16 September 2023: Articles 
Tourniquet-Related Nerve Injury Following Reconstructive Surgery for Wassel Type IV Preaxial Polydactyly of 13-Year-Old Boy: A Case Report
Unusual or unexpected effect of treatment, Diagnostic / therapeutic accidents, Rare disease, Congenital defects / diseases, Clinical situation which can not be reproduced for ethical reasons
Hilmi MuhammadDOI: 10.12659/AJCR.940977
Am J Case Rep 2023; 24:e940977
Abstract
BACKGROUND: Congenital thumb duplication comes under the Wassel type IV classification is the hypoplastic variety, with the extra digit growing from the dominant thumb’s soft tissue alone. Excising the hypoplastic finger while reconstructing for the retained one has been the most adopted approach. Tourniquets are commonly utilized tools in orthopedic surgeries to reduce the amount of blood, thus enhancing the visibility. Unfortunately, tourniquet-related nerve injury (TNRI) is gaining more attention as a serious complication of tourniquet use in surgery.
CASE REPORT: A 13-year-old Asian boy with preaxial polydactyly Wassel type IV of the right hand underwent reconstruction surgery. A pneumatic tourniquet was applied at 200 mmHg on the right mid-upper arm and maintained for 90 min. After the surgery, the patient had total weakness with numbness, tingling, and burning sensation from his right upper arm to his fingertips. The neurological examination and nerve conduction studies (NCS) results were consistent with axonotmesis lesions. Pharmacological and physical rehabilitation therapy had successfully restored full motoric and sensory function after 6 months.
CONCLUSIONS: Nerve injury should be acknowledged as a possible complication from routinely-utilized tourniquets in orthopedic surgeries. Our cases may expand the need for further studies to establish a guideline for tourniquet use and TRNI management.
Keywords: Pediatrics, Physical and Rehabilitation Medicine, Polydactyly, Preaxial 4, Trauma, Nervous System, Male, Humans, Adolescent, Surgery, Plastic, Tourniquets, Hand, Thumb, Paresthesia, Polydactyly
Background
Congenital malformation of the hand with additional digits, known as polydactyly, can be found as frequent as 0.08 to 1.4 in every 1000 live births. The extra fingers may be found on the radial, ulnar, or central part of the hand. The preaxial polydactyly manifestation ranges from mild malformation of an isolated split distal part of a digit to a whole developed set of extra fingers with their own carpal bones. Usually, the duplicated digit(s) are underdeveloped and serve no function [1].
Wassel (1969) developed a classification, based on the amount of bone components of the duplicated thumb, into 7 groups, and this classification became the most extensively used categorization method for preaxial polydactyly [2]. Wassel classification starts from type 1 with only bifid distal phalanx to type 6 with duplicated metacarpal. Odd numbers signify bifid osseous structures. Even numbers indicate duplicated bones and higher numbers describe more proximal levels of duplication. Roman numerals are assigned based on how proximally the bifurcation or duplication extend. Wassel classification starts from type I with only bifid distal phalanx and goes on until type VII is a triphalangism. Type IV Wassel is described as a duplication of the proximal phalanx [3].
Excising the hypoplastic finger while reconstructing the retained one has been the approach most widely used by surgeons. The aim is to ensure that the joint and physeal plate are longitudinally oriented within the pollux axis, achieving articular stability with good range of motion and avoiding nail malalignment, which should result in a well-proportioned thumb size and volume. Specifically, in cases of preaxial thumb polydactyly, the objective is to achieve a well-aligned and stable thumb. The more-radial extra digit is usually the one being excised as it is more likely to be underdeveloped [4]
Tourniquets are commonly used in surgery to create a bloodless field, to engorge vessels for venipuncture, and in rare instances to control bleeding in life- or limb-threatening situations. In performing general orthopedic surgical procedures like polydactyly reconstruction, pneumatic tourniquets are commonly used to reduce the amount of blood within the surgical field, which enhances the visibility of anatomical features and aids in a thorough dissection, especially when closely approaching the neurovascular bundle and tendon. Lowest occlusive pressures are often measured manually by inflating the tourniquet and noting the pressure at which the distal arterial pulse stops, which is typically confirmed by a Doppler stethoscope. To account for changing conditions during surgery, a safety margin of 50–100 mmHg is added [5].
Tourniquet-related injuries are gaining more attention as a serious complication in contrast to their benefits. Blisters, abrasions, and lacerations are all examples of superficial injuries, and more serious injuries include neurovascular trauma, compartment syndrome, and muscular contusions [7]. Here, we reported the case of a 13-year-old Asian boy who underwent polydactyly reconstruction surgery in which the use of a pneumatic tourniquet had iatrogenically caused nerve injury.
Case Report
A 13-year-old Asian boy with congenital abnormality of the right thumb came to our Orthopedic and Traumatology clinic and was diagnosed with preaxial polydactyly Wassel type IV of the right hand (Figure 1). He denied any weakness, pain, or numbness in his right hand. There was no history of trauma or other congenital abnormalities. His vital sign was normal, and general and neurological examination found no abnormalities. He has not received any therapy or surgery before.
The polydactyly reconstruction was performed on November 28, 2022. We began the procedure by applying a manual pneumatic tourniquet at the level of the mid-upper arm and inflated it to 200 mmHg, which was maintained for 90 min. We performed radial side thumb excision followed by attachment of each extensor and flexor tendon to the ulnar thumb (Figure 2). We also reconstructed the radial collateral ligament and performed the first metacarpal osteotomy, then fixated it with 1.6-mm crossed Kirschner wire (Figure 3). The cuff was deflated just before completion of the surgery.
Immediately after surgery, the patient indicated he had complete weakness of his right elbow, wrist,and fingers. He also reported moderate-intensity numbness, tingling, and burning sensation along the right upper arm all the way to his fingertips. After an overnight stay at the hospital, the patient was discharged the next day with physical and radiograph status as shown in Figure 3. The patient was sent home with oral medications of cefixime 200 mg/12 h, calcium lactate 500 m/24 h, calcitriol 0.5 mcg/24 h, mecobalamin 500 mcg/24 h, methylprednisolone 4 mg/12 h, and paracetamol 500 mg/12 h.
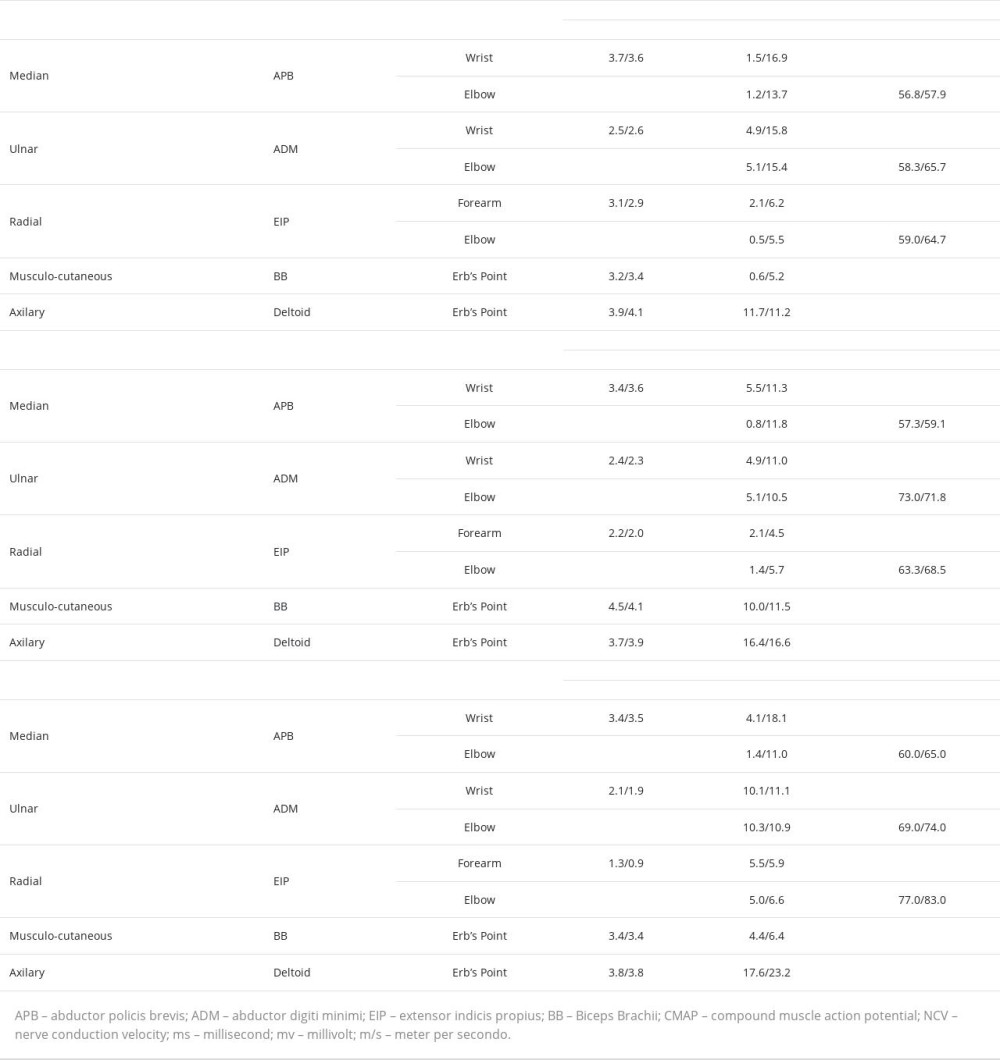
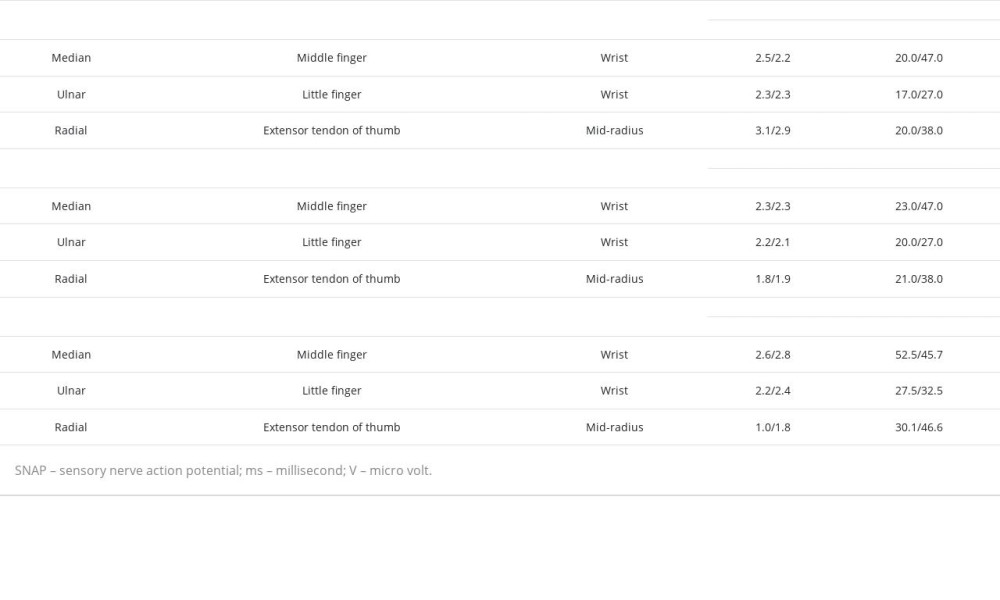
During his first follow-up 4 days after discharge, the patient reported improved pain in his right arm but the weakness persisted. The tingling sensation had also subsided but the numbness persisted. He was sent to the Neurology Department for further management. His vital signs and general examination were normal. Neurological examination showed total weakness in his right elbow, wrist, and hand (Table 1) with decreased deep-tendon reflexes. Sensory examination revealed reduced fine-tactile and pain sensitivity along his right mid-upper arm and all his fingers. Nerve conduction study (NCS) conducted 2 weeks after the surgery revealed decreased amplitude of compound-muscle action potential (CMAP) and sensory-nerve action potential (SNAP) of the right median, ulnar, radial, and musculocutaneous nerve, with normal conduction velocity and distal latency (Tables 2, 3). The neurological examination and NCS suggested axonotmesis lesions in the right median, ulnar, radial, and musculocutaneous nerves.
The patient was treated pharmacologically with mecobalamin 500 mcg and gabapentin 200 mg twice daily simultaneously with the physical rehabilitation program. He underwent a physical rehabilitation program consisting of neuromuscular electrical stimulation twice a week combined with range of motion (ROM) and hand function exercise twice a month (Figure 4). Each therapy session lasted for an hour, along with a training session for the patient to re-enact the movements independently at home.
At-home movements exercises included passive full-range ROM exercise of the affected joints, repeated 10 times for 1 set twice daily. Once the patient achieved strength against gravity, the physical therapy regimen was escalated by the occupational therapist, adding several subtasks of finer hand functioning (reaching, grasping, pinching, and manipulating small objects) to improve performance during activities of daily living (ADL). The patient and caregiver were coached to properly position the affected limb during ADL to avoid secondary injury from overstretching the weakened muscles and to prevent development of joint stiffness.
Three months after implementing this combination therapy, we evaluated the patient’s sensory problems, motoric function, and NCS study. He no longer had the tingling sensation and numbness in previously affected areas. Neurological examination showed improvement in motoric function (Table 1). On NCS evaluation, there was no significant improvement in CMAP amplitude of the previously affected nerve except the right musculocutaneous nerve (Table 2). Sensory nerve conduction study showed no significant improvement either (Table 3).
After a total of 6 months of follow-up, the patient’s overall functional recovery was very satisfying. The motoric function of the affected arm was completely restored (Table 1). NCS evaluation study showed CMAP amplitude improvement of the right ulnar and radial nerve but no significant improvement in the right median nerve (Table 2), while the SNAP amplitude of all previously affected nerves was significantly improved (Table 3).
Discussion
We present a case of nerve injury that was iatrogenically caused by 200 mmHg tourniquet utilization for 90 min in polydactyly reconstruction surgery. This 13-year-old patient had a very satisfying outcome after a combination of pharmacological and physical rehabilitation therapy for 6 months.
In radial polydactyly, we used the most commonly utilized classification by Wassel [2,3]. Out of the 6, Wassel type IV is the most frequent and was the type that our patient presented with. Surgical treatment for this congenital abnormality is intended to restore both the thumb’s appearance and function. Ablation of the radial thumb is a common choice. The existence of the crucial ulnar collateral ligaments makes it preferable to keep the ulnar thumb’s bony skeleton in place. To centralize and balance the tendons, osteotomy of the affected bone is required for alignment [4].
During limb surgeries, a tourniquet is used to generate a bloodless field, allowing for a more thorough surgical dissection. However, its use is not without complications, which range from injury to the skin, neurovascular and muscle damage, extend to reperfusion injury, rhabdomyolysis, nerve injury, and systemic consequences. Tourniquet compression nerve injuries are often temporary and manifest as mild-to-moderate symptoms. In the long term, the effects of TRNIs are detrimental, with the most dreaded outcome being nerve injury extending to paralysis [6].
Middleton and Varian reported that the incidence of tourniquet-related in Australia during the 1970s was roughly 1 in 5000 upper-limb applications [9]. Various complications still arise from application of pneumatic surgical tourniquet, even after proper inflation pressures and timings have been controlled. However, under normal circumstances and when a pneumatic tourniquet has been utilized according to conventional recommendations, the risk of significant neurological sequelae is extremely low, with a total incidence of 0.032% [7].
Odinsson and Finsen (2006) reported a couple of methods commonly used by surgeons to determine the tourniquet pressure during surgery. Surgeons can apply a fixed tourniquet pressure, usually at 250 mmHg around the upper arm and 300 mmHg around the thigh, with clinical considerations suggesting using lower pressure in pediatric patients. Surgeons also can apply a tourniquet at 100 mmHg higher than the patient’s systolic blood pressure [10].
A case series from Norway reported 15 neurological complications (3 in the upper limb and 12 in the lower limb) due to tourniquet use during surgery. All but 2 were resolved within 6 months, possibly due to tourniquet application for around 3 h [10]. Another study reported 203 cases of TRNI, 64 to the upper extremity and the rest to the lower. Although there is a wide range of tourniquet application durations in which TRNIs seem to occur, all cases had cuff times longer than 60 min. Almost all patients achieved partial to full recovery within 6 days up to 18 months after surgery, but 2% of these patients never recovered [6]. The association between tourniquet use duration and the occurrence of nerve injury was further studied by Horlocker et al (2006), who found a doubled risk of nerve injuries for every half-hour extension of tourniquet inflation [11].
Reflecting back to our case, we applied 200 mmHg of tourniquet pressure for no more than 90 min. We released the tourniquet after radial collateral ligament reconstruction was performed, as it was the last main procedure prior to soft-tissue closure with suturing. Although time and pressure parameters used during our surgery were controlled under the “limit”, TRNI complication still occurred in our case. Controlling intraoperative parameters when using tourniquets can supplement preventive measures of checking pressure gauges pre-operatively, ensuring the desired pressure is correctly achieved to reduce the incidence of TRNI [13].
The pathophysiology of nerve damage on TRNI involves both compression and ischemia. Compression of the nerve, mechanically congesting microvascular structures, and inadequate tissue perfusion eventually lead to axonal degeneration, more frequently resulting in a brief functional loss without eliminating the possibility of irreparable damage and paralysis [4]. Mechanical pressure seems to be more pivotal than distal ischemia in the pathophysiology of nerve damage [6]. The effect of different mechanism seems to be dependent on the duration of tourniquet use. For times of up to 3 h, mechanical compression dominates in causing peripheral neuropathies. Beyond that, the lack of blood flow can induce lasting structural abnormalities with extended injuries to muscle tissues [12]. Nerve injuries are more prevalent in the upper than in the lower extremity, with the radial nerve being the most susceptible [6].
Three categories of nerve injuries were described by Sir Herbert Seddon: neurapraxia, axonotmesis, and neurotmesis. Neurapraxia occurs more commonly in response to blunt trauma, followed by a temporary nerve conduction block and demyelination. As the mildest form of nerve injury, neuropraxia spontaneous healing may be as short as a couple of days ranging up to 12 weeks. Coming in as the second-degree nerve lesion, axonotmesis results in the loss of axons while preserving the connective tissue layers. Depending on the distance between the lesion and the target tissue, incomplete recovery is commonly encountered, with a rate of spontaneous regeneration of 0–3 mm per day [14,15]. Lastly, neurotmesis, as the third-degree and most severe nerve injury, will have the nerve physically separated. No electrophysiological activity or recovery should be anticipated unless surgical treatment is undertaken [14].
After a diagnosis is made and other probable causes have been ruled out, there is still no consensus on how to treat TRNI. A new approach for handling TRNI was proposed by Chang et al (2022) in the absence of such recommendations [6]. The literature emphasizes that follow-up examinations are needed until 4 weeks after surgery. Electrodiagnostic studies should be utilized, especially when there is no functional recovery, including NCS and electromyography (EMG), which may show fibrillation as a sign of denervation or fasciculation as a sign of recovery. These electrodiagnostic studies should be repeated 3–6 months after the injury. When there are no or partial improvements, surgical exploration is indicated [6,10]. Magnetic resonance neurography (MRN) has been increasingly utilized in clinical settings due to its ability to visualize complex nerve structures along their entire pathway and to distinguish nerves from surrounding vasculature and tissue in a noninvasive manner [16].
Generally, the management of peripheral nerve injury may include pharmacological therapy, physical rehabilitation, surgery, and cell-based therapies with or without tube guide biomaterial adjunct [17]. In our case, we combined administration of oral pharmacotherapy of mecobalamin 500 mcg every 12 h along with physiotherapy regimen of NMES wrist extensor and finger flexor twice a week. We also encouraged ROM exercise, ADL exercise, and hand function exercise twice monthly. The overall result was very satisfying, as the sensory and motoric function of the lower arm was almost fully restored after 6 months of combined therapy.
Recent literature demonstrates evidence of vitamin B12 (cobalamin) acting as a nerve-regeneration therapy. Cobalamin promotes myelin formation, resulting in nerve cell survival and remyelination as well as downregulating the Wallerian degeneration to allow for complete healing [18]. An exercise-based rehabilitative approach improves axonal growth and peripheral nerve architecture. Through this, growth factors increase to stimulate peripheral nerve regeneration and improve synaptic elimination while neuropathic pain is relieved through endogenous opioids release. Surgery may be an alternative management option if there is no significant clinical improvement after 3 months of follow-up. When choosing the right approach, the anatomical location of the TRNI and the goals of reconstruction should be considered. For instance, the surgeon may think about trying neurolysis, distal nerve decompression, or even nerve transfers in patients of TRNI without recovery if conservative surgical procedures are unsuccessful [6].
We realized several limitations of our report. Due to limitations in our healthcare facility, we did not perform EMG or structural imaging like MRN. Those 2 modalities can assist in more precise diagnosis and treatment. By reporting this rare case, we wish to raise surgeons’ awareness of the risk of TRNI even when tourniquets are applied at pressures and for lengths of time that are generally considered to be safe. In addition, we also encourage further studies on the best practice for the use of tourniquets during surgical procedures and management of TRNI if it occurs.
Conclusions
Nerve injury should be kept in mind as a possible complication of routine tourniquet use in many orthopedic surgeries. The possible risks from tourniquet use as a part of the overall procedure should be clearly and thoroughly explained to patients when gaining informed consent. When TRNI does occur as a postoperative complication, collaborative work between orthopedic, neurology, and physical rehabilitation departments is required to achieve good recovery. The improvement of clinical conditions in our TRNI patients may be significantly impacted by a combination of young age at onset, short duration of tourniquet use, early identification, pharmacotherapeutic care, and medical rehabilitation program. Our cases may expand the need for further studies to establish a guideline for tourniquet use and TRNI management.
Figures
References:
1.. Comer GC, Potter M, Ladd AL, Polydactyly of the hand.: J Am Acad Orthop Surg, 2018; 26(3); 75-82
2.. Wassel HD, The result of surgery for polydactyly of the thumb: A review: Clin Orthop, 1969; 64; 175-93
3.. Manske MC, Kennedy CD, Huang JI, Classifications in brief: The Wassel classification for radial polydactyly: Clin Orthop Relat Res, 2017; 475(6); 1740-46
4.. Kayalar M, Surgical reconstruction in Wassel type IV thumb duplication: Acta Orthop Traumatol Turc, 2014; 48(2); 181-86
5.. Oragui E, Parsons A, White T, Tourniquet use in upper limb surgery: Hand (New York, N,Y), 2011; 6(2); 165-73
6.. Chang J, Bhandari L, Messana J, Management of tourniquet-related nerve injury (TRNI): A systematic review: Cureus, 2022; 14(8); e27685
7.. Mingo-Robinet J, Castañeda-Cabrero C, Alvarez V, Tourniquet-related iatrogenic femoral nerve palsy after knee surgery: Case report and review of the literature: Case Rep Orthop, 2013; 2013; 368290
8.. Choong PFM, Tourniquet injuries: An overinflated problem?: ANZ J Surg, 2004; 74(9); 717
9.. Middleton KWD, Varian JP, Tourniquet paralysis: ANZ J Surg, 1974; 44(2); 124-28
10.. Odinsson A, Finsen V, Tourniquet use and its complications in Norway.: J Bone Joint Surg Br., 2006; 88-B(8); 1090-92
11.. Horlocker TT, Hebl JR, Gali B, Anesthetic, patient, and surgical risk factors for neurologic complications after prolonged total tourniquet time during total knee arthroplasty: Anesth Analg, 2006; 102(3); 950-55
12.. Masri BA, Eisen A, Duncan CP, McEwen JA, Tourniquet-induced nerve compression injuries are caused by high pressure levels and gradients – a review of the evidence to guide safe surgical, pre-hospital and blood flow restriction usage: BMC Biomed Eng, 2020; 2(1); 7
13.. Arumugam M, Prevention of tourniquet paralysis during the use of Pneumatic tourniquets: Int J Orthop Trauma Nurs, 2011; 15(2); 57-61
14.. Chhabra A, Ahlawat S, Belzberg A, Andreseik G, Peripheral nerve injury grading simplified on MR neurography: As referenced to Seddon and Sunderland classifications: Indian J Radiol Imaging, 2014; 24(03); 217-24
15.. Grinsell D, Keating CP, Peripheral nerve reconstruction after injury: A review of clinical and experimental therapies: Biomed Res Int, 2014; 2014; 698256
16.. Ku V, Cox C, Mikeska A, MacKay B, Magnetic resonance neurography for evaluation of peripheral nerves: J Brachial Plex Peripher Nerve Inj, 2021; 16(01); e17-e23
17.. Lopes B, Sousa P, Alvites R, Peripheral nerve injury treatments and advances: One health perspective: Int J Mol Sci, 2022; 23(2); 918
18.. Baltrusch S, The role of neurotropic B vitamins in nerve regeneration: Biomed Res Int, 2021; 2021; 9968228
Figures
In Press
28 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942881
28 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943590
29 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943843
30 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943577
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250