23 February 2024: Articles 
Definitive Closure Using an Ovine Reinforced Tissue Matrix in Contaminated Penetrating Abdominal Trauma
Unusual clinical course, Challenging differential diagnosis, Management of emergency care, Clinical situation which can not be reproduced for ethical reasons
Luis G. Fernandez1ABDEF*, Jason Murry1B, Marc R. Matthews2ADE, Christopher L. Thompson3CD, Mohamed Abdelgawad1F, Rebekah Bjorklund1FDOI: 10.12659/AJCR.943188
Am J Case Rep 2024; 25:e943188
Abstract
BACKGROUND: Cases involving penetrating abdominal trauma may be complex and often involve damage to multiple organ systems. Synthetic, biologic, and reinforced biologic matrices/reinforced tissue matrices (RBMs/RTMs) are frequently used in hernia repair and other surgical procedures requiring reinforcement, including trauma cases that require abdominal repair.
CASE REPORT: The first case was a 35-year-old male patient with a stab wound (SW) to the right side of the chest and the abdomen resulting in damage to the diaphragm, epicardium, liver, and duodenum. The second case was a 22-year-old male patient who suffered multiple traumas after an automated trencher accident, including a skull fracture with exposed brain and major lacerations to the shoulder and abdomen causing a large right-flank hernia. In both cases, OviTex® (TELA Bio, Inc., Malvern, PA), a reinforced tissue matrix (RTM), was used to help obtain and maintain abdominal wall closure. We also present an institutional economic analysis using data from the author’s institution with average case cost and future projections for procedure volume and product usage volume through 2021.
CONCLUSIONS: We report favorable outcomes in a series of patients with contaminated (CDC Wound Class III) surgical fields who underwent abdominal wall closure and reinforcement with OviTex RTM. Our work adds to the growing body of literature suggesting that reinforced biologics offer a potential alternative to biological meshes in the setting of a contaminated surgical field. Additionally, in comparison to other commonly available biologic matrices, use of OviTex RTM may be a cost-effective option to achieve abdominal wall closure even in complex cases.
Keywords: Abdominal Wall, intra-abdominal hypertension, Soft Tissue Infections, Soft Tissue Injuries, Surgical Mesh
Background
Synthetic, biologic, and reinforced biologic matrices/reinforced tissue matrices reinforced (RBMs/RTMs) are frequently used in hernia repair and other surgical procedures requiring reinforcement, including trauma cases requiring abdominal repair [1–3]. Penetrating abdominal trauma patients are frequently seen in both urban and suburban/rural trauma centers in the US (35%/12%, respectively) [4,5]. Cases involving penetrating abdominal trauma may be complex, as they often involve damage to multiple organ systems in the setting of gross contamination [4–7].
Case Reports
CASE 1:
A 35-year-old male Hispanic patient presented with a stab wound (SW) to the right side of the chest and the abdomen that resulted in lacerations to the diaphragm, epicardium, liver, and duodenum with significant gastrointestinal contamination. We performed damage control surgery (DCS), open abdomen (OA), right lateral thoracotomy, repair of central tendon laceration of the diaphragm, inferior medial sternotomy with repair of an epicardial laceration, exploratory celiotomy, repair of Grade III duodenal injury and a Grade IV liver laceration with negative-pressure would therapy and temporary abdominal closure (NPWT/TAC, ABTHERA ADVANCE™ Open Abdomen Dressing, 3M, Saint Paul, MN) (Figures 1, 2). The patient had clinical evidence of abdominal compartment syndrome (ACS) (Figure 2).
On hospital day (HD) 9, the patient underwent resection of a segment of necrotic liver (Cuinaud Segment IIB), with primary fascial closure, and negative-pressure wound therapy (NPWT, 3M™ V.A.C.® Therapy, 3M, Saint Paul, MN) (Figure 3). On HD 14, the patient’s upper midline incision dehisced due to bile digestion and necrosis of the native fascia. The patient underwent debridement of the necrotic fascia, myocutaneous advancement of the abdominal wall, with an overlay placement of two 8-layer OviTex 2S Resorbable RTMs (20×20 cm and 20×16 cm, respectively) (Figure 4).
On clinical follow-up (29 days after discharge home, 58 days after the index surgery), the physical exam showed no evidence of a ventral hernia (Figure 5).
In Case 1, the use of two 8-layer ovine RTM (OviTex 2S Resorbable; 20×16 cm and 20×20 cm) was effective in providing definitive abdominal fascial closure in a hostile environment. Despite exposure to bile, the ovine RTM was able to retain its integrity and showed no evidence of wound infection or dehiscence. To date, the patient has not reported having a ventral hernia (Figure 5).
CASE 2:
Open skull fracture with exposed brain, major lacerations to the shoulder, right hemithorax and abdomen causing a large right-flank hernia due to an automated trencher accident (Figure 6A).
A 22-year-old male white patient suffered multiple trauma due to an automated trencher accident, including a skull fracture with exposed brain and major lacerations to the shoulder and abdomen causing a large right-flank hernia (20×15 cm defect), with gross environmental contamination and devitalized tissue due to shear force trauma (Figure 6A, 6B). Damage control surgery (DCS) was done and a cranial subcutaneous flap advancement closure along with debridement and repair of the avulsion of the right diaphragm was performed. A right hemicolectomy with primary anastomosis was done and a 10×20 cm 6-layer OviTex 1S Resorbable RTM was used as a sublay repair (Figure 6C) for the right-flank hernia (Figure 6B). NPWT/TAC was applied to the open abdomen and the thoraco-abdominal flank incision (Figure 6D, 6E).
On HD 2 the patient returned to the OR for an abdominal wash-out using HOCL solution (Vashe®, Urgo Medical North America, Fort Worth, TX), a cholecystectomy, and a primary abdominal closure with placement of a closed-incision negative-pressure therapy wound dressing (PREVENA™ Incision Management System, 3M, Saint Paul, MN) and a forearm debridement and re-application of wound VAC.
On HD 3, the patient was extubated. He followed commands but had mild-to-moderate expressive aphasia, which improved with speech therapy. Serial head CTs were unremarkable. The left chest tube and the right hepatic fossa Jackson Pratt drain were removed. On HD 8, the patient was taken back to the OR with orthopedic surgery for irrigation and debridement of the right forearm, a right posterior interosseous nerve reconstruction using a nerve allograft (AxoGen® Advance Nerve Graft, Alachua, Fl), right extensor carpi radialis longus muscle repair, and partial wound closure with re-application of NPWT dressing.
The patient tolerated the procedure well, was extubated postoperatively, and was transferred back to the intensive care unit. Final irrigation and debridement with full closure of the right elbow wound was done by the hand service on HD 10. The patient continued to do well clinically and the aphasia had totally resolved with no residual neurologic deficits. He was discharged home on HD 13 (Figure 7).
In Case 2, a 6-layer ovine RTM (OviTex 1S Resorbable; 10×20 cm) was used to achieve abdominal wall closure as part of the initial repair of a complex, traumatic right-flank hernia. This patient did not require mesh revision nor develop any wound complications. The right flank, abdominal wall reconstruction with the ovine RTM provided an excellent clinical result, with no evidence of wound infection or dehiscence.
INSTITUTIONAL ECONOMIC ANALYSIS: An economic analysis was performed using data from our institution, where both XenMatrix™ and OviTex have been used in complex abdominal wall repairs (Figure 8). With 95% confidence, the average case cost with XenMatrix will be within ±$3517 of $1817, with sample size (n) of 50 cases (Figure 8A). These procedures have an average case time of 207 minutes and 157 minutes cut-to-close. This graph presents a skew of 1.68. A positive skew indicates more values lie below the mean distribution. These graphs will typically present with a “tail” that extends toward the higher values. With 95% confidence, the average case cost with OviTex RTM will be within ±$4335 of $12 271 (Figure 8B). Sample size (n) of 13 cases. These procedures have an average case time of 180 minutes and 126 minutes cut-to-close. This graph presents a skew of 0.45. Similar to Figure 8A, the smaller “tail” also extends toward the higher values in Figure 8B.
A cost analysis was performed assuming consistent surgical case time across procedures, which resulted in a potential total cost savings of $2953.67 per case if all XenMatrix cases are converted to OviTex RTM products. There has been an average incremental increase of potential procedures by 17.9% year-over-year (YOY) in which OviTex RTM or XenMatrix could be used (over a 5-year period, 2016–2020). Of these cases, actual product usage of OviTex RTM and XenMatrix grew by an average of 4.1% over a 3-year period. Please note, OviTex RTM and XenMatrix were not available in our market in 2016 and 2017.
Procedure volume is projected to increase in volume by 10.54%, reducing the average procedure growth from 17.9% to 16.5% (Figure 9). This decrease for the average growth from 17.9% to 16.5% is because the hospital saw a decline in cases across all service lines due to Covid-19 restrictions. Despite this, the overall 2021 projection still increased. Product usage is projected to increase to 14.9% from 2020 to 2021. This will raise the average case use of product from 4.1% to 6.8%.
Potential 5-year cost savings were predicted using 2 models (Figure 10). The first is a conservative model of future cost savings based on an incremental procedure volume growth of 0% and a product usage volume increase of 5%. After 5 years, the facility would save a total of $359 875 (Figure 10A). The second projected growth model presents future cost savings based on an incremental procedure volume growth of 10.54% and a product use increase of 6.8%. After 5 years, the facility would save a total of $549 931 (Figure 10B).
Discussion
The use of surgical mesh is common in hernia repair. While biological meshes are routinely used for contaminated fields, the use of reinforced meshes may be an attractive alternative [8]. In our series, we demonstrated favorable outcomes with the use of an ovine RTM for the management of patients with complex, grossly contaminated, open thoraco-abdominal trauma.
Surgical fascial closure has evolved throughout the years, from various suturing techniques to the meshes available today, including synthetic, resorbable synthetic, biological, and reinforced biologic mesh. Use of permanent synthetic meshes significantly reduced hernia recurrence rates as compared to simple suturing, although rates of incisional wound complications have been reported [9–11] and often require surgical reintervention.
A study of 1071 patients who were followed for a median of 5 years noted a 5.1% explanation rate [12]. Biological meshes have been generally indicated for use in contaminated fields. Several studies have demonstrated impressive efficacy [13,14], but their cost has limited their widespread use [15,16]. Use of reinforced biologic meshes has been suggested. Recent experience with synthetic reinforced biological mesh (hybrid mesh) suggests that by decreasing the degree of inflammation (as compared to permanent synthetic mesh) they provide adequate strength with acceptable rates of recurrence [17,18].
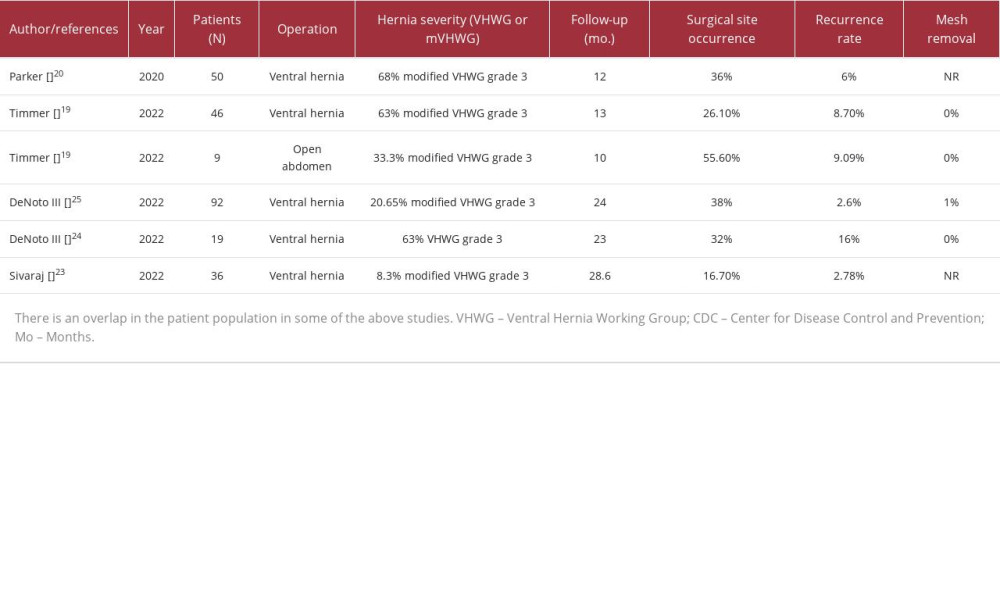
The use of these hybrid meshes in contaminated surgical fields is increasing. A list of studies on the use of OviTex is shown in Table 1 [19–25]. The rate of surgical site occurrence (SSO), defined as patients who had developed an infection or complication at the surgical site, ranged between 0% and 55.6%. The variance of SSO tended to correlate with case complexity, with Timmer et al reporting a 55.6% SSO rate in open abdomen cases, which decreased to 26.1% in ventral hernia repairs [12]. Of note, the rates of recurrence were low, with most reporting rates below 10%. One prospective trial including 92 patients reported a 2.6% Kaplan-Meier estimated recurrence rate at 24 months [25]. In our series, we reported no incidences of SSO or recurrence.
An advantage of the use of OviTex RTM is its favorable cost profile as compared to biological mesh. A study by Reynolds et al reported the costs of 46 ventral hernias cases repaired without mesh, 79 repaired with synthetic mesh, and 48 repaired with biologic mesh [26]. They reported a median cost of $5432 without mesh, which increased to $7590 using synthetic mesh and to $16 970 using biological meshes (
The advantage of case reporting is the ability to detect novel clinical findings, pathologic presentations, and interventions [27]. However, case reports, such as this one, are limited in their general application by small sample sizes; therefore, causal inference and generalization may not be possible. Inherent bias and over-interpretation of the clinical outcome are other known potential confounding factors associated with limited case series. Our intent was to encourage a further, more robust analysis, of the feasibility, safety, and effectiveness of the use of OviTex RTM in the setting of a contaminated wound environment.
Conclusions
We report favorable outcomes in 2 patients with abdominal trauma, in grossly contaminated surgical fields, who underwent abdominal wall closure and reinforcement with OviTex RTM. Our work adds to the growing body of literature showing that hybrid reinforced biologics offer a potential alternative to non-reinforced biological meshes in the setting of a grossly contaminated surgical field.
Both cases required surgical repair with a resilient, hybrid reinforced biologic mesh to achieve closure of the abdominal defect. In these 2 cases, the ovine RTM provided an effective and durable abdominal wall reconstruction, and the use of an ovine RTM saved our institution US $1874–$10 473 per case. Based on our experience, we believe that Ovine RTMs may be a cost-effective option to achieve abdominal wall closure in complex, contaminated cases.
Figures
References:
1.. Faylona JM, Evolution of ventral hernia repair: Asian J. Endosc. Surg, 2017; 10; 252-58
2.. DeNoto G, Ceppa EP, Pacella SJ, A prospective, single arm, multi-center study evaluating the clinical outcomes of ventral hernias treated with OviTex® 1S permanent reinforced tissue matrix: The BRAVO Study 12-month analysis: J Clin Med, 2021; 10(21); 4998
3.. Holihan JL, Hannon C, Goodenough C, Ventral hernia repair: A meta-analysis of randomized controlled trials: Surg Infect, 2017; 18; 647-58
4.. , Office of Statistics and Programming, National Center for Injury Prevention and Control, Centers for Disease Control and Prevention WISQARS Details of Leading Causes of Death . Accessed Jan 20, 2020www.cdc.gov/injury/wisqars/index.html
5.. LoCicero J, Mattox KL, Epidemiology of chest trauma: Surg Clin North Am, 1989; 69; 15-19
6.. Miniño AM, Anderson RN, Fingerhut LA, Deaths: Injuries, 2002: Natl Vital Stat Rep, 2006; 54(10); 1-124
7.. Berg R, Karamanos E, Inaba K, The persistent diagnostic challenge of thoracoabdominal stab wounds: J Trauma Acute Care Surg, 2014; 76(2); 418-23
8.. Sawyer M, Ferzoco S, DeNoto III G, A polymer-biologic hybrid hernia construct: Review of data and early experiences: Polymers, 2021; 13(12); 1928
9.. Burger JW, Luijendijk RW, Hop WC, Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia: Ann Surg, 2004; 240(4); 578-83
10.. Kokotovic D, Bisgaard T, Helgstrand F, Long-term recurrence and complications associated with elective incisional hernia repair: JAMA, 2016; 316(15); 1575-82
11.. Luijendijk RW, Hop WC, Van Den Tol MP, A comparison of suture repair with mesh repair for incisional hernia: N Engl J Med, 2000; 343(6); 392-98
12.. Hawn MT, Gray SH, Snyder CW, Predictors of mesh explantation after incisional hernia repair: Am J Surg, 2011; 202(1); 28-33
13.. Bellows CF, Shadduck P, Helton WS, Early report of a randomized comparative clinical trial of Strattice™ reconstructive tissue matrix to lightweight synthetic mesh in the repair of inguinal hernias: Hernia, 2014; 18; 221-30
14.. Ansaloni L, Catena F, Coccolini F, Inguinal hernia repair with porcine small intestine submucosa: 3-year follow-up results of a randomized controlled trial of lichtenstein’s repair with polypropylene mesh versus surgisis inguinal hernia matrix: Am J Surg, 2009; 198(3); 303-12
15.. Butler CE, Prieto VG, Reduction of adhesions with composite AlloDerm/polypropylene mesh implants for abdominal wall reconstruction: Plast Reconstr Surg, 2004; 114(2); 464-73
16.. FitzGerald JF, Kumar AS, Biologic versus synthetic mesh reinforcement: What are the pros and cons?: Clin Colon Rectal Surg, 2014; 27(4); 140-48
17.. See CW, Kim T, Zhu D, Hernia mesh and hernia repair: A review: Eng Regen, 2020; 1; 19-33
18.. Costa A, Adamo S, Gossetti F, Biological scaffolds for abdominal wall repair: Future in clinical application?: Materials (Basel), 2019; 12(15); 2375
19.. Timmer AS, Claessen JJ, Brouwer de Koning IM, Clinical outcomes of open abdominal wall reconstruction with the use of a polypropylene reinforced tissue matrix: A multicenter retrospective study: Hernia, 2022; 26(5); 1241-50
20.. Parker M, Kim RC, Barrio M, A novel biosynthetic scaffold mesh reinforcement affords the lowest hernia recurrence in the highest-risk patients: Surg Endosc, 2021; 35(9); 5173-78
21.. Sawyer MA, New ovine polymer-reinforced bioscaffold in hiatal hernia repair: JSLS, 2018; 22(4); e2018.00057
22.. Ferzoco SJ, Early experience outcome of a reinforced bioscaffold in inguinal hernia repair: A case series: Int J Surg Open, 2018; 12; 9-11
23.. Sivaraj D, Henn D, Fischer KS, Reinforced biologic mesh reduces postoperative complications compared to biologic mesh after ventral hernia repair: Plast Reconstr Surg Glob Open, 2022; 10(2); e4083
24.. DeNoto III G, Bridged repair of large ventral hernia defects using an ovine reinforced biologic: A case series: Ann Med Surg (Lond), 2022; 75; 103446
25.. DeNoto III G, Ceppa EP, Pacella SJ, 24-month results of the BRAVO Study: A prospective, multi-center study evaluating the clinical outcomes of a ventral hernia cohort treated with OviTex® 1S permanent reinforced tissue matrix: Ann Med Surg (Lond), 2022; 83; 104745
26.. Reynolds D, Davenport DL, Korosec RL, Roth JS, Financial implications of ventral hernia repair: A hospital cost analysis: J Gastrointest Surg, 2013; 17(1); 159-66
27.. Jenicek M: Clinical case reporting in evidence-based medicine, 1999, Oxford, UK, Butterworth Heinemann
Figures
In Press
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943645
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942921
22 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943346
24 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943560
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250