29 November 2023: Articles 
A Unique Case of Perforated Appendicitis in a Giant Incarcerated Right-Sided Inguinal Hernia: Challenges and Surgical Management
Rare disease
Alexis LitchinkoDOI: 10.12659/AJCR.941649
Am J Case Rep 2023; 24:e941649
Abstract
BACKGROUND: Amyand hernia is a rare condition described as the presence of the appendix within an inguinal hernia. The clinical presentation of can be atypical, depending on the length of the defect’s history and the size of the hernia. As inguinal hernia repair is considered a routine surgical procedure, giant hernias are mostly encountered in countries with limited medical care or with patient rejection of surgical management.
CASE REPORT: We report a case of a 56-year-old patient with a history of a chronic giant inguinal-scrotal hernia for more than 10 years who presented himself to the Emergency Department with acute pain in the scrotum and fever. Computed tomography revealed a perforated appendicitis located in the inferior part of the scrotum. The patient underwent a surgical procedure with an inguinal and middle laparotomy approach, revealing a full incarceration of the right and traverse colon, terminal ileal loop, and omentum, along with evidence of a perforated appendicitis. Standard appendectomy and direct hernia repair were successfully performed.
CONCLUSIONS: To the best of our knowledge, this is the first case of a perforated appendicitis within a right giant inguinal hernia described in the modern English-language literature. Rare in our daily practice, giant hernias are a real challenge regarding their surgical management during and after surgery, making this case with a perforated appendicitis even more arduous.
Keywords: appendicitis, Hernia, Inguinal
Background
Presence of the appendix in an inguinoscrotal hernia is a specific clinical presentation that was first described by the French surgeon Claudius Amyand in 1735 [1]. This type of presentation is considered with or without an associated appendicitis. A recent review in 2014 estimated the prevalence of Amyand hernias as 0.5% among inguinal hernias and 0.1% associated with appendicitis [2,3]. Inguinoscrotal hernias are a common situation in surgeons’ daily practice, and early diagnosis and accessibility to surgery in Western countries has made giant hernias a rare condition [4,5].
Regarding giant hernias, Trakarnsagna et al [6] proposed a recent classification in 2014 regarding the level of the scrotum and proposed a specific surgical approach for each stage (Figure 1). Type 1 is characterized by a hernia located below the mid-inner thigh but above the suprapatellar lines. The recommended treatment for this type is hernioplasty, and it’s essential to monitor both intraabdominal and intrathoracic pressure during the procedure. Type 2 is characterized by a hernia situated below the suprapatellar lines but above the superior border of the patellar bone. For this type, hernioplasty combined with resection of content is suggested, along with a procedure to increase intra-abdominal volume. Type 3 involves a hernia located below the superior border of the patellar bone. The recommended approach for this type is to increase the intra-abdominal volume surgically prior to surgery. However, direct hernioplasty is contraindicated for this type. Regarding Amyand hernias, 2 classifications are commonly used: Losanoff and Bassof classification [7] and the De Garengeot classification [8]: The Losanoff and Bassof classification system categorizes Amyand hernia into 4 types based on the condition of the appendix and the presence of associated pathology. Type 1 is a normal appendix, type 2 is an inflamed appendix, type 3 is a perforated appendix, and type 4 is an appendix with a tumor. The ancient De Garengeot classification system is based on the anatomic location of the hernia sac and the contents. Type 1 is a femoral hernia with the appendix located in the sac, type 2 is an inguinal hernia with the appendix located in the sac, and type 3 is an inguinal hernia with the appendix located outside the sac. The association of these 2 conditions is an even more unique situation.
We present a case of a perforated appendicitis within a giant type 3 Amyand hernia with its surgical management and a review of precedent cases and discussion of the literature. This work has been reported in line with the SCARE criteria [9]. Written informed consent was obtained from the patient for the publication of this case report and any accompanying images. Institutional approval was also secured for the publication of this case.
Case Report
A 56-year-old male patient with no significant past medical or surgical history presented to the Emergency Department with concerns of acute scrotal pain accompanied by fever. The duration of these symptoms was approximately 72 h prior to presentation. The patient’s vital signs upon admission were as follows: a body temperature of 38.2°C, blood pressure of 165/99 mm Hg, and heart rate of 95 beats per min. A visual analog scale rating for pain of 6 out of 10. Notably, the patient had been experiencing a progressive right-sided inguinoscrotal hernia for approximately 15 years. The hernia had become irreducible for the past year, causing intermittent discomfort.
Upon initial evaluation, the patient appeared to be in stable general condition, with the only reported symptom being acute pain localized to the right scrotal region. A thorough clinical examination revealed a giant type 3 right inguinoscrotal hernia extending below the superior border of the patellar bone (Figure 2A, 2B). Notably, there was erythema and acute tenderness localized below the right side of the scrotum, indicative of an underlying inflammatory process. A complete blood count and biochemical profile demonstrated a severe leukocytosis, with a white blood cell count of 18.5 G/L (reference range ≤11 G/L), and elevated C-reactive protein level of 311 mg/L (reference range ≤10 mg/L), suggesting a systemic inflammatory response.
Diagnostic imaging in the form of abdominopelvic computed tomography (CT) was performed to further evaluate the condition. The scan revealed a massive inguinoscrotal hernia containing the terminal ileal loop, ascending colon, and right portion of the transverse colon. Additionally, the presence of free fluid in the declivitous part of the right scrotum raised high clinical suspicion for perforated appendicitis.
Given the acute presentation and imaging findings, the decision was made to proceed with immediate surgical intervention. An initial oblique incision was made parallel to the inguinal canal in an attempt to manually reduce the hernia, but this was unsuccessful (Figure 3). Consequently, a midline laparotomy was performed to safely mobilize and reposition the herniated bowel content back into the abdominal cavity. The resulting defect in the inguinal region measured approximately 8 cm in diameter and contained the right and transverse colons, terminal ileal loop, and omentum, along with evidence of a perforated appendicitis (Figure 4).
A stapled appendectomy was performed without complications, and a partial omentectomy was carried out. The spermatic cord was intraoperatively identified, and its vascularity was confirmed through the use of an ultrasonic pen-shaped Doppler, showing a satisfactory arterial pulse. Owing to the fecal contamination and the high risk for mesh infection, a mesh-free Shouldice repair technique was used for the hernia. Two 19-Fr Blake drains were subsequently placed in situ, one in the right scrotal sac and the other within the abdominal cavity, to facilitate postoperative drainage. Skin closure was achieved using surgical staples (Figure 5).
Postoperative monitoring of intra-abdominal pressure confirmed it to be within the normal range. Histopathological analysis corroborated the diagnosis of a perforated appendiceal phlegmon, with transmural necrosis and mesoappendiceal abscesses also noted. Postoperative care proceeded without incident, with continuation of antibiotics for a 7-day period yielding favorable clinical and biological outcomes. Follow-up at 6 months postoperatively revealed the patient to be in excellent health, with no signs of hernia recurrence or other complications.
Discussion
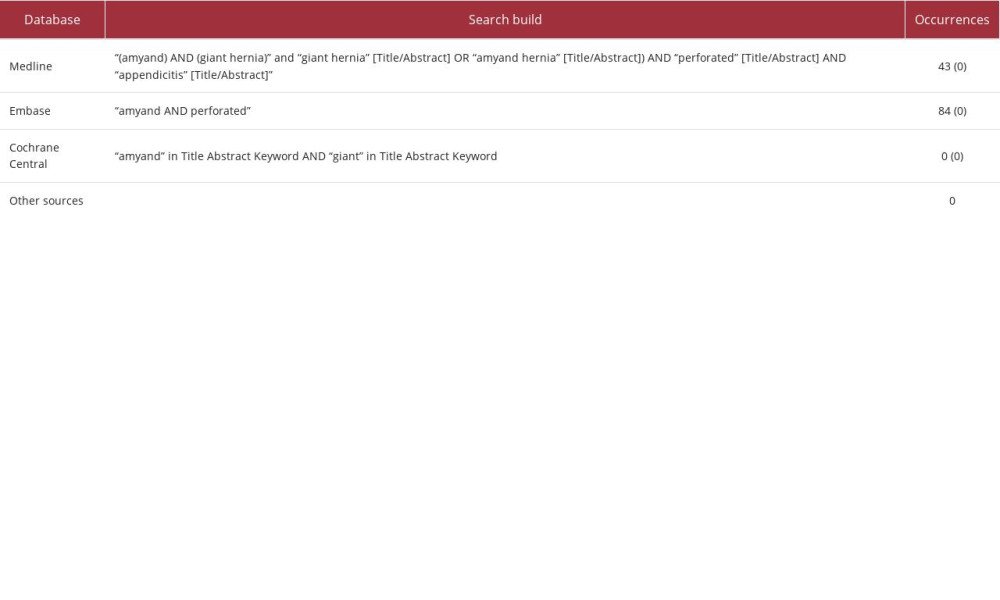
We initiated a literature search strategy on March 23, 2023, in the English-language scientific databases of MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials without any time restrictions. We sought original studies or case reports discussing giant right-sided inguinoscrotal hernias with perforated appendicitis; this search strategy is detailed in Table 1. Further, we conducted additional searches via Google and manually reviewed the reference lists of included studies. The final review yielded 127 articles related to the subject but did not uncover any articles specifically describing a giant Amyand hernia with perforated appendicitis on the right side, even after screening abstracts. This is surprising because, although this type of hernia is exceptionally rare, there have been reports of abscessed or perforated appendicitis occurring in the left groin region. However, none matched our clinical case involving the right side of the patient.
In our case, we opted for a mesh-free repair of the inguinal defect due to the presence of local fecal contamination and the elevated risk of mesh infection, despite knowing that this carries a high probability of hernia recurrence.
To the best of our knowledge, this is the first case ever reported in the English-language scientific literature describing a stage 3 giant right Amyand hernia with perforated appendicitis, marking this as an exceedingly rare condition.
This case report and its associated review contribute valuable insights to the repair options for a rare and complex condition such as a giant Amyand hernia. Surgeons must be cognizant of the potential intraoperative diagnosis of Amyand hernia and the unique surgical considerations that such cases entail.
In recent literature and recommendations, there has been growing evidence supporting the use of synthetic mesh repair in limited contaminated fields for hernia repairs, including giant Amyand hernia [10–15]. This approach has shown comparable rates of surgical site infection to endogenous repair techniques. Synthetic mesh repair offers several advantages, such as increased strength, reduced tension on the suture line, and improved tissue integration, which can be particularly beneficial in cases involving contaminated or infected surgical sites.
Despite these encouraging results, it is crucial to acknowledge that more high-quality studies are needed to reach a consensus on the optimal surgical approach for treating giant Amyand hernia. A tailored approach – taking into account individual patient characteristics, hernia size, extent of contamination, and associated comorbidities – is recommended to achieve both optimal hernia repair and effective sepsis control, thereby improving patient outcomes.
Conclusions
While synthetic mesh repair has shown promise in the management of giant Amyand hernia, further research is warranted to solidify its efficacy and long-term outcomes. Surgeons should remain vigilant about the potential diagnosis of Amyand hernia during surgery and adapt their surgical strategies accordingly. By considering the specific characteristics of each case, surgeons can optimize hernia repair techniques and effectively manage associated sepsis, leading to improved patient care and outcomes.
Figures
References:
1.. Amyand C, VIII. Of an inguinal rupture, with a pin in the appendix coeci, incrusted with stone; And some observations on wounds in the guts: Phil Trans R Soc London, 1735; 39(443); 329-42
2.. Michalinos A, Moris D, Vernadakis S, Amyand’s hernia: A review: Am J Surg, 2014; 207(6); 989-95
3.. Ivanschuk G, Cesmebasi A, Sorenson EP, Amyand’s hernia: A review: Med Sci Monit, 2014; 20; 140-46
4.. Fitzgibbons RJ, Forse RA, Clinical practice. Groin hernias in adults: N Engl J Med, 2015; 372(8); 756-63
5.. Lau WY, History of treatment of groin hernia: World J Surg, 2002; 26(6); 748-59
6.. Trakarnsagna A, Chinswangwatanakul V, Methasate A, Giant inguinal hernia: Report of a case and reviews of surgical techniques: Int J Surg Case Rep, 2014; 5(11); 868-72
7.. Losanoff JE, Basson MD, Amyand hernia: A classification to improve management: Hernia, 2008; 12(3); 325-26
8.. de Garengeot RJC, [Treatise on surgical operations.]: Chez Guillaume Cavelier; 1731 [in French]
9.. Agha RA, Franchi T, Sohrabi C, The SCARE 2020 guideline: Updating consensus Surgical CAse REport (SCARE) duidelines: Int J Surg, 2020; 84; 226-30
10.. Poelman MM, van den Heuvel B, Deelder JD, EAES Consensus Development Conference on endoscopic repair of groin hernias: Surg Endosc, 2013; 27(10); 3505-19
11.. Hodgkinson DJ, McIlrath DC, Scrotal reconstruction for giant inguinal hernias: Surg Clin North Am, 1984; 64(2); 307-13
12.. Mehendal FV, Taams KO, Kingsnorth AN, Repair of a giant inguinoscrotal hernia: Br J Plast Surg, 2000; 53(6); 525-29
13.. Patsas A, Tsiaousis P, Papaziogas B, Repair of a giant inguinoscrotal hernia: Hernia, 2010; 14(3); 305-7
14.. Staubitz JI, Gassmann P, Kauff DW, Lang H, Surgical treatment strategies for giant inguinoscrotal hernia – a case report with review of the literature: BMC Surg, 2017; 17(1); 135
15.. Hentati H, Dougaz W, Dziri C, Mesh repair versus non-mesh repair for strangulated inguinal hernia: Systematic review with meta-analysis: World J Surg, 2014; 38(11); 2784-90
Figures
In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943174
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943136
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943645
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942921
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250