13 November 2023: Articles 
Successful Total Knee Arthroplasty for Hoffa and Proximal Tibial Fractures: Report of Three Complex Cases After Failed Osteosynthesis Procedures
Rare disease
Takuma Maeda1A, Tomoyuki Matsumoto1A*, Masahiro Fujita1A, Masanori Tsubosaka1A, Tomoyuki Kamenaga1A, Naoki Nakano1A, Yuichi Kuroda1A, Shinya Hayashi1A, Takahiro Niikura1A, Ryosuke Kuroda1ADOI: 10.12659/AJCR.941187
Am J Case Rep 2023; 24:e941187
Abstract
BACKGROUND: Distal femoral and proximal tibial fractures often lead to nonunion and post-traumatic osteoarthritis, and total knee arthroplasty (TKA) has emerged as an effective alternative for older patients. This report includes 3 cases of successful TKA treatment. The cases involve a 42-year-old man and a 62-year-old man with Hoffa coronal fractures of the distal femur, and a 50-year-old man with a proximal tibial fracture. These patients underwent multiple osteosynthesis procedures before receiving TKA.
CASE REPORT: Case 1: A 42-year-old man with a displaced Hoffa's fracture had persistent knee pain. Nonunion post-initial fixation led to reoperation with iliac bone grafting and plate fixation. TKA using a Posterior Stabilized (PS)-type implant resulted in improved motion and function after 3 years. Case 2: A 62-year-old man suffered lateral condyle and ligament injuries from a displaced Hoffa's fracture. Despite plate fixation, dislocation occurred, requiring conversion. TKA with long-stem hinge-type implant, using augmentation block, led to enhanced stability and outcomes at 2 years. Case 3: A 50-year-old man's tibial nonunion, treated with plate fixation, resulted in infection and bone fusion. TKA using a constrained PS-type implant insert addressed the lateral tibial adhesions via iliotibial band (ITB) release and treated severe tibial plateau damage. Positive results were seen at 1 year.
CONCLUSIONS: The challenges of pseudarthrosis, like bone defects and compromised tissue, highlight the need for precise implant selection based on evaluations of bone quality, defects, knee stability, and hyperextension, rather than resorting to overly-constrained implants.
Keywords: Arthroplasty, Replacement, Knee, Femoral Fractures, Tibial Fractures
Background
Distal femoral and proximal tibial fractures are common in orthopedics, and nonunion, a major complication following surgical fixation, greatly reduces patient satisfaction due to exacerbation of pain and disability, prolonged rehabilitation, and the requirement for secondary surgical treatment [1,2]. Hoffa’s fracture, involving a coronal plane fracture of the distal femoral condyle, is relatively rare in orthopedic injuries [3]. This fracture type presents unique challenges due to its distinct location and configuration, often defying successful conservative treatment. Its rarity is attributed to the specific forces required for its occurrence, complicating diagnosis and management [4]. Previous studies have reported a relatively high risk of postoperative complications, such as implant failure and nonunion, following the osteosynthesis [3]. Several authors have suggested that TKA can be an effective treatment option for cases of nonunion after Hoffa’s fractures [5,6]. Likewise, proximal tibial fractures have a relatively high rate of nonunion, even with internal fixation [7]. This is mainly due to the deforming forces in the proximal aspect of the tibia and limited soft tissue coverage [8]. Harold et al suggested that TKA was an appropriate treatment for nonunion following proximal tibial fractures [5].
TKA is a common surgical treatment with good long-term results for severe osteoarthritis (OA) of the knee joints that helps reduce pain and recover functional capacity. Distal femoral and proximal tibial fractures tend to be a factor in nonunion and result in post-traumatic OA (PTOA), and TKA can be an effective treatment for such patients [6,9].
While several authors reported TKAs after osteosynthesis of distal femur and proximal tibial fractures [5,10,11], reports of Hoffa fractures leading to TKA are rare [12,13]. However, to the best of our knowledge, there are no reports of TKA as a salvage treatment after re-osteosynthesis of pseudarthrosis following primary internal fixation. This report is of 2 cases of Hoffa coronal fracture of the distal femur in a 42-year-old man and a 62-year-old man, and 1 case of proximal tibial fracture in a 50-year-old man, all successfully treated with TKA after multiple previous osteosynthesis procedures.
Case Reports
CASE 1:
A 42-year-old man presented in 2018 with a complaint of pain in the left knee with a 0–95° range of motion and no instability. In 2016, the patient had a road traffic accident and experienced a fracture of the left patella and an ipsilateral displaced Hoffa’s fracture of the medial femoral condyle (AO: 33-B3.1). Initially, a partially threaded cannulated screw fixation of the condylar fracture was performed. One year after the initial surgery in 2016, radiographic examination showed a nonunion of the femoral condyle, and reoperation using screw extraction, iliac bone grafting, and plate fixation were performed. The pain in the left knee joint persisted, and in 2018, PS-type TKA (Persona, Zimmer Biomet) was performed. The procedure was conducted using a medial parapatellar approach. Bone resection was performed utilizing an intramedullary rod. Notably, there was severe internal joint deterioration. The femoral posterior condyle exhibited significant osteophyte formation, necessitating detachment of the joint capsule, but no specific additional techniques were required. At the final follow-up in 2021, the patient had a painless mobile joint with 125° range of motion. The 2011 Knee Society Score (KSS) improved from a preoperative score of 96 to 211, and his functional activities improved from 28 to 83 one year later (Figure 1, Table 1).
CASE 2:
A 62-year-old man presented in 2016 with a complaint of pain and giving way of his left knee at a 0–85° range of motion, with medial instability and severe lateral instability. In 2015, the patient experienced a left femoral-displaced Hoffa’s fracture of the lateral femoral condyle (AO: 33-B3.1) and an avulsion fracture of the medial collateral ligament (MCL). Initially, plate fixation of the lateral condyle and screw fixation of avulsion fractures were performed. Two months later, after the initial surgery in 2015, radiographic examination revealed dislocation, and plate conversion was performed. The knee joint pain in maximum flexion and giving way persisted, and in 2016, TKA was performed. During the procedure, due to challenging subcutaneous dissection caused by adhesions, a quadriceps snip was utilized to facilitate access. A medial parapatellar approach was utilized. Bone resection was performed utilizing an intramedullary rod. Additionally, a bone defect occurred in the lateral femoral condyle, necessitating the use of an augment block. Given the non-functioning state of the MCL, a planned long-stem hinge-type TKA (RHK, Zimmer Biomet) was chosen to enhance implant stability. Final follow-up at 2 years after TKA, in 2018, revealed a painless mobile joint with a 100° range of motion. KSS improved from a preoperative score of 64 to 201, and his functional activities improved from 26 to 80 one year later (Figure 2, Table 1).
CASE 3:
A 50-year-old man presented in 2020 with a complaint of pain of the right knee with −5° to 80° range of motion and no instability. Six years prior, in 2014, the patient fell from a motorcycle and experienced a right proximal tibial fracture (AO: 41-C3). Initially, plate fixation was performed and subsequently became an infected nonunion. After 2 surgeries on the infected nonunion, in 2014 and in 2015, bone fusion was achieved, leading to the removal of all implants in 2017. Three years later, in 2020, the patient’s pain in the knee joint persisted, and TKA was performed. A medial parapatellar approach was utilized. Due to significant adhesions on the lateral aspect of the tibia, an increased detachment of the ITB insertion was required to facilitate patellar eversion. Bone resection was conducted using an intramedullary rod. Notably, the tibial plateau exhibited severe bone loss and cartilage damage; however, bone integrity was maintained. In line with our preoperative plan, the stemmed tibial component was not utilized, and instead, a constrained PS insert (Persona, Zimmer Biomet) was utilized. At a 1-year final follow-up, in 2021, the patient had a painless mobile joint with 100° range of motion. KSS improved from a preoperative score of 117 to 198, and his functional activities improved from 29 to 81 one year later (Figure 3, Table 1)..
Discussion
The most important finding of this study is that TKA can be an effective treatment for refractory nonunion that cannot be achieved by repeated revision osteosynthesis. Distal femoral fractures in the coronal plane, known as Hoffa’s fractures, are rare and associated with a relatively high risk of postoperative complications, such as implant failure and pseudoarthrosis, after osteosynthesis [3]. For adequate stability and early active rehabilitation, cannulated or lagged screws combined with a locking plate are recommended [14]. In Case 1, the initial osteosynthesis was only screw fixation; therefore, there is a possibility that the fixation was poor and resulted in non-union. In Case 2, although a combination of cannulated screw and plate fixation was used in the first osteosynthesis, it was dislocated. The treatment for ligament damage may have been inadequate because mediolateral instability remained at the time of presentation.
When dealing with patients who are physiologically younger, with preserved articular cartilage and enough distal bone for fixation, revision osteosynthesis is the recommended treatment option [15]. However, for elderly patients who have severe osteopenia, multiple unsuccessful attempts at internal fixation, insufficient remaining distal bone stock, and/or significant degenerative changes in the knee, knee arthroplasty is a desirable treatment option [16]. Moreover, TKA is an effective treatment for nonunion Hoffa’s fracture after osteosynthesis. Our results are consistent with those of previous studies, indicating the high effectiveness of TKA in obtaining good results [12,13].
Fracture-related infection (FRI) is another complication that adversely affects bone healing and increases the risk of pseudarthrosis [17]. In Case 3, instability of the fracture site might have prevented bone union and caused infection, the so-called infected pseudarthrosis. Metsemakers et al reported that in the treatment of FRI, the presence of implants increased the risk of infection; however, residual instability of the fracture site outweighed this risk [18]. In this case, we waited for the fracture site to stabilize through bone healing before removing the implant, which allowed us to suppress FRI and select TKA, resulting in a good outcome.
There can be various surgical challenges and complexities when performing a secondary TKA for pseudoarthrosis after knee fracture, malunions, bone defects, prior internal fixation devices, latent infections, arthrofibrosis, and compromised soft-tissue envelope. Typically, the use of bone grafts or revision implants is needed to address these issues [19,20]. It has been less successful than primary TKA for primary knee OA in terms of postoperative outcomes and complications, reoperation, and survival rates [6, 21].
In Case 1, we performed PS-type TKA with good outcomes because there was no instability of the knee joint and bone defects, and the medial release of the knee joint could be limited to the deep MCL. In Case 2, we used a hinge-type implant with an augmentation block because of the medial and lateral instabilities of the knee joint and bone loss in the posterolateral part of the distal femur. However, the outcome was relatively good. In Case 3, we had to pay attention to the risk of bone fragility due to osteosynthesis and infection and prepare a long-stem tibial component. However, intraoperative findings showed that the bone quality was relatively good, and we selected a normal implant with CPS insert without a long-stem tibial component, resulting in a good outcome. Patients with instability may require constrained implants, such as hinge-type, PCCK-type, and stem-supported implants, due to poor bone quality [22]. However, these implants have a higher risk of infection and loosening; thus, it is preferable to select appropriate implants based on preoperative and intraoperative evaluations according to the patient’s bone quality, bone defects, knee instability, and presence or absence of hyperextension, rather than using unnecessarily highly constrained implants [23]. Reddy et al successfully executed unconstrained TKA on 2 patients who had bilateral Hoffa fractures following bone grafting [12]. Conversely, Mortazavi et al utilized a constrained TKA for a case involving a lateral Hoffa fracture [13]. All interventions led to positive clinical outcomes. These studies underscore the importance of evaluating distinct patient parameters such as age, activity level, and bone stock prior to determining the appropriate surgical intervention, a viewpoint we strongly concur with. Although knee fractures around the joint have a high risk of nonunion, which can contribute to poor postoperative outcomes, we propose that TKA can be an effective salvage surgery option.
Conclusions
Pseudarthrosis challenges stress the importance of choosing the right implant. It is crucial to assess the patient’s bone stock, knee stability, and other factors instead of just picking restrictive implants. Our cases show how TKA can be a good solution in these difficult situations.
Figures
References:
1.. Koso RE, Terhoeve C, Steen RG, Zura R, Healing, nonunion, and re-operation after internal fixation of diaphyseal and distal femoral fractures: A systematic review and meta-analysis: Int Orthop, 2018; 42(11); 2675-83
2.. Bonafede M, Espindle D, Bower AG, The direct and indirect costs of long bone fractures in a working age US population: J Med Econ, 2013; 16(1); 169-78
3.. Kurahatti A, Seenappa H, Shanthappa AH, Nagakumar JS, The functional and radiological outcome of Hoffa’s fracture treated with cannulated cancellous screws: Cureus, 2022; 14(4); e23829
4.. Patel PB, Tejwani NC, The Hoffa fracture: Coronal fracture of the femoral condyle a review of literature: J Orthop, 2018; 15(2); 726-31
5.. Bielke HD, Alamino LP, Aguer S, Total knee arthroplasty in patients with joint fracture sequela: Mid-term follow-up outcome: Rev Asoc Argent Orthop Traumatol, 2020; 85(2); 107-18
6.. Saleh H, Yu S, Vigdorchik J, Schwarzkopf R, Total knee arthroplasty for treatment of post- traumatic arthritis: Systematic review: World J Orthop, 2016; 7(9); 584-91
7.. Thompson JH, Koutsogiannis P, Jahangir A, Tibia fractures overview. [Updated 2023 Jul 31]: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing Available from: https://www.ncbi.nlm.nih.gov/books/NBK513267/
8.. Obana KK, Lee G, Lee LSK, Characteristics, treatments, and outcomes of tibial plateau nonunions: A systematic review: J Clin Orthop Trauma, 2021; 16; 143-48
9.. Putman S, Argenson JN, Bonnevialle P, Ten-year survival and complications of total knee arthroplasty for osteoarthritis secondary to trauma or surgery: A French multicentre study of 263 patients: Orthop Traumatol Surg Res, 2018; 104; 161-64
10.. Vestergaard V, Pedersen AB, Hare KB, Knee fracture Increases TKA risk after initial fracture treatment and throughout life: Clin Orthop Relat Res, 2020; 478(9); 2036-44
11.. Dombrowski ME, O’Malley MJ, Indications for distal femoral replacement arthroplasty in acute geriatric distal femoral fractures: Oper Tech Orthop, 2018; 28(3); 125-33
12.. Reddy VG, Mootha AK, Chiranjeevi T, Kantesaria P, Total knee arthroplasty as salvage for non union in bicondylar hoffa fracture: A report of two cases: J Orthop Case Rep, 2011; 1(1); 26-28
13.. Mortazavi SMJ, Khan FMY, Ramezanpour A, Firoozabadi MJD, Post-traumatic total knee arthroplasty: A case of Hoffa fracture non-union and review of literature: J Orthopedic and Spine Trauma, 2018; 4(3); 59-61
14.. Gao M, Tao J, Zhou Z, Surgical treatment and rehabilitation of medial Hoffa fracture fixed by locking plate and additional screws: A retrospective cohort study: Int J Surg, 2015; 19; 95-102
15.. Haidukewych GJ, Berry DJ, Jacofsky DJ, Torchia ME, Treatment of supracondylar femur nonunions with open reduction and internal fixation: Am J Orthop, 2003; 32(11); 564
16.. Haidukewych GJ, Springer BD, Jacofsky DJ, Berry DJ, Total knee arthroplasty for salvage of failed internal fixation or nonunion of the distal femur: J Arthroplasty, 2005; 20(3); 344-49
17.. Moriarty TF, Metsemakers WJ, Morgenstern M, Fracture-related infection: Nat Rev Dis Primers, 2022; 8(1); 67
18.. Metsemakers WJ, Kuehl R, Moriarty TF, Infection after fracture fixation: Current surgical and microbiological concepts: Injury, 2018; 49(3); 511-22
19.. El-Galaly A, Haldrup S, Pedersen AB, Increased risk of early and medium-term revision after post-fracture total knee arthroplasty. Results from the Danish Knee Arthroplasty Register: Acta Orthop, 2017; 88(3); 263-68
20.. Elsoe R, Johansen MB, Larsen P, Tibial plateau fractures are associated with a long-lasting increased risk of total knee arthroplasty a matched cohort study of 7,950 tibial plateau fractures: Osteoarthr Cartil, 2019; 27(5); 805-9
21.. Lunebourg A, Parratte A, Gay A, Lower function, quality of life, and survival rate after total knee arthroplasty for posttraumatic arthritis than for primary arthritis: Acta Orthop, 2015; 86(2); 189-94
22.. Parratte S, Ollivier M, Argenson JN, Primary total knee arthroplasty for acute fracture around the knee: Orthop Traumatol Surg Res, 2018; 104(1S); S71-80
23.. Costa GG, Presti ML, Agrò G, Difficult primary total knee arthroplasty requiring a varus-valgus constrained implant is at higher risk of periprosthetic infection: Knee Surg Sports Traumatol Arthrosc, 2020; 28(12); 3787-95
Figures
Tables
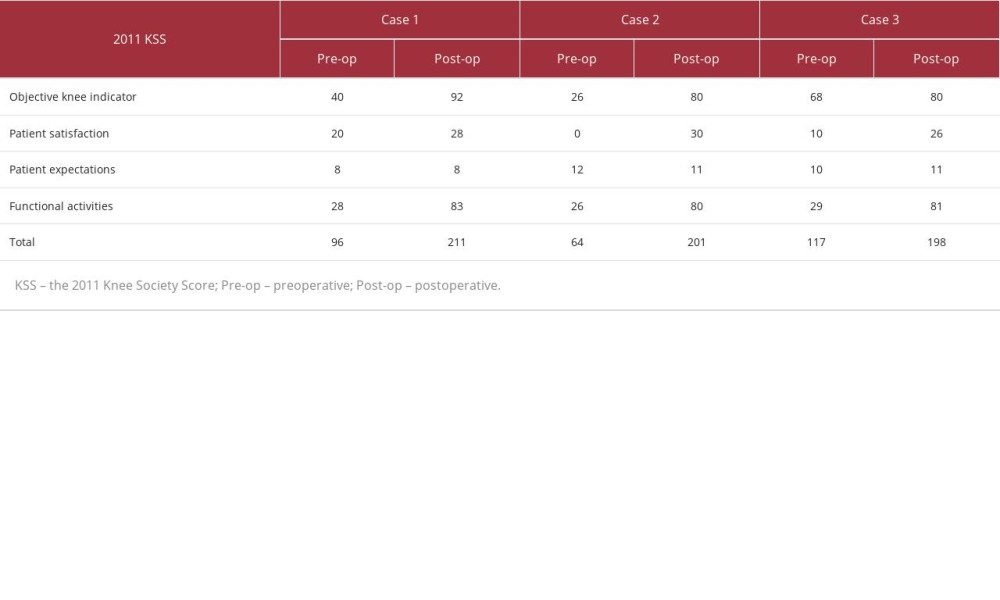 Table 1.. Pre- and post-surgery knee scores: three cases.This table shows the preoperative and postoperative 2011 Knee Society Scores for 3 cases, arranged in the order of objective knee indicator, patient satisfaction, patient expectations, functional activities, and total.
Table 1.. Pre- and post-surgery knee scores: three cases.This table shows the preoperative and postoperative 2011 Knee Society Scores for 3 cases, arranged in the order of objective knee indicator, patient satisfaction, patient expectations, functional activities, and total.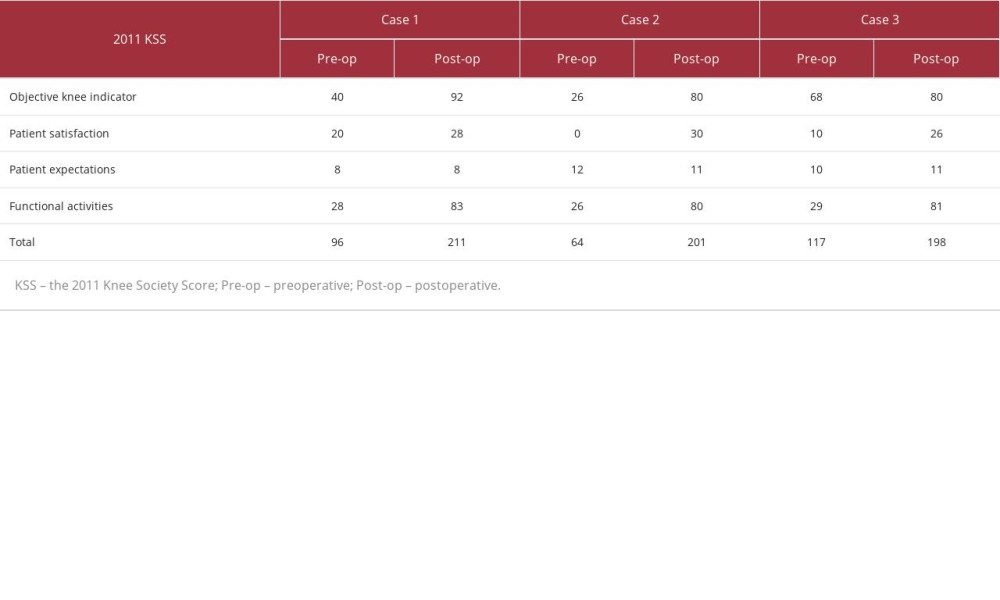 Table 1.. Pre- and post-surgery knee scores: three cases.This table shows the preoperative and postoperative 2011 Knee Society Scores for 3 cases, arranged in the order of objective knee indicator, patient satisfaction, patient expectations, functional activities, and total.
Table 1.. Pre- and post-surgery knee scores: three cases.This table shows the preoperative and postoperative 2011 Knee Society Scores for 3 cases, arranged in the order of objective knee indicator, patient satisfaction, patient expectations, functional activities, and total. In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943174
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943136
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








