18 January 2024: Articles 
A 25-Year-Old Military Recruit with Isolated Myositis Following Routine Chemoprophylaxis with Intramuscular Benzathine Penicillin G
Adverse events of drug therapy, Rare coexistence of disease or pathology
Ji-Min Park1ABCDEF*, Matthew A. Soderstrom1EF, Austin N. Baraki1EDOI: 10.12659/AJCR.941221
Am J Case Rep 2024; 25:e941221
Abstract
BACKGROUND: Myositis is an inflammatory myopathy that can be caused by a variety of drugs, diseases, and toxins. The U.S. military uses chemoprophylaxis with intramuscular penicillin G to prevent group A streptococcal infection. We present a case of penicillin G-induced myositis, a rare cause of drug-induced myositis with limited discussion in the medical literature.
CASE REPORT: A 25-year-old man with no pertinent medical history presented to the Emergency Department with right hip and leg pain after receiving a single dose of intramuscular penicillin G as part of standard prophylaxis for group A streptococcal infection during basic military training. He reported pain and leg weakness that was exacerbated by physical exertion and weight bearing but had no systemic symptoms, such as fevers or chills. Initial radiographs of the hip were normal; however, subsequent magnetic resonance imaging of the hip revealed intramuscular edema and features consistent with myositis of the right proximal thigh and hip musculature. He was admitted for isolated right gluteal myositis, attributed to his preceding local penicillin injection. He recovered with symptomatic care over the following 2 weeks, with return to baseline function.
CONCLUSIONS: This case highlights a rare complication of intramuscular penicillin G as a cause of acute isolated myositis. It serves to inform physicians of this rare complication and to recommend the consideration of intramuscular penicillin G as a causative etiology in individuals presenting with myositis and recent penicillin G exposure.
Keywords: Antibiotic Prophylaxis, Injection Site Reaction, myositis, Penicillin G Benzathine
Background
Myositis is an inflammatory myopathy that often leads to rhabdomyolysis owing to direct damage to muscle sarcolemma, with the consequent release of myoglobin and its toxic metabolites into the systemic circulation [1]. Drug-induced myositis is well documented in the literature, with many agents identified as potential etiologies. Myositis caused by various drugs can be difficult to identify due to similar presentations of alternative etiologies of myositis, such as autoimmune myopathies, exogenous toxins, metabolic diseases, endocrinopathies, malignancy, and infections [2]. While numerous pharmacologic agents have been identified as offending agents in the development of myositis, penicillin G has rarely been described in the literature as a potential cause of drug-induced myositis in the adult population. Chemoprophylaxis with intramuscular benzathine penicillin G has been used widely by the U.S. military to prevent epidemics of group A streptococcal infections during basic training [3]. Patients generally tolerate benzathine penicillin well; however, notable adverse effects include injection site pain and sometimes hypersensitivity reactions [4]. This case represents a case of a young active-duty basic military training (BMT) trainee who presented with an isolated gluteal myositis after administration of intramuscular penicillin G, without other identifiable causal etiologies, highlighting penicillin G as a rare but important causative etiology of acute myositis.
Case Report
A 25-year-old healthy male military recruit with no pertinent medical history presented to the BMT clinic with right hip and leg pain that started several hours after receiving intramuscular penicillin G as part of standard BMT prophylaxis. The pain was rated 6/10 in severity, was localized over the right hip, and was worsened by exercise and weight bearing. He also reported mild right lower extremity swelling but denied systemic symptoms, such as fevers or chills. He had previously been tolerating physical activity during training and reported no history of falls, traumatic injuries, or prior surgeries of the affected limb. Physical examination at the BMT clinic revealed mild weakness of the affected limb and tenderness to palpation over the hip musculature, and no other abnormalities. Presumed overuse injury was diagnosed, and the patient was prescribed ibuprofen and methocarbamol, with instructions to maintain the non-weightbearing status of the affected limb for the remainder of the day, with a gradual return to activity as tolerated.
Over the course of the next day, he experienced worsening pain despite analgesic use, prompting presentation to the Emergency Department. He reported that he could no longer bear any weight on his right leg, and rated the pain as 8/10 in severity. The pain was characterized as constant and sharp, with associated increased swelling around the right hip. He was afebrile, with vital signs of blood pressure, 139/77 mmHg; heart rate, 100 beats per min; respiratory rate, 16 breaths per min; and SpO2, 99% on room air. A physical examination revealed significant tenderness over the posterolateral aspect of the right hip and mild edema without fluctuance or other overlying skin changes. There was no ecchymosis, deformity, or significant warmth over the affected area. Distal pulses were palpable bilaterally.
Initial laboratory studies included a complete blood count, complete metabolic panel, creatine kinase (CK), and C-reactive protein. The complete blood count revealed a mild leukocytosis, with a leukocyte count of 12.37×103/µL, but was otherwise normal. The complete metabolic panel and creatinine level were within the reference range. C-reactive protein and CK levels were elevated at 11.3 mg/dL and 971 U/L, respectively. The initial radiograph of the pelvis and bilateral hips was normal, with no fracture or dislocation. However, subsequent contrast-enhanced magnetic resonance imaging of the right hip revealed severe intramuscular edema and enhancement within the right tensor fascia lata and mild intramuscular edema within the right gluteus medius, right gluteus minimus, and right gluteus maximus, concerning for severe myositis versus myofascial soft tissue infection (Figure 1). There was no intra-articular involvement or other findings suggestive of macroscopic muscular necrosis, joint injection, or osteomyelitis.
Based on the above findings, the initial differential diagnoses included infectious myositis, necrotizing fasciitis, rhabdomyolysis, toxic or drug-induced myositis, trauma, hypersensitivity reaction, and autoimmune myositis. His lack of systemic symptoms and subsequent response to treatment were reassuring against infection. Despite a modest elevation in CK level, the patient did not present with symmetric proximal muscle weakness or other findings suggestive of inflammatory myopathies, such as dermatomyositis or polymyositis, and a lack of myoglobinuria made significant rhabdomyolysis less likely. His history and a negative urine drug screen pointed against illicit substance use to include anabolic steroids. A lack of other auto-immune phenomena and a lack of family history lowered the probability of a primary autoimmune process. The absence of subcutaneous gas, lack of infectious symptoms, and improving trends in his laboratory markers and physical examination were reassuring against necrotizing fasciitis. Lastly, lack of surrounding skin erythema or presence of an abscess suggested against skin and soft tissue infection around the injection site. Given the lack of other identifiable risk factors, and the immediately preceding history of intramuscular penicillin G into the affected area, a presumptive diagnosis of penicillin G-induced myositis was made.
The patient was admitted and treated with supportive care and pain control with non-steroidal anti-inflammatory drugs, with rapid reduction of pain over the following 2 days. He did not require antibiotic therapy or surgical intervention. His white blood cell count and CK levels normalized spontaneously. He was discharged and was able to return to full duty 2 weeks later without other issues.
Discussion
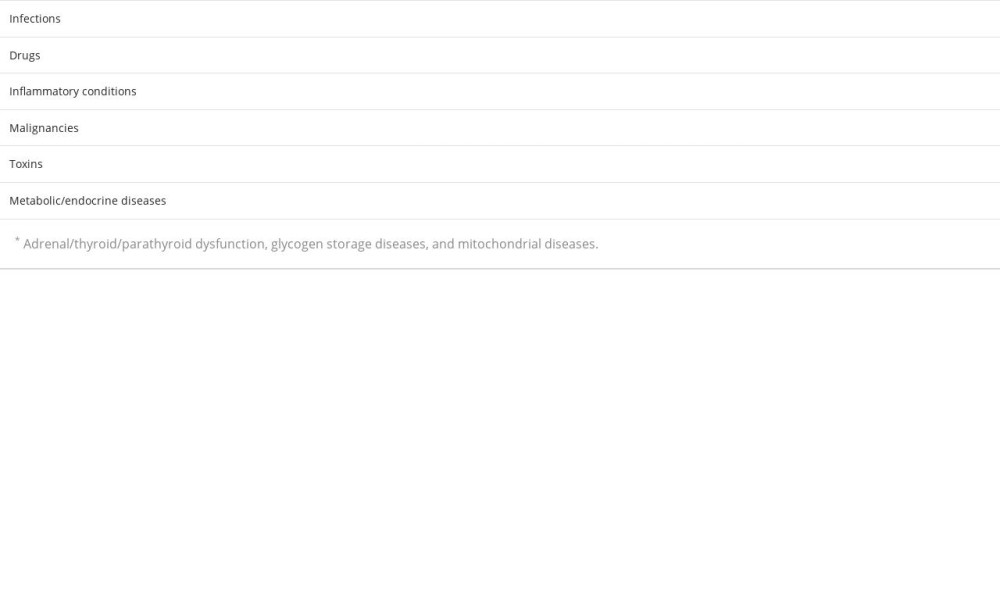
This case report serves to inform the medical community that penicillin G can precipitate an isolated myositis. Myositis has a broad array of potential causes, including infections, auto-immune diseases, drugs and toxins, malignancies, metabolic diseases, and endocrinopathies, among others (Table 1). Infectious myositis can occur secondary to bacterial, viral, and parasitic infections. Bacterial myositis is associated with
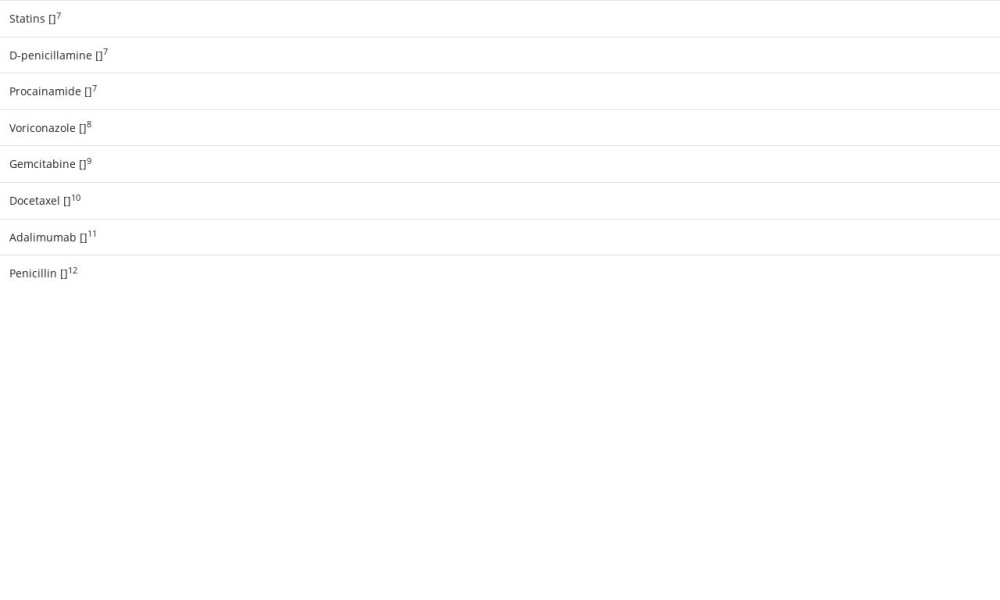
Many drugs can cause muscular adverse effects, leading to myopathies and myositis. Drug-induced myositis manifests as muscle weakness, myalgia, CK elevation, and potential progression to rhabdomyolysis [7]. While this phenomenon is well recognized with statins, fibrates, metal binders, certain anti-arrhythmics, azoles [8], anti-neoplastic agents [9,10], and tumor necrosis factor-alpha inhibitors [11], penicillin has been rarely implicated as a causal etiology of drug-induced myositis (Table 2). Diagnosis of drug-induced myositis, particularly related to intramuscular penicillin G, can be challenging in clinical settings owing to the apparent rarity of the condition and similar presentation to other etiologies of myositis. This is likely to be more challenging when a patient has multiple co-morbid conditions and other medications. When faced with a case of drug-induced myositis, we recommend removing the suspected offending agent, providing supportive care with analgesia, and using conservative management to allow recovery with follow-up to complete resolution.
In our review of the literature, a single case report was identified in which a 7-year-old boy receiving intramuscular penicillin G developed myositis while being treated for rheumatic heart disease. This case describes a boy with history of acute rheumatic fever who developed fever, left hip monoarthritis, and elevated inflammatory markers, consistent with myositis 46 days after receiving an intramuscular penicillin G injection, with no other causes [12]. Similarly, our case of a 25-year-old healthy man presenting with isolated myositis starting several hours after local injection illustrates that intramuscular penicillin G is a potential causal agent of drug-induced myositis. Despite a thorough diagnostic evaluation as mentioned above, there were no other identifiable risk factors or underlying conditions besides the history of the preceding intramuscular penicillin G into the right gluteal musculature. To the best of our knowledge, this is the first case report of penicillin G-linked myositis in the adult population. Penicillin G is a rare etiology of acute myositis that deserves the attention of clinicians when considering differential diagnoses for myositis.
Lastly, penicillin G is used as a standard prophylaxis for group A streptococcus among military trainees. We acknowledge that it is imperative to minimize the adverse effects of antibiotics to attain an optimized clinical safety [13]. However, owing to the rarity of this complication, we do not advocate a change in the current practice. Nonetheless, physicians should be educated and aware of myositis as a potential complication.
Conclusions
This case is valuable, as it illustrates a rare cause of drug-induced myositis in a basic military trainee without any other identifiable causes. Intramuscular penicillin G-induced myositis is rarely reported in the literature, and we hope to inform the medical community of this potential complication so that they can consider this diagnosis in individuals with exposure. While penicillin G-induced myositis is rare, recognizing penicillin G as an etiology of isolated myositis is important and may reduce unnecessary antibiotic exposure, costly medical evaluations, and potentially surgical intervention if necrotizing fasciitis is suspected.
References:
1.. Hamel Y, Mamoune A, Mauvais FX, Acute rhabdomyolysis and inflammation: J Inherit Metab Dis, 2015; 38(4); 621-28
2.. Zuckner J, Drug-related myopathies: Rheum Dis Clin North Am, 1994; 20(4); 1017-32
3.. Webber BJ, Kieffer JW, White BK, Chemoprophylaxis against group A streptococcus during military training: Prev Med, 2019; 118; 142-49
4.. Gartlan WA, Rahman S, Reti K, Benzathine penicillin: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing [Updated 2023 May 14]. In:
5.. Berth SH, Lloyd TE, Secondary causes of myositis: Curr Treat Options Neurol, 2020; 22(11); 38
6.. Fayyaz B, Rehman HJ, Uqdah H, Cancer-associated myositis: An elusive entity: J Community Hosp Intern Med Perspect, 2019; 9(1); 45-49
7.. Valiyil R, Christopher-Stine L, Drug-related myopathies of which the clinician should be aware: Curr Rheumatol Rep, 2010; 12(3); 213-20
8.. Shanmugam VK, Matsumoto C, Pien E, Voriconazole-associated myositis: J Clin Rheumatol, 2009; 15(7); 350-53
9.. Chun JY, Lee JM, Ahn DW, Gemcitabine-induced myositis in a diabetes mellitus patient on hemodialysis: Korean J Intern Med, 2017; 32(5); 930-32
10.. Wongsaengsak S, Quirch M, Ball S, Docetaxel-induced acute myositis: A case report with review of literature: J Chemother, 2021; 33(2); 116-21
11.. Gaboriau L, Davion JB, Combret S, Adalimumab and myositis: A case report and review of the French and international Pharmacovigilance Databases: Neuromuscul Disord, 2020; 30(11); 915-20
12.. Francis JR, Wyber R, Remenyi B, Myositis complicating benzathine penicillin-G injection in a case of rheumatic heart disease: IDCases, 2016; 4; 6-7
13.. Bolcato M, Fassina G, Rodriguez D, The contribution of legal medicine in clinical risk management: BMC Health Serv Res, 2019; 19(1); 85
In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250