 17(22); 7003-14
10.. Persson M, Andrén Y, Mark J, Recurrent fusion of MYB and NFIB transcription factor genes in carcinomas of the breast and head and neck: Proc Natl Acad Sci USA, 2009; 106(44); 18740-44
11.. Batsakis JG, Luna MA, El-Naggar A, Histopathologic grading of salivary gland neoplasms: III. Adenoid cystic carcinomas: Ann Otol Rhinol, 1990; 99(12); 1007-9
12.. Bradley PJ, Adenoid cystic carcinoma of the head and neck: A review: Curr Opin Otolaryngol Head Neck Surg, 2004; 12(2); 127-32
13.. Szanto PA, Luna MA, Tortoledo ME, White RA, Histologic grading of adenoid cystic carcinoma of the salivary glands: Cancer, 1984; 54(6); 1062-69
14.. El-Naggar A, Huvos A, Barnes L, World Health Organization classification of tumours: Pathology and genetics of head and neck tumors: IARC Press, 2005; 221-22
15.. Gormley WB, Sekhar LN, Wright DC, Management and long-term outcome of adenoid cystic carcinoma with intracranial extension: A neurosurgical perspective: Neurosurg, 1996; 38(6); 1105-12 ; discussion 1112–13
16.. Wang CC, See LC, Hong JH, Tang SG, Nasopharyngeal adenoid cystic carcinoma: Five new cases and a literature review: J Otolaryngol, 1996; 25(6); 399-403
17.. Ng BHK, Tang IP, Adenoid cystic carcinoma of the nasopharynx: A case series: Indian J Otolaryngol Head Neck Surg, 2019; 71(Suppl. 1); 731-33
18.. Liu TR, Yang AK, Guo X, Adenoid cystic carcinoma of the nasopharynx: 27-year experience: Laryngoscope, 2008; 118(11); 1981-88
19.. Seok J, Lee DY, Kim WS, Lung metastasis in adenoid cystic carcinoma of the head and neck: Head Neck, 2019; 41(11); 3976-83
20.. Liu X, Yang X, Zhan C, Perineural invasion in adenoid cystic carcinoma of the salivary glands: Where we are and where we need to go: Front Oncol, 2020; 10; 1493
21.. Shotton JC, Schmid S, Fisch U, The infratemporal fossa approach for adenoid cystic carcinoma of the skull base and nasopharynx: Otolaryngol Clin North Am, 1991; 24(6); 1445-64
22.. Pitman KT, Prokopakis EP, Aydogan B, The role of skull base surgery for the treatment of adenoid cystic carcinoma of the sinonasal tract: Head Neck, 1999; 21(5); 402-7
23.. Schramm VL, Imola MJ, Management of nasopharyngeal salivary gland malignancy: Laryngoscope, 2001; 111(9); 1533-44
24.. Buchholz TA, Shimotakahara SG, Weymuller EA, Neutron radiotherapy for adenoid cystic carcinoma of the head and neck: Arch Otolaryngol Head Neck Surg, 1993; 119(7); 747-52
25.. Amit M, Binenbaum Y, Sharma K, Adenoid cystic carcinoma of the nasal cavity and paranasal sinuses: A meta-analysis: J Neurol Surg B Skull Base, 2013; 74(3); 118-25
26.. Garden AS, Weber RS, Morrison WH, The influence of positive margins and nerve invasion in adenoid cystic carcinoma of the head and neck treated with surgery and radiation: Int J Radiat Oncol Biol Phys, 1995; 32(3); 619-26
27.. Kokemueller H, Eckardt A, Brachvogel P, Hausamen JE, Adenoid cystic carcinoma of the head and neck – a 20 years experience: Int J Oral Maxillofac Surg, 2004; 33(1); 25-31
28.. Issing PR, Hemmanouil I, Stöver T, Adenoid cystic carcinoma of the skull base: Skull Base Surg, 1999; 9(4); 271-75
29.. Khademi B, Bahranifard H, Kabiri S, Nasopharyngeal adenoid cystic carcinoma: Report of five cases and treatment outcome: Middle East J Cancer, 2011; 2(2); 81-85
30.. Lee J il, Kim YZ, Lee EH, Kim KH, Skull base invasion of adenoid cystic carcinoma of the lacrimal gland: A case report: J Korean Neurosurg Soc, 2008; 44(4); 273-76
31.. Saâdi I, el Marfany M, Hadadi K, [Adenoid cystic carcinoma of the nasopharynx: a case report.]: Cancer Radiother, 2003; 7(3); 190-94 [in French]
32.. Abdul-Hussein A, Morris PA, Markova T, An unusual presentation of adenoid cystic carcinoma of the minor salivary glands with cranial nerve palsy: A case study: BMC Cancer, 2007; 7; 157
33.. Kuno H, Fujii S, A case of adenoid cystic carcinoma arising from the nasopharynx: Jpn J Clin Oncol, 2013; 43(9); 942
34.. Liang YF, Kong B, Xiang WY, Nasopharyngeal adenoid cystic carcinoma: A case report and review of the literature: Int J Clin Exp Pathol, 2014; 7(7); 4516-18
35.. Boon IS, Warfield AT, Ahmed SK, Dedifferentiated adenoid cystic carcinoma of the nasopharynx: A rare entity of head and neck cancer: BMJ Case Rep, 2016; 2016; bcr2016215889
36.. Afani L, Errihani H, Benchafai I, Lalami Y, [Nasopharyngeal adenoid cystic carcinoma, a rare but highly challenging disease with unmet therapeutic needs: A case-report and review of the literature.]: Cancer Radiother, 2016; 20(5); 400-44 [in French]
37.. Phan J, Ng SP, Pollard C, Phan J, A rare case of unresectable adenoid cystic carcinoma of the nasopharynx treated with intensity modulated proton therapy: Cureus, 2017; 9(9); e1688
38.. Tatari MM, Anajar S, Hassnaoui J, Nasopharyngeal adenoid cystic carcinoma, suggestion of therapeutic innovations: A case report and review of literature: Ann Med Surg (Lond), 2018; 30; 32-35
39.. Tojumi SH, Seka E, Aarab J, An unusual case of nasopharyngial adenoid cystic carcinoma with intracranial and orbital extension: A challenge for innovative conformal radiotherapy techniques: Ann Clin Med Case Rep, 2020; 4(2); 1-3
40.. Sninate S, Allioui S, Tbouda M, Jerguigue H, Latib R, Omor Y, Nasopharyngeal adenoid cystic carcinoma presenting with exophthalmos: A case report: Radiol Case Rep, 2021; 16(4); 956-60
41.. Arora V, Yadav V, Mandal G, Adenoid cystic carcinoma of the nasopharynx – a rare entity: Our institutional experience and therapeutic approach: Indian J Surg Oncol, 2021; 12(2); 428-31
42.. Amin MB, Edge S, Greene F: AJCC cancer staging manual, 2017
Figures
In Press
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250