31 March 2024: Articles 
Surgical Treatment of Spontaneous Superficial Temporal Artery Arteriovenous Malformation: A Case Report
Challenging differential diagnosis, Rare disease, Congenital defects / diseases
Leslie R. Elmore1ABEF*, Christopher Esper1E, Andrei I. GritsiutaDOI: 10.12659/AJCR.942839
Am J Case Rep 2024; 25:e942839
Abstract
BACKGROUND: An arteriovenous malformation (AVM) is an abnormal connection between an artery and a vein, bypassing the capillary network. An AVM of the superficial temporal artery (STA) can occur after trauma, iatrogenic injury, infection, or spontaneously. Spontaneous, or iatrogenic, presentations of STA AVM are thought to be rare, with very few reported cases. Symptoms include local pain, headache, tinnitus, or paresthesia, in addition to a palpable mass associated with thrill on palpation. Options for diagnosis include intra-arterial angiography, doppler ultrasound, magnetic resonance angiography (MRA), and computed tomography angiography (CTA). Current management options include surgical excision, ligation, and embolization; however, it is unknown which treatment is superior in terms of recurrence and which carries a lower risk of complications.
CASE REPORT: We present a case of a spontaneous STA AVM in a 76-year-old woman with past medical history significant for seasonal allergies and hyperlipidemia, who presented with pulsatile tinnitus and a palpable, tender mass located to the left temporal area. The mass had been present for several years, with gradual increase in size two to three years prior to presentation. She denied any history of trauma or procedure prior to presentation of the pulsatile mass. She underwent open excision with complete resolution of symptoms and no recurrence at 11-month follow-up.
CONCLUSIONS: AVM of the STA is a condition that can occur secondary to trauma, infection, iatrogenic injury, or spontaneously. Spontaneous, or iatrogenic, presentations of STA AVM are thought to be rare, with very few cases documented in the literature. Surgical treatment remains the standard of management, with options including surgical excision, ligation, or embolization.
Keywords: Temporal Arteries, Arteriovenous Malformations, spontaneous
Introduction
An AVM is an abnormal connection between an artery and a vein, bypassing the capillary network [1]. An AVM of the STA is thought to occur spontaneously or secondary to trauma, infection, or iatrogenic injury [2,3]. There have been several reports documenting AVM secondary to trauma or iatrogenic injury. However, spontaneous STA AVM are thought to be rare [4]. This article presents a case of a spontaneous STA AVM and discusses pathogenesis, clinical manifestations, treatment options, and outcomes.
Case Report
A 76-year-old woman with past medical history significant for seasonal allergies and hyperlipidemia presented with a palpable mass of the left temporal area associated with tenderness and tinnitus. She stated that the mass had been present for approximately 10 years prior to presentation, with noted gradual increase in size over the past few years. She had undergone in-office open incision and drainage by another provider two to three months prior to presentation, without change in symptoms and persistent mass. She was administered NSAIDS and steroids, which did not improve her symptoms. She denied any history of trauma or family history of arterial malformations. On physical exam, a pulsatile, well-circumscribed mass measuring 1.0×1.0 cm was noted in the left temporal area and was found to be tender to palpation. Laboratory test results were within normal limits. Computed tomography angiography (CTA) was performed, which noted a 1.3×1.0 cm arteriovenous malformation nidus within the left temporal subcutaneous tissues with arterial feeders mainly from the left external carotid artery and draining veins (Figure 1).
After preoperative evaluation, we proceeded with open re-section of the AVM under general anesthesia. Open resection was chosen to provide complete resection with low risk of recurrence and complications. Ultrasound was used intraoperatively and a pulsatile mass was identified in the subcutaneous tissue with both arterial and venous components (Figure 2). The main inflow was noted to be the superficial temporal artery, with 2 branching outflow arteries. Arterial control of the superficial temporal artery was obtained and a parietal branch of the frontal branch of the STA was skeletonized and controlled utilizing 2-0 silk ties and reinforced with medium hemoclips (Figure 3). The STA was also controlled with 2-0 silk ties and reinforced with medium hemoclips. All 4 points were then transected, and the AVM was completely excised.
The postoperative course was uneventful and the patient was discharged on the same day. The pathology results reported an arteriovenous malformation without evidence of atherosclerosis. On postoperative follow-up at both 2 weeks and 11 months, the patient stated that her tinnitus had resolved, and the mass was no longer palpable.
Discussion
The STA lies between the skull and subcutaneous tissues, thus allowing it to be prone to injury. It has two branches: the frontal and the parietal branch [5]. The STA and respective vein lie in close proximity, allowing opportunity for an AVM to form [6]. The term cirsoid aneurysm can be used to describe AVMs that are localized to the scalp [3,7].
There are many possible causes for an AVM of the STA. An AVM of the STA can occur as a result of trauma, iatrogenic injury, or, in rare cases, spontaneously [2,8]. Li et al found that an AVM can be postinfectious in nature [3], but the exact cause remains unknown. It is estimated that 95% of these cases are a result of trauma or iatrogenic manipulation [1]. Morare et al estimated that about 75% of scalp AVM are secondary to trauma, making spontaneous malformations rare [9]. One source estimates that scalp AVMs count for 8.1% of 800 known AVMs from a literature review [3]. Furthermore, AVM of the head and neck are reported to occur in 0.1% of the population, with only 0.5% to 2.0% of these involving the STA [9]. Li et al estimates 36 patients with AVF of the STA have been reported, with 6 cases being spontaneous [3]. Matsushige found that 42 cases of spontaneous AVM of the scalp were documented between 1973 and 2003. However, it is unclear how many of these 42 cases involve the STA [10]. We report 38 known cases of spontaneous STA AVM documented in the literature, including our present case report.
Spontaneous arteriovenous fistulas are rare, and the etiology remains unclear. Selleck et al hypothesized that an AVM occurs secondary to errors in development between gestational weeks 4-6, with some of these being prompted by hormones [11]. Komatsu et al echoes this theory, stating that an AVM may “result from failure of the embryonic vasculature to differentiate into arteries and veins; instead, there is persistent communication between them” [12]. Several sources believe spontaneous AVM to be secondary to atherosclerosis [2,5,8]. Morandi et al suggests that obesity and chronic increases in arterial pressure can promote development [5]. Yagi et al recognized that many cases were associated with a history of hypertension or disease processes related to hypertension [4]. Walker et al hypothesized that radiation may be a cause [13]. Our patient presented with a spontaneous AVM of STA without any history of trauma or recent manipulation, and she had no documented diagnosis of hypertension.
Clinically, AVM of STA can present with local pain, headache, painless swelling, pulsatile mass with increasing size, or tinnitus. A mass associated with palpable thrill on physical exam will also be present. The appreciated bruit and thrill will be absent when compressing the STA proximal to the mass [1,3–6]. Pulsatile tinnitus associated with a pulsatile mass is the most common sign. One reported case was asymptomatic aside from a small mass that had increased in size [4]. Another case manifested similar symptoms to a migraine, with pain, nausea, emesis, fever, and dizziness [14]. AVMs are thought to account for 2% of all cases of tinnitus [11]. One source stated that AVMs can be associated with purple or red birthmarks [15]. Complications of STA AVM include pain, ischemic necrosis or ulceration, and hemorrhage [2]. Differential diagnoses include epidermoid cyst, abscess, hematoma, inflammatory lesion, neoplasm, pseudo-aneurysm, true aneurysm, arterial occlusion, and dissection [8,11,16]. Our patient presented with discomfort over the left temporal area in addition to pulsatile tinnitus and a pulsatile mass that was tender to palpation on physical exam.
Intra-arterial angiography is the criterion standard imaging for diagnosis, and Doppler ultrasound, MRA, and CTA also are used [1,17,18]. Angiography can help guide surgical planning in regards to identifying inflow and outflow vessels, especially when the treatment is embolization [1]. Angiography also helps to exclude intracranial components [8]. Disadvantages of arterial angiography include complications with access. CTA and MRA have the advantages of being non-invasive and more accessible [16]. Kang et al noted that CT temporal bone has a higher sensitivity to middle-ear abnormalities, while MRA can help demonstrate neoplasm and vascular abnormalities in addition to soft tumor involvement related to temporomandibular joint dysfunction and parotid gland [17,18]. We performed a CTA (Figure 1), which noted an arteriovenous malformation nidus within the left temporal subcutaneous tissues with arterial feeders primarily from the left external carotid artery and draining veins.
Treatment options include surgical excision, ligation, sclero-therapy, and embolization [8] (Table 1). In surgical excision, complete resection of the nidus, in addition to ligation of the feeding arteries and draining veins, is vital and failure to do so will likely lead to recurrence [1,19]. One case report stated that for a scalp AVM located in the skin, embolization is the treatment of choice, while for an AVM located in the muscle, surgical excision is the treatment of choice [20]. An important advantage of surgical excision is recurrence prevention if a complete excision is performed [19].
Disadvantages to surgical excision include possibility of undesirable cosmesis at the incision site in addition to a higher chance of increased blood loss compared to other methods [12,13]. Ligation alone of the feeding artery and draining vein has been reported [12]. However, ligation is associated with an increased chance of recurrence [11]. Komatsu reported that total excision is more effective treatment than ligation and embolization [12]. Previously, surgical excision was regarded as the standard treatment, but embolization has now been shown to be safe and effective in some cases.
Endovascular therapy via transarterial, transvenous, and percutaneous access has been reported [1,21]. Walker et al describes a direct puncture technique that avoids navigating a catheter and guidewires, decreases operative time, decreases radiation exposure, decreases contrast load, and provides increased delivery of the chemical agent to the targeted area for embolization [13]. Access via carotid or femoral carries significant risks. Marcaccio et al reported that among those undergoing a trans-carotid approach vs trans-femoral approach for carotid artery stenosis, there is a reported risk of 2.9% and 2.3%, respectively, for stroke/death [22].
Endovascular techniques include sclerotherapy and embolization utilizing coils, balloons, glue, and various liquid agents. Li et al described using both sodium tetradecyl sulfate and absolute alcohol as sclerosing agents [8,23].
Yang et al described using a balloon to successfully occlude the AVM, but stressed the importance of occluding the feeding artery close to the vein [1]. Kominami et al described embolization utilizing glue, without recurrence [24]. Glue agents include N-butyl-2-cyanoacrylate (NBCA) [13]. Liquid embolic agents include Onyx, ethylene vinyl alcohol copolymer (SQUID), and hydrophobic injectable liquid (PHIL). Onyx was the first copolymer-based embolic agent used, allowing for extensive knowledge of its use. However, disadvantages include transient loss of visualization over long periods of time and imaging artifacts. SQUID and PHIL are newer agents, with advantages including lower viscosity, improved visualization, and fewer artifacts on imaging [14,25,26]. Juan-Carepena et al described utilizing PHIL, which reduces imaging artifacts and does not cause discoloration when injected into the STA AVM, given the superficial nature [2].
Particulate embolic agents include polyvinyl alcohol (PVA) [14,25,26]. Contrast agent can also be used in conjunction with embolic agents to help visualization such as lipiodol, a radioactive substance made from poppy seed oil [14,17]. Gelfoam pieces have been used, but this treatment was unsuccessful in 2 out of 3 cases, and the patients subsequently underwent surgical excision [27].
One report discussed utilizing the rim of a sterile denture cup to compress the arterial inflow and venous outflow for 5 min during percutaneous access and injection of 3% Sotradecol, a sclerosing agent, in combination with contrast material and Avitene, a hemostatic agent [23].
An advantage to endovascular therapy is that it has both diagnostic and therapeutic efficacy, and can also result in desirable cosmesis outcomes [1]. Disadvantages include incomplete embolization resulting in recurrence, undesirable skin pigmentation from utilized agents, overlying skin necrosis from chemical agent, systemic migration, and rare cardiopulmonary collapse secondary to intravascular injection of ethanol [8,21,23]. Embolization alone achieves complete closure in only 65% of patients [2]. Embolization has been used alone or with surgical excision to decrease intraoperative bleeding [21].
Komatsu et al reported that surgical excision is more successful than ligation and embolization in terms of recurrence [12]. In our case, the patient underwent open excision under general anesthesia with additional local anesthesia, without recurrence, and had complete resolution of symptoms at the 11-month follow-up appointment.
Conclusions
Spontaneous AVMs of the STA are exceedingly rare and the etiology remains controversial. A thorough clinical history and physical exam remain paramount to correct diagnosis. Intra-arterial angiography remains the criterion standard for imaging. However, additional imaging modalities include ultrasound, MRA, and CTA. Treatment options include surgical excision, ligation, sclerotherapy, and embolization with coils, glue, balloons, or chemical solution. Our institution prefers complete surgical excision of STA AVM, as it carries less risk of complications, including stroke and death, and surgical excision seems to be superior, with lower recurrence rates than other treatment options.
Figures
References:
1.. Yang M, Pan L, Cai MJ, Spontaneous arteriovenous fistula of the superficial temporal artery: Diagnosis and treatment: Clin Neurol Neurosurg, 2014; 123; 18-24
2.. Juan-Carpena G, Palazón-Cabanes JC, Gallego-León JI, Niveiro M, Betlloch-Más I, Spontaneous arteriovenous fistula of the superficial temporal artery misdiagnosed as hemangioma: Dermatol Ther, 2021; 34(1); e14723
3.. Li D, Heiferman DM, Rothstein BD, Scalp Arteriovenous malformation (cirsoid aneurysm) in adolescence: Report of 2 cases and review of the literature: World Neurosurg, 2018; 116; e1042-e46
4.. Yagi S, Saijo Y, Matsuda T, Mass on the head: Spontaneous arteriovenous fistula of the superficial temporal artery: J Med Invest, 2019; 66(1.2); 209-10
5.. Morandi X, Godey B, Riffaud L, Brassier G, Nontraumatic arteriovenous fistula of the superficial temporal artery: Otolaryngol Head Neck Surg, 2001; 124(5); 588-89
6.. Janssen M, Vaninbroukx J, Fourneau I, Arteriovenous fistula after superficial temporal artery biopsy: Ann Vasc Surg, 2013; 27(4); 500 e1–5
7.. Fisher-Jeffes ND, Domingo Z, Madden M, de Villiers JC, Arteriovenous malformations of the scalp: Neurosurgery, 1995; 36(4); 656-60 ; discussion 660
8.. Li F, Zhu S, Liu Y, Traumatic arteriovenous fistula of the superficial temporal artery: J Clin Neurosci, 2007; 14(6); 595-600
9.. Tisetso Morare NM, Baloyi ERJ, Post-traumatic arteriovenous malformation of the superficial temporal artery: J Vasc Surg Cases Innov Tech, 2020; 6(1); 50-54
10.. Matsushige T, Kiya K, Satoh H, Arteriovenous malformation of the scalp: Case report and review of the literature: Surg Neurol, 2004; 62(3); 253-59
11.. Selleck AM, O’Connell B, Patel S, Clark JM, Intraparotid superficial temporal artery arteriovenous malformation causing persistent pulsatile tinnitus: Otol Neurotol, 2020; 41(7); e873-e75
12.. Komatsu Y, Narushima K, Kobayashi E, Congenital arteriovenous malformation of the scalp – case report: Neurol Med Chir (Tokyo), 1989; 29(3); 230-34
13.. Walker GB, Wang AP, Hadwen J, Direct puncture of the superficial temporal artery in embolization of a scalp arteriovenous fistula: A case report: Neurointervention, 2023; 18(1); 67-71
14.. Kim DM, Benndorf G, Von Moers A, Spontaneous scalp arteriovenous fistula in a child with hartnup disease: J Endovasc Ther, 2004; 11(3); 348-50
15.. Khodadad G, Arteriovenous malformations of the scalp: Ann Surg, 1973; 177(1); 79-85
16.. Daronch OT, Bragato PH, Ferreira LFT, Traumatic arteriovenous fistula in the temporal region: A therapeutic challenge: J Vasc Bras, 2021; 20; e20200055
17.. Chen MC, Chung WY, Luo CB, Wu HM, Arteriovenous malformation in the parotid region presenting as pulsatile tinnitus: A case report: Head Neck, 2010; 32(2); 262-67
18.. Kang M, Escott E, Imaging of tinnitus: Otolaryngol Clin North Am, 2008; 41(1); 179-93
19.. Kohout MP, Hansen M, Pribaz JJ, Mulliken JB, Arteriovenous malformations of the head and neck: natural history and management: Plast Reconstr Surg, 1998; 102(3); 643-54
20.. Nishimura T, Kubota S, [A case of congenital AVM in temporoparietal muscle.]: No Shinkei Geka, 1996; 24(3); 277-80 [in Japanese]
21.. Youn SW, Lee NJ, Suh SI, Kang SH, Direct-puncture embolization of scalp arteriovenous fistulae: Neurol Med Chir (Tokyo), 2012; 52(7); 525-28
22.. Marcaccio CL, Anjorin A, Patel PB, In-hospital outcomes after upper extremity versus transfemoral and transcarotid access for carotid stenting in the Vascular Quality Initiative: J Vasc Surg, 2022; 76(6); 1603-1614 e7
23.. Hendrix LE, Meyer GA, Erickson SJ, Cirsoid aneurysm treatment by percutaneous injection of sodium tetradecyl sulfate: Surg Neurol, 1996; 46(6); 557-60 ; discussion 560–61
24.. Kominami S, Watanabe A, Akimoto M, Superficial temporal arteriovenous fistula as a complication of rhytidectomy: J Craniofac Surg, 2012; 23(2); 603-5
25.. Labropoulos N, Meisner RJ, Gasparis A, Tassiopoulos AK, Management of non-giant cell arteritis disease of the superficial temporal artery: J Vasc Surg, 2011; 53(1); 200-3
26.. Vollherbst DF, Chapot R, Bendszus M, Möhlenbruch MA, Glue, onyx, squid or PHIL? Liquid embolic agents for the embolization of cerebral arteriovenous malformations and dural arteriovenous fistulas: Clin Neuroradiol, 2022; 32(1); 25-38
27.. Shimoda M, Matumae M, Shibuya N, [Three cases of scalp arteriovenous malformations.]: No Shinkei Geka, 1987; 15(2); 173-78 [in Japanese]
28.. Cross FS, Glover DM, Simeone FA, Oldenburg FA, Congenital arteriovenous aneurysms: Ann Surg, 1958; 148(4); 649-63 ; discussion 663–65
29.. Mohanty S, Rao CJ, A large cirsoid aneurysm of the scalp associated with epilepsy: J Neurol Neurosurg Psychiatry, 1976; 39(9); 835-36
30.. Kaufman SL, Kumar AA, Roland JM, Transcatheter embolization in the management of congenital arteriovenous malformations: Radiology, 1980; 137(1 Pt 1); 21-29
31.. Takahashi N, Kikuchi H, Karasawa J, [Embolization and detached balloon occlusion by the femoral route in craniofacial lesions.]: No Shinkei Geka, 1983; 11(6); 591-602 [in Japanese]
32.. Kuroki K, Taguchi H, Sumida M, [A case of hemorrhagic non traumatic arteriovenous fistula of the scalp.]: No Shinkei Geka, 1999; 27(9); 851-53 [in Japanese]
Figures
Tables
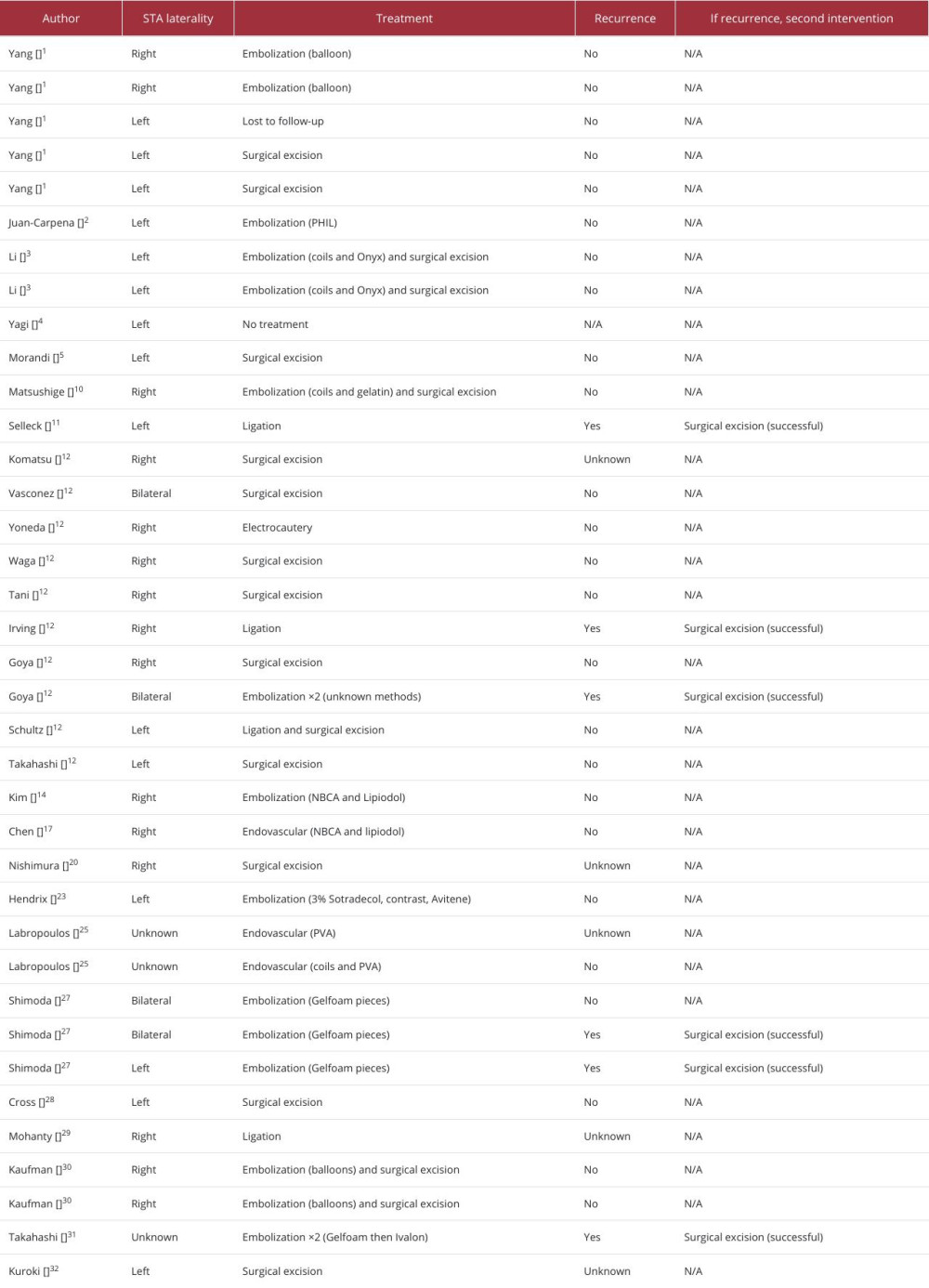 Table 1.. Summary of 37 spontaneous superficial temporal artery arteriovenous malformations including laterality, treatment, recurrence at follow-up, and additional intervention if recurrence occurred.
Table 1.. Summary of 37 spontaneous superficial temporal artery arteriovenous malformations including laterality, treatment, recurrence at follow-up, and additional intervention if recurrence occurred.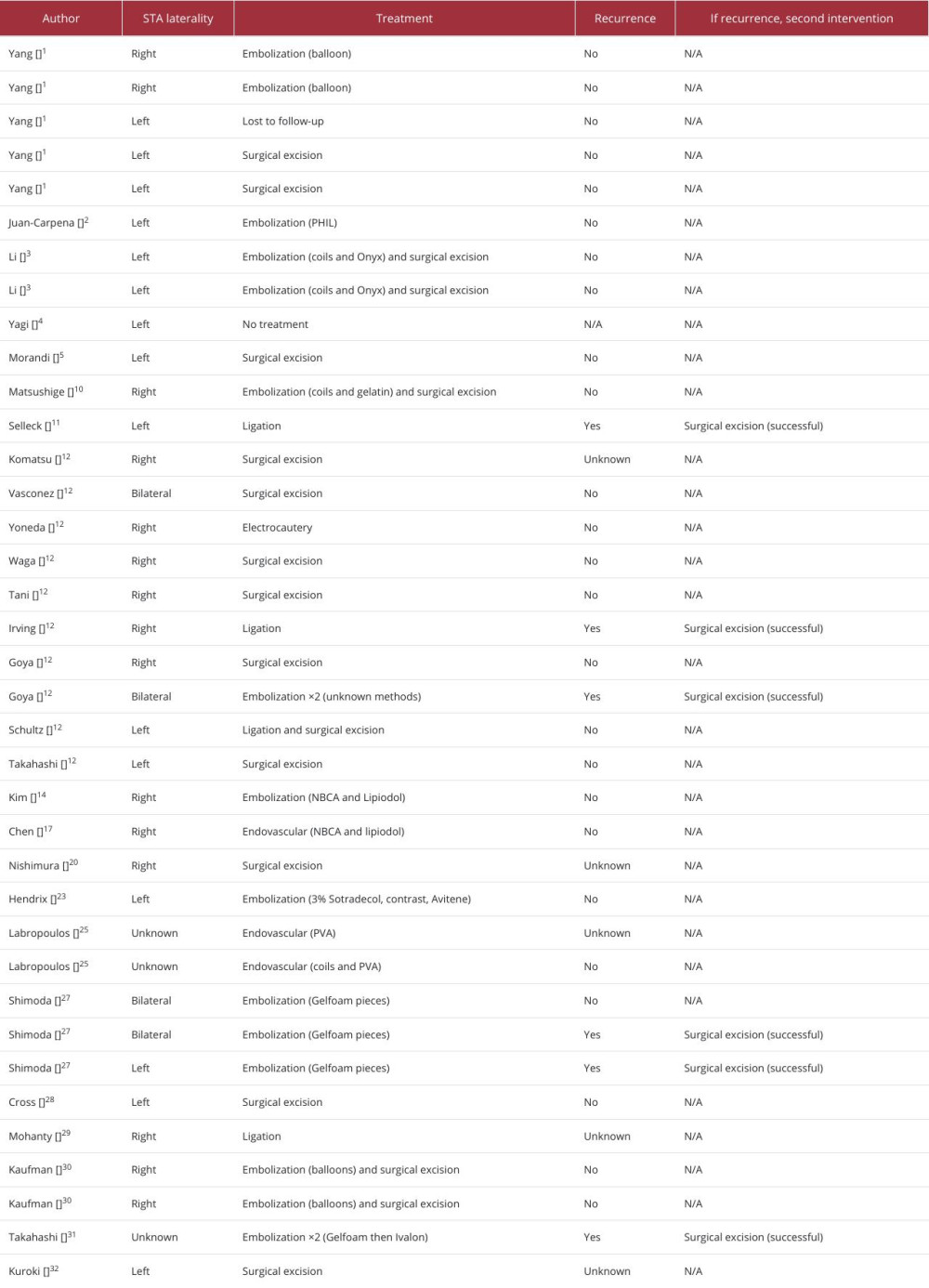 Table 1.. Summary of 37 spontaneous superficial temporal artery arteriovenous malformations including laterality, treatment, recurrence at follow-up, and additional intervention if recurrence occurred.
Table 1.. Summary of 37 spontaneous superficial temporal artery arteriovenous malformations including laterality, treatment, recurrence at follow-up, and additional intervention if recurrence occurred. In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








