10 September 2023: Articles 
Inverted Maxillary Third Molar Impaction within the Maxillary Sinus: A Rare Case Report
Unusual clinical course
Alaa Waleed AlqutubDOI: 10.12659/AJCR.941859
Am J Case Rep 2023; 24:e941859
Abstract
BACKGROUND: The maxillary third molar is considered one of the most impacted teeth and can present in different types based on the direction and depth of the impaction. However, the inverted type of maxillary third molar impaction is a rare condition, with few reported cases in the current literature.
CASE REPORT: We report an extremely rare case of a 48-year-old man with an inverted maxillary third molar situated in the maxillary sinus in direct contact with the posterior wall of the sinus, with a portion of the coronal part perforating the infratemporal fossa. Because of the anatomical and structural complexity of the impaction and because the tooth has never been symptomatic, the case was conservatively managed after weighing the risks and benefits of surgical intervention. A 2-year follow-up was made to ensure no changes in the impaction location, confirming the validity of the conservative approach.
CONCLUSIONS: This case is the first reported inverted maxillary third molar impacted in such an anatomical location. This reported case contributes to existing knowledge regarding this rare type of impaction and that this rare impaction location can present congenitally with a non-iatrogenic origin. A thorough dental history and clinical and radiographical examinations will aid dental professionals in their clinical decision making for patients with similar presentations.
Keywords: Dentistry, Maxillary Sinus, conservative treatment, Male, Humans, Middle Aged, Tooth, Impacted, Molar, Third, Rare Diseases
Background
The failure of a tooth to erupt into its final position in the dental arch within the expected time frame is defined as tooth impaction [1]. The normal process of tooth eruption could be interrupted by an adjacent tooth, dense overlying alveolar bone, thick soft tissue, insufficient space due to inadequate arch length, or genetic abnormalities. Therefore, these unerupted teeth are retained impacted unless surgical interventions are attempted to expose or remove them. Mandibular third molars are reported to be the most frequently impacted teeth, followed by maxillary third molars, maxillary canines, and mandibular premolars. Because third molars are the last teeth to erupt, they tend to be the most impacted teeth due to the inadequate space available for eruption [1].
The impacted maxillary third molar presents radiographically in various angulations and positions within the alveolar bone. In terms of angulation, vertical impaction is counted 63% of the time, while distoangular and mesioangular impactions are counted 25% and 12% of the time, respectively. Some rare positions, such as inverted, transverse, and horizontal, are present in less than 1% of cases [1,2].
The difficulty of surgical removal is determined based on the depth of the impaction compared with the height of the adjacent second molar. Class A impaction occurs when the occlusal surface of the impacted tooth is at the level of the occlusal plane of the second molar. Class B impaction implicates an impacted tooth with an occlusal plane between the occlusal and cervical lines of the adjacent molar. Class C impaction occurs when the occlusal plane of the impacted tooth is lower than the cervical line of the adjacent molar [2].
Third molar impaction removal is the most common surgical operation performed by oral and maxillofacial surgeons. However, the challenge is to decide on the appropriate management rather than the treatment. The decision of whether an impacted third molar should be removed depends on a variety of factors. Clinicians should weigh the risk–benefit ratio of retaining the impaction versus surgical removal to reach a systematic, patient-oriented approach for optimal management [3].
This reported case of the maxillary third molar was an inverted impaction, which is an extremely rare type of impaction [2,4–6]. In addition, the interesting original anatomical location of the tooth within the maxillary sinus makes it the first reported case in such a position with a non-iatrogenic origin.
Case Report
CLINICAL MANAGEMENT:
The surgical procedure to remove the inverted impaction through transinusal access was proposed. However, considering the patient age, asymptomatic history of the impacted tooth, and the possible surgical complications due to the impaction position and location, the patient and the clinician opted to keep the tooth in situ. A 2-year follow-up was made to rule out changes in the impaction location by comparing the images obtained by CBCT with the partial comparison analysis program 3-matic Research 13.0 (Materialise NV, Belgium) software tool (Figure 6). The comparison revealed no changes in the location of the impaction over 2 years.
Discussion
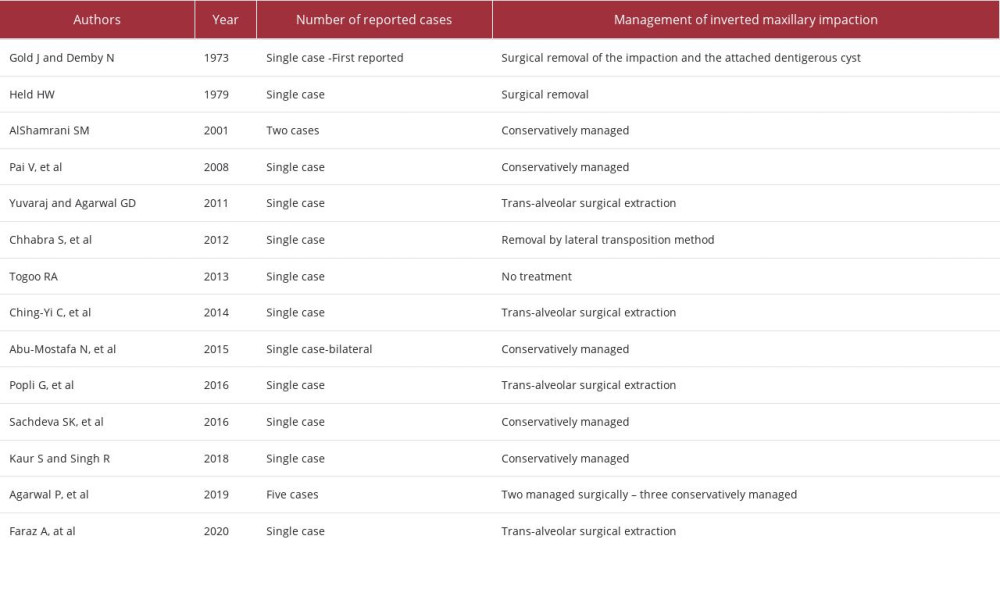
The inverted presentation of the maxillary third molar is very rare, with few reported cases in the current literature [2–16] (Table 1). An inverted impaction is discovered radiographically when the crown of the third molar faces up toward the maxillary sinus, while the apex of the root points down toward the crest of the alveolar ridge [3–5]. The etiology of the inverted position is unclear. Abnormal or atypical odontogenic epithelium proliferation before the development of a tooth germ can cause tooth inversion [17]. Impactions of this type remain in their positions for years without manifesting clinically [4]. Rarely, that could lead to resorption of the adjacent tooth or cause serious complications, such as an ectopic eruption into the nasal floor or the development of a pathological lesion [6]. The location of the inverted impaction challenges surgical manipulation and removal, as there is a chance that the tooth will be dislodged into the maxillary sinus floor, orbital floor, infratemporal fossa, or temporal space, which complicates the surgical procedure [2].
The exact etiology of impacted teeth in the maxillary sinus is also unclear. Any interruption of the tooth development process, developmental anomalies, crowding of dentition, trauma, or iatrogenic predispositions can cause the impaction in the maxillary sinus. In some cases, the impaction has an idiopathic etiology [18].
This rare form of impaction is the first reported case of maxillary third molar impaction in such an inverted, rare anatomical position with an idiopathic origin. The inverted maxillary third molar impaction is congenitally located in the thick posterior wall of the maxillary sinus, with part of the coronal portion perforating the infratemporal fossa.
The posterior wall of the maxillary sinus is formed by the body of the superior portion of the maxilla and contains the alveolar canal, which transmits the posterior superior alveolar vessels and nerves to the posterior teeth. The infratemporal fossa lies behind the posterior wall of the maxillary sinus [19].
In a systemic research study conducted by Mavriqi et al, a total of 34 cases were reported for third molars located in the maxillary sinus, with associated symptoms such as headache, sinusitis, facial pain, or totally asymptomatic. They reported the most common locations of the maxillary third molar in the maxillary sinus as presented at the posterior wall (24.13%), lateral wall (22.41%), medial wall (18.96%), inferior wall (17.24%), orbital floor (15.51%), and rarely at the anterior wall (1.72%) of the sinus [20].
The risk-benefit ratio was assessed before making a decision about the management of this case. Although maxillary impacted tooth displacement into the maxillary sinus or infratemporal fossa is rare [21], this case displayed a considerable risk of tooth displacement into these spaces due to its position within the sinus. The high position and complex relationship of this impacted third molar with the posterior wall of the maxillary sinus complicates the surgical procedure, and the accessibility to the tooth in such an inverted position is very challenging, with high morbidity [22]. The procedure comprises a significant number of complications: displacement of the tooth into the sinus, sinus membrane perforation, and bleeding are possibly encountered intraoperatively. Postoperative complications can include the risk of infection spreading due to the existing sinusitis, which can prolong the healing process [23].
The displacement of the inverted impacted tooth into the infratemporal fossa or temporal fossa is another reported potential complication [21]. The infratemporal fossa is bordered anteriorly by the thin maxillary cortex that constitutes the posterior border of the maxillary sinus. Later, the infratemporal fossa communicates with the pterygopalatine fossa. It contains many vital structures, such as the maxillary artery, the sphenopalatine nerve, the venous pterygoid plexus, and the pterygoid muscles. In addition to the anatomical and structural complexity of the infratemporal fossa, the deep location makes tooth displacement and retrieval a major hazard, with possible hemorrhaging and nerve injury. Guégan et al conducted a systematic review of clinical cases dating from 1977 to 2020. They surveyed the iatrogenic displacement of the maxillary third molar into the infratemporal fossa or the temporal fossa reported in the literature and reported a total of 27 clinical cases of projected teeth, in which 22 teeth were projected into the infratemporal fossa and 5 teeth were projected into the temporal fossa. They concluded that these complications should be managed carefully, following a structured decision-making process; otherwise, they can lead to further complications [22].
Different surgical approaches for the removal of impacted teeth from the maxillary sinus have been proposed. The Caldwell-Luc technique, trans-nasal endoscopic, and transinusal approaches are used in such cases. The Caldwell-Luc procedure provides high visibility into the sinus. However, it is associated with more morbidities than is the trans-nasal endoscopic approach. The Caldwell-Luc procedure requires a large opening in the anterior maxillary sinus wall to access the impacted tooth with higher risk of complications. The trans-nasal endoscopic technique is a minimally invasive technique used mainly for teeth presented in the paranasal cavities. It has the advantage of visualization of orbital floor defects. The transinusal approach is more invasive but the visibility is significantly better than the endoscopic-assisted approach [20,24]. The suggested surgical intervention in the present case was the transinusal approach, because of the inverted position and the location of the impaction at the posterior wall of the sinus, which presents a high risk of displacement of the tooth into the maxillary sinus. However, the conservative approach was adopted in this case.
Precisely locating the tooth is crucial to avoid possible complications and to aid in the decision-making process. Computed tomography (CT) is an elemental diagnostic tool for managing these clinical situations, as orthopantomogram is a less accurate, unreliable X-ray and is limited by distortion and superimposition of anatomical structures. Therefore, use of orthopantomogram can lead to improper diagnosis and management [20]. In this case, we used CBCT to precisely locate the original site of the impaction. Cross-sectional imaging provides more accurate localization, and therefore, more reliable diagnosis and treatment planning can be achieved [18].
CBCT and medical CT or VCT can both be used for dental imaging. However, VCT has higher contrast resolution, highlighting the discrimination between different tissue types [25]. Hence, an additional VCT was made for the purpose of case reporting after obtaining the patient’s consent.
There is no conclusive treatment procedure to remove inverted and impacted maxillary third molars. The conservative approach is considered the safest option, as long as the tooth is asymptomatic and has no related pathological manifestations [11]. Therefore, the clinician and the patient opted to retain the impacted tooth in this case, and an annual clinical and radiological examination was planned to detect any positional or pathological alterations. A 2-year follow-up was done, and CBCT images were assessed for pathological changes and were superimposed using part comparison analysis to validate the location of the tooth, with no changes detected over 2 years (Figure 6). This validates the conservative treatment approach followed in this case.
This case highlights the extremely uncommon nature of such impactions and underscores the importance of proper diagnosis and management in similar situations. By documenting and reporting this case, we aim to contribute to the existing knowledge regarding this rare type of impaction, ultimately aiding dental professionals in their clinical decision making for patients with similar presentations.
Conclusions
Inverted maxillary third molar impaction is a rare condition that requires careful clinical and radiographic appraisal for effective management. It is crucial to assess the location of the impaction using advanced radiographic imaging techniques to develop a patient-oriented surgical plan. Conservative management is generally the preferred approach, especially when the patient is asymptomatic. This involves closely monitoring the impaction without immediate surgical intervention. Regular follow-ups and periodic imaging can help evaluate changes in the condition over time. However, if symptoms or complications arise, surgical intervention should be considered after a thorough evaluation of the potential risks. By following these guidelines, dental professionals can effectively manage similar conditions and ensure optimal patient outcomes. In this case, we followed a systematic approach for the clinical management. Because of the anatomical and structural complexity of the impaction and the asymptomatic history of the tooth, conservative management and regular follow-ups were applied.
Figures
References:
1.. Hupp JR, Principles of management of impacted teeth.: Contemporary Oral and Maxillofacial Surgery, 2014; 143-67
2.. Agarwal P, Kumar S, Jain K, Kiran K, Inverted maxillary third molar impactions: Ann Maxillofac Surg, 2019; 9; 484-88
3.. Park W, Kim JH, Kang SH, Reconsideration of decision making for third molar extraction: J Korean Assoc Oral Maxillofac Surg, 2011; 37(5); 343-48
4.. Gold J, Demby N, Rare inverted maxillary third molar impaction: Report of case: J Am Dent Assoc, 1973; 87(1); 186-88
5.. Held HW, Inverted maxillary molar: Dent Radiogr Photogr, 1979; 52(4); 87
6.. Yuvaraj , Agarwal GD, Inverted maxillary third molar impaction – a case report: Peoples J Sci Res, 2011; 4(1); 57-58
7.. AlShamrani SM, Inverted and impacted maxillary third molar. Report of two cases: Odontostomatol Trop, 2001; 24; 15-17
8.. Chhabra S, Chhabra N, Dhillon G, Inverted and impacted maxillary third molar: Removal by lateral transposition method: Int J Exper Dent Sci, 2012; 1(1); 26-29
9.. Togoo RA, Rare occurrence of inverted maxillary third molar impaction: A case report: J Int Oral Health, 2013; 5(3); 85-87
10.. Chen CY, Wang WC, Lin LM, Chen YK, Incidental detection of a rare inverted and impacted maxillary third molar in a patient of mandibular unicystic ameloblastoma: Dentistry, 2014; 4; 213
11.. Abu-Mostafa N, Barakat A, Al-Turkmani T, Al-Yousef A, Bilateral inverted and impacted maxillary third molars: A case report: J Clin Exp Dent, 2015; 7(3); e441-43
12.. Popli G, Bansal V, Dubey P, Inverted impacted maxillary third molar: A rare occurrence: Int J Oral Health Med Res, 2016; 3(1); 101-2
13.. Sachdeva SK, Jayachandran S, Kayal L, Bakyalakshmi K, Inverted and impacted maxillary and mandibular third molar: Unusual case reports with review of the literature: Saudi J Med Med Sci, 2016; 4; 32-34
14.. Kaur S, Singh R, Rare occurrence of impacted and inverted maxillary third molar – a case report: Int J Curr Res Med Sci, 2018; 4(4); 53-55
15.. Pai V, Kundabala M, Sequier PS, Rao A: J Oral Health Community Dent, 2008; 2; 8-9
16.. Faraz A, Fatima A, Faraz S, Rare occurrence of inverted and impacted maxillary third molar: A case report: Int J Drug Res Dental Sci, 2020; 2(4); 105-9
17.. Rammal M, Alfonso C, An unusual case of an inverted and impacted maxillary third molar: Oral Surg, 2013; 7(2); 109-11
18.. Lai YT, Luk YS, Fung KH, Anomalous morphology of an ectopic tooth in the maxillary sinus on three-dimensional computed tomography images: J Radiol Case Rep, 2013; 7(2); 11-16
19.. Ganesan K, Rathod N, Maxillary Sinusitis.: Oral and Maxillofacial Surgery for the Clinician, 2021, Singapore, Springer
20.. Mavriqi L, Lorusso F, Tartaglia G, Transinusal pathway removal of an impacted third molar with an unusual approach: A case report and a systematic review of the literature.: Antibiotics (Basel), 2022; 11(5); 658
21.. Gómez-Oliveira G, Arribas-García I, Álvarez-Flores M, Delayed removal of a maxillary third molar from the infratemporal fossa: Med Oral Patol Oral Cir Bucal, 2010; 15(3); e509
22.. Guégan B, Casenave T, Lapeyrie P, Benard V, Management of third molars projected into the temporal fossa and infratemporal fossa: Systematic literature review: J Oral Med Oral Surg, 2023; 29(1); 11
23.. Testori T, Weinstein T, Taschieri S, Wallace SS, Risk factors in lateral window sinus elevation surgery: Periodontol 2000, 2019; 81(1); 91-123
24.. Alhashim FY, Almarhoon FS, Alhashim HY, Moumen A, Endonasal endoscopic management of different cases of dentigerous cysts and ectopic teeth.: J Surg Case Rep., 2021; 2021(4) rjab099
25.. Botticelli S, Verna C, Cattaneo PM, Two-versus three-dimensional imaging in subjects with unerupted maxillary canines.: Eur J Orthod, 2011; 33(4); 344-49
Figures
In Press
02 Apr 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942681
03 Apr 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943597
03 Apr 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943392
04 Apr 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943271
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250