26 July 2020: Articles 
Histopathological Features of Deep Soft Tissue Epithelioid Angiosarcoma in the Lower Extremity: A Rare Case Report
Rare disease
Pham Nguyen Cuong1ABCDEF, Nguyen Thanh Xuan2ABCDEF*, Pham Nhu Huy3F, Tran Nhu Tung4B, Nguyen Huu Son5DDOI: 10.12659/AJCR.923933
Am J Case Rep 2020; 21:e923933
Abstract
BACKGROUND: Epithelioid angiosarcoma is an extremely rare malignant disease of the endothelial cells. Most of the previous reports about this disease were regarding clinical features and radiological findings, with limited descriptions of pathological diagnosis. This report aimed to present a reference to increase understanding of the timely diagnosis of epithelioid angiosarcoma.
CASE REPORT: A 65-year-old male was diagnosed with epithelioid angiosarcoma originating from the deep soft tissue of the lower leg. He had a history of 2 months of rapid swelling and painful in the left lower leg, which occurred after a muscle cramp, and was clinically suspicioius for hematoma. Radiological examination revealed a large heterogeneous soft-tissue mass. Histopathology results showed that the mass was malignant, and the differential diagnosis wasa malignant vascular tumor, melanoma, poorly differentiated carcinoma, clear cell sarcoma, epithelioid sarcoma, and anaplastic large-cell lymphoma. Immunohistochemistry findings confirmed that it was an epithelioid angiosarcoma.
CONCLUSIONS: This case underscores the difficult of diagnosing epithelioid angiosarcoma. It requires careful pathological investigation and immunophenotype labeling.
Keywords: Extremities, Immunohistochemistry, Pathology, Sarcoma, Soft Tissue Neoplasms, Hemangioendothelioma, Epithelioid, Lower Extremity, Rare Diseases
Background
Angiosarcomas are rare malignancies of the endothelial cell. They generally account for fewer than 1% of all soft-tissue sarcomas, and just 10% of all angiosarcomas arise in deep soft tissues. They usually occur at the site of local and/or distant metastasis, and the lungs are the most frequent site for metastases. Often, the prognosis for patients with angiosarcomas is poor [1,2]. There are three subtypes of angiosarcomas: categorized as visceral (occurring in body organs), cutaneous, and soft tissue. They are histologically classified based on their differentiation in forms such as endothelial cell atypia or high-grade spindle malignant cells. Tumors with malignant endothelial cells are defined as epithelioid angiosarcoma (EA) due to their predominantly (or specifically) epithelioid appearance [3,4]. EA frequently arises in the soft tissues of the extremities (mainly intramuscular), but other sites with EA are also often seen, such as skin, bone, thyroid gland, or adrenal glands. They are more common in older patients, with a median age ranging from 60 to 71 years [1,5,6]. EA diagnosis is a challenge because it is usually mistaken for other injuries such as epithelioid hemangioendothelioma, epithelioid hemangioma, metastatic carcinoma, metastatic melanoma, epithelioid sarcoma, lymphoma, and others sarcomas with epithelioid features [7].
The purpose of this report, therefore, was to examine EA, a rare disease that is diagnosed and treated in our hospital, and to present a reference to increase understanding of the timely diagnosis of epithelioid angiosarcoma.
Case Report
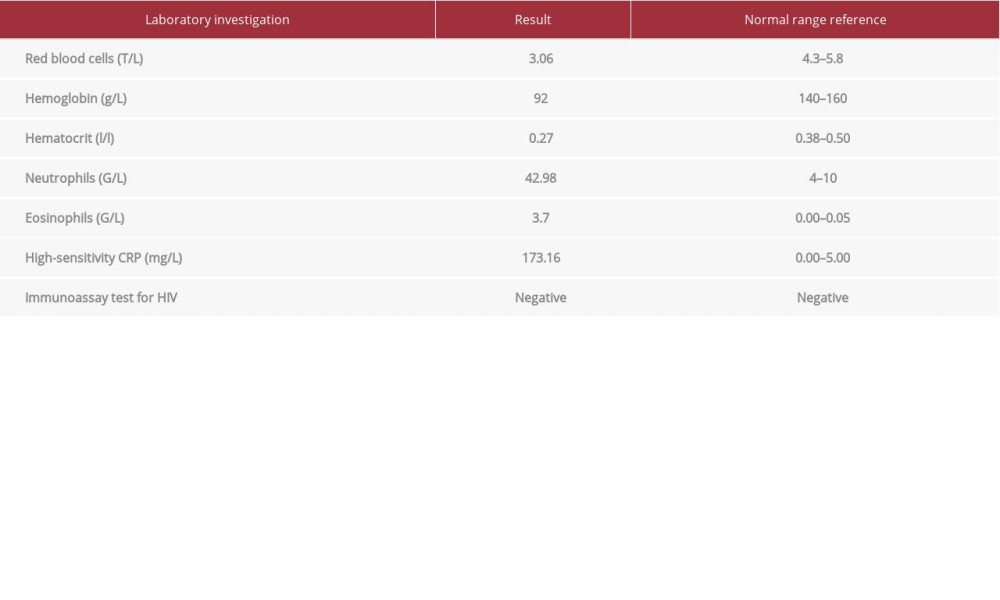
A 65-year-old male patient was admitted to our hospital. He had a 2-month history of rapid swelling and painful in the left lower leg, which started after a muscle cramp and was clinically suspicious for hematoma. Table 1 shows the nonspecific changes in laboratory findings for this patient, such as anemia and increase in high-sensitivity C-reactive protein.
An ultrasound of the left calf muscles showed a mixed hyper-echoic and hypoechoic, ill-defined area measuing 13×7×12 (cm). There were components with liquid-density, posterior enhancement, non-vascular color Doppler signals, and infiltration of the surrounding area.
Computed tomography (CT) scan revealed a 14×10×6-cm mass on the back of the left leg, with a fluid-density component and soft tissue. This mass changed the normal anatomical structure of muscle bundles and the inside of it was mostly solid, enhanced, and hypervascular (Figure 1).
All preoperative findings (clinics, laboratory, imaging) suggested a diagnosis of hematoma.
Based on the multidisciplinary tumor board’s recommendation, surgery was performed several days later. Small samples were taken of irregular, soft, gray-white material mixed with hemorrhagic, necrotic areas.
Microscopically, Hematoxylin-Eosin-stained sections demonstrated large epithelioid cells with a round or polygonal shape and nuclei containing prominent nucleoli in central to eccentrical sites. The chromatin was peripherally marginated within the nucleus. Architecturally, the cells were primarily arranged in sheets. Mitotic figures, including abnormal mitoses, were frequently seen (Figure 2).
Immunohistochemical staining was analyzed in the standard Envision method. Malignant cells were found to be focally positive for S100, CKAE1/AE3, CD34, and Ki67 (50%); diffusely positive for CD31, Factor VIII, Vimentin; and negative for HMB45, Melan A, LCA, ALK, SMA, EMA, CD30 (Figure 3).
The histological findings and immunohistochemical results confirmed the diagnosis as epithelial angiosarcoma.
Discussion
EA is a rare form of angiosarcoma, characterized by large cells with an epithelioid appearance. It is a poorly differentiated malignancy and described by aggressive biological behavior [8].
Diagnosing epithelioid angiosarcoma remains difficult because it is so rare and can be confused with epithelioid hemangioendothelioma, epithelioid hemangioma, metastatic carcinoma, metastatic melanoma, epithelioid sarcoma, lymphoma, and many sarcomas with epithelioid features [7]. The clinical features, prognosis, and immunohistochemistry of this lesion have not yet been clearly elucidated [9].
Clinically, EA originates in endothelial cells, therefore, it can develop in any part of the body and affect patients at all ages [10]. However, EA occurs more frequently in older patients, at a median age from 61 to 71 years, and predominantly in males [11,12]. EA usually presents as a rapidly growing mass that is palpable when in an extremity. Patients may have pain or discomfort related to mass effect. Without treatment, the tumor might rapidly grow to over 20 cm. Some symptoms, such as hemorrhage, local ulceration, and focal edema, can present when the tumor size increases [1]. The etiology of EA reaminsl unknown. However, specific risk factors have been identified, such as previous irradiation, arteriovenous fistulae, toxic chemical exposure, and chronic lymphedema [13].
On imaging, the soft tissue of EA may appear as an irregular soft tissue mass with enhancement on contrast-enhanced CT. In more advanced cases, invasion of underlying bone or nearby solid organs can occur. Also, calcification of soft tissue can be seen [1].
Macroscopically, gross findings from EA are very similar to those of typical angiosarcomas. They tend to be hemorrhagic, porous masses, because of their inherent vascular nature, with a cut surface that is grey-white or grey-red. The lesions often have an indistinct margin and extend beyond the obvious gross confines of these margins. That makes it difficult for the surgeon to ensure a total resection [7].
Microscopically, distinguishing between EA and other epithelial tumors in diagnosis is challenging. Histologically, EA sometimes is misdiagnosed as metastasis carcinoma [7]. Identificatoin of occasional cells with erythrocytes in intracytoplasmic lumina can lead to diagnosis of EA. Architecturally, EA cells most commonly are arranged mainly in sheets, following by cords or cellular islands [7,13].
In immunohistochemical analysis, the epithelioid variant, which highly positive for Vimentin, is the most common form of EA. It always stains positive for Factor VIII. In most cases, CD31 is weakly positive, largely due to the high sensitivity of this marker. Approximately 40% to 100% of cases of EA are positive for CD34, and it may tend to stain in areas with vessel formation, which is easy to see. Thus, it is limited with the lesions of utility in sheet and poor differentiation. CKAE1/AE3 stains are counted for over 35 percent of angiosarcomas, have the range of positivity from 78 to 100% in fewer studies, particularly the exploration of the epithelioid cell variants [8]. Malignant epithelial cells in EA are usually negative for synaptophysin, S-100, EMA, CEA, CD20, and HMB4 [4,7,14].
In our case, clinical features and histopathological findings were consistent with the diagnostic criteria for EA. The differential diagnosis also was quite diverse. As we mentioned earlier, the histological features of EA are often nonspecific and difficult to directly confirm via microscopic evaluation on Hematoxylin-eosin staining sections. It is easily misdiagnosed as carcinoma or other tumors with an epithelial appearance, such as melanoma, clear cell sarcoma, poorly differentiated carcinoma, epithelioid sarcoma, and anaplastic large-cell lymphoma. On immunohisto-chemical analysis, positivity for an endothelial marker (CD31, CD34, Factor VIII), Vimentin, and EMA negativity help to differentiate EA from poorly differentiated carcinoma and epithelioid sarcoma. Its negativity for S-100, HMB-45, and Melan-A helps to exclude clear cell sarcoma and melanoma. Because cytokeratins are positive in about one-third of cases of soft tissue angiosarcoma, and particularly with EA, they cytokeratins cannot be used to accurately differentiate between EA and poorly differentiated carcinoma. When tumor cells are negative for LCA, SMA, ALK, and CD30, the other possibilities also are excluded [6,7,15]. In the case of malignant vascular tumors, we excluded the diagnosis as epithelioid hemangioendothelioma because of the lower levels of atypical cells in EA.
Treatments for EA include complete surgical resection of the tumor, chemotherapy, and radiation therapy [16–18]. Approximately 50% of patients die due to the disease within 2 to 3 years after being diagnosed; nevertheless, in 20% to 30% of patients, the outcome is excellent [6,16].
Regarding prognosis of EA, metastasis to lymph nodes as well as other organs such as the lungs, bones, soft tissue, and skin can be seen, while the lungs are the only site of metastasis for most other malignant soft tissue tumors [4,6]. In our case, Ki-67 was showed about 50% positivity. According to one report, staining for Ki-67 with MIB--1 was seen in 10% of patients and over 72% of all subtypes of angiosarcomas studied, indicating that these malignancies have a highly proliferative nature. About 83% of patients with a high proliferative index (MIB-1 >10%) eventually died, while 67% of those with low growth index (MIB-1 <10%) may have been cured, so increased tumoral proliferation is adversely associated with prognosis [4].
Conclusions
EA in deep soft tissue is a rare histopathological form of angiosarcoma in particular and of soft tissue sarcoma in general. A combination of clinical characteristics, radiological findings, histopathology, and especially immunohistochemistry features is essential to quickly and accurately diagnosis this rare tumor.
Figures
References:
1.. Gaballah AH, Jensen CT, Palmquist S, Angiosarcoma: Clinical and imaging features from head to toe: Br J Radiol, 2017; 90; 20170039
2.. Pandey M, Sutton GR, Giri S, Martin MG, Grade and prognosis in localized primary angiosarcoma: Clin Breast Cancer, 2015; 15; 266-69
3.. Antonescu C, Malignant vascular tumors – an update: Mod Pathol, 2014; 27(Suppl. 1); S30-38
4.. Hart J, Mandavilli S, Epithelioid angiosarcoma: A brief diagnostic review and differential diagnosis: Arch Pathol Lab Med, 2011; 135; 268-72
5.. Fletcher CD, Beham A, Bekir S, Epithelioid angiosarcoma of deep soft tissue: A distinctive tumor readily mistaken for an epithelial neoplasm: Am J Surg Pathol, 1991; 15; 915-24
6.. Meis-Kindblom JM, Kindblom LG, Angiosarcoma of soft tissue: A study of 80 cases: Am J Surg Pathol, 1998; 22; 683-97
7.. Wu J, Li X, Liu X, Epithelioid angiosarcoma: A clinicopathological study of 16 Chinese cases: Int J Clin Exp Pathol, 2015; 8; 3901-9
8.. Sakamoto A, Takahashi Y, Oda Y, Iwamoto Y, Aggressive clinical course of epithelioid angiosarcoma in the femur: A case report: World J Surg Oncol, 2014; 12; 281
9.. Young RJ, Brown NJ, Reed MW, Angiosarcoma: Lancet Oncol, 2010; 11; 983-91
10.. Chang JH, Kim JH, Hong SH, Angiosarcoma presenting with spontaneous hydropneumothorax: Report of a case and review of the literature: Open Respir Med J, 2014; 8; 48-54
11.. Lahat G, Dhuka AR, Hallevi H, Angiosarcoma: Clinical and molecular insights: Ann Surg, 2010; 251; 1098-106
12.. Liu H, Huang X, Chen H, Epithelioid angiosarcoma of the kidney: A case report and literature review: Oncol Lett, 2014; 8; 1155-58
13.. Jagtap SV, Kumar S, Kulkarni SR, Jagtap SS, Angiosarcoma of deep soft tissue presented as mass lower leg: Int J Health Sci, 2014; 4; 274-77
14.. Long M, Shali W, Huang Q, Epithelioid angiosarcoma of the liver: Report of two cases and review of the literature: Int J Clin Exp Pathol, 2018; 11; 3191-98
15.. Branch K, Smith M, Epithelioid angiosarcoma: A case review: Path Case Rev, 2008; 13; 264-68
16.. Deshpande V, Rosenberg AE, O’Connell JX, Nielsen GP, Epithelioid angiosarcoma of the bone: A series of 10 cases: Am J Surg Pathol, 2003; 27; 709-16
17.. Goldblum JR, Rice TW, Epithelioid angiosarcoma of the pulmonary artery: Hum Pathol, 1995; 26; 1275-77
18.. Lund L, Amre R, Epithelioid angiosarcoma involving the lungs: Arch Pathol Lab Med, 2005; 129; e7-10
Figures
In Press
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250