29 July 2020: Articles 
Use of a Titanium Cage and Intramedullary Nails to Treat Distal Femoral Fracture Nonunion in a Patient with Renal Osteopathy: A Case Report
Unusual clinical course, Challenging differential diagnosis, Unusual or unexpected effect of treatment, Diagnostic / therapeutic accidents
Hongyu Jin1ABCDEF, Maoqi Xiong2BCE, Hui Zhou3CD, Man Zhang4BCD, Xiao He2CDE, Dan Pu2AEG*DOI: 10.12659/AJCR.924565
Am J Case Rep 2020; 21:e924565
Abstract
BACKGROUND: Nonunion occurs to approximately 10% of people who suffer from distal femoral fracture, which can be induced by other diseases and medical interventions. CKD and subsequent renal osteopathy are regarded as risk factors for nonunion. Internal fixation is the most widely applied medical procedure to treat distal femoral fracture, the efficiency and stability of which are improved by emerging biological materials. Besides traditional screws and plate, titanium cages and intramedullary nails have been introduced lately to repair nonunion and large bone defects resulting from it, which is a huge challenge for orthopedic surgeons. To the best of our knowledge, this is the first report on a distal femoral fracture patient with renal osteopathy treated by internal fixation enhancement using a titanium cage and intramedullary nails.
CASE REPORT: We report the case of an 84-year-old Chinese woman with renal osteopathy who underwent 4 internal fixation operations to treat a distal femoral fracture. The first 3 surgeries used screws and a plate as internal fixation materials to treat the fracture and nonunion, but did not achieve satisfactory outcomes. In the final surgery, a titanium cage and intramedullary nail were used and the patient recovered soon.
CONCLUSIONS: Doctors should pay attention to patient’s primary health conditions, especially renal disorders, before performing surgeries for distal femoral fracture. It is important to select the most appropriate materials and choose the most suitable surgical method in patients with poor health conditions.
Keywords: Ambulatory Surgical Procedures, Fractures, Bone, Renal Insufficiency, Chronic, Aged, 80 and over, Femoral Fractures, Fracture Fixation, Intramedullary, Fractures, Ununited, Prostheses and Implants, Radiography, Reoperation, Titanium
Background
Nonunion commonly occurs in distal femur fractures, especially supracondylar regions, usually due to unsuccessful clinical interventions in distal femoral fractures [1,2]. About 0% to 10% of patients managed by intramedullary devices are likely to develop nonunion resulting from high- or low-energy injuries and this can occur in patients of all age groups [3,4]. Patients with femoral nonunion are faced with various lifelong problems, notably prolonged psychological and physical disorders, gait malfunction, and persistent disability [5]. To improve the quality of life in this population, many surgical methods have been introduced to treat distal femoral fracture, with internal fixation being the most widely applied [6,7]. Fortunately, a number of emerging high-standard materials are increasingly used in internal fixation to provide more satisfactory stability and efficiency. Several materials appear to improve union rates in patients with basic bony malformation and abnormalities, such as bone metabolism disturbance, osteogenesis difficulty, and osteoporosis.
Renal osteopathy is regarded as a major risk factor for bone metabolism disturbance. However, despite various choices of surgical methods and bone implants, continuous efficacy loss and substantial bone loss in metaphysis remains a challenge for orthopedists in cases with post-operative nonunion in distal femoral epicondylar fracture complicated with renal osteopathy.
In this case report, we described an 84-year-old woman suffering from poor health conditions, including renal osteopathy, who underwent 4 surgeries to heal a distal femoral fracture. The patient regained ambulation after the fourth surgery, in which a titanium cage and intramedullary nail were used instead of conventional screws and plate. We discuss the impact of renal osteopathy on fracture healing and present different methods used to treat distal femoral fracture. Finally, we assessed risk factors for nonunion.
Case Report
An 84-year-old Chinese woman with distal femoral fracture and nonunion was admitted to the Department of Orthopedics of West China Hospital for surgery in October 2016. From 2006 to 2016, the patient underwent 4 continuous operations to treat a distal femur fracture. The first operation was done when she was 76 years old, in which a typical internal fixation with dynamic condylar screw (DCS) was applied. However, due to the breaking of screws and the implants’ inefficacy driven by nonunion, a second and third operation were performed to replace previous internal fixation materials when she was 77 and 79 years old. Allograft and artificial bones were used to supplement bony loss during the second and third operations.
Figures 1–4 show X-rays taken when the initial fracture occurred and after the first, second, and third operations, respectively. Unfortunately, these operations were unable to successfully heal the fracture. Undergoing so many operations is difficult for elderly patients with poor basic health status.
Besides bony abnormalities, the patient also suffered from chronic renal failure, which we suspected was directly related to the lasting nonunion. Tables 1 and 2 show results of biochemical and urine tests, respectively, on admission to West China Hospital, demonstrating elevated typical urine protein, urine glucose, urea, creatinine, and serum cystatin C, which indicated intermediate stage chronic renal failure. In addition, osteomalacia was also suspected based on results of biochemical exams. The patient also had high serum glucose, urea, and creatinine and low total bilirubin, total protein, albumin, and A/G values. According to her medical history, the patient developed renal malfunction when she was 72, which was 2 years before the fracture. Additionally, we saw from the X-rays taken previously that the patient also developed severe osteoarthritis of the knee on the side of the supracondylar fracture, which is one of the most important risk factors for nonunion. We thus decided to prescribe anti-inflammatory drugs for 1–2 months to combat the osteoarthritis.
Moreover, 1.5 months before admission, the patient developed sudden dizziness followed by repeated bilateral tinnitus, photaesthesia, and numbness in limbs. The initial episode lasted for 10 min, and each subsequent episode was worse. Finally, the patient went to the Outpatient Department due to her unbearable symptoms. A neurology-specific physical examination found symmetrical round pupils, sensitive pupillary reflex, middle tongue protrusion, grade 5 muscle strength in upper limbs and right lower limb, negative pathological reflexes, and grade 1 muscle strength in the proximal left lower limb. Further imaging examinations showed low-density areas in the frontal corner of ventricles on both sides, which indicated cerebral infarction. Encephalatrophy was also noted on MRI and CT.
Ten days after re-admission to the Department of Orthopedics in West China Hospital 1.5 months later for treatment of osteoarthritis, a fourth operation was proposed. Since the second and third operations were not successful in the end, we used intramedullary nails combined with a titanium cage in the fourth internal fixation. In the operation, we successfully removed 9 screw and broken steel plates before implanting a 4-cm-long titanium cage with a diameter of 19 mm into the broken part in order to recover the limb force line, limb length, and axial stability. Subsequently, a 12.5×20 mm intramedullary nail was implanted into the place between the femoral inter-condylar fossa and posterior cruciate ligament (Figures 5, 6). Finally, 2 and 4 screw were implanted to the proximal and distal part, respectively, of the nail. Following this surgery, we filled the bone loss with a titanium cage and a quantity of allograft and artificial bones, which was proved effective according to the patient’s mobility and regional motion capacity.
The patient recovered well and quickly and was discharged from the Department of Orthopedics 2 weeks after the operation. We carried out a long-term follow-up of the patient by telephone call once a week and a home visit every 3 months. The patient lived in the Department of Rehabilitation for 1 month and she could walk with the help of a single walking stick when she was discharged. According to medical records, she practiced the regional muscle strength exercise of walking with sticks. She never became unable to walk after she went home. According to our follow-up, the patient had kept up the habit of walking with a stick for 1 h or more every day and never complained about pain or uneasiness. She also had a regular outpatient visit to solve the renal problems. It appears that this surgery allowed the patient to regain mobility, which greatly increased her quality of life.
Discussion
Internal fixation with DCS is a standard and proven effective therapy for treating distal femoral fracture. However, in some circumstances the traditional internal fixation therapy can be less effective and even lead to severe post-operation adverse effects, which can be devastating. In this case report, we described an elderly woman with several primary diseases, including renal osteopathy and cerebral infarction, who underwent 4 restoration operations to treat distal femoral fracture and eventually died of operation-related complications. Thus, to successfully manage such patients with poor basic health, especially with renal disfunction, we discussed the methods of treating nonunion, the impact of local osteoarthritis, the influence of renal osteopathy on fracture healing, and different treatment options for distal femoral fracture, especially the efficacy of a titanium cage for bone loss in fracture healing operations, and surgery choices in patients with poor basic health.
When a nonunion occurs, we must first define the risk factors, such as osteoporosis, metabolic diseases, and local inflammation. To avoid a nonunion, treating the primary diseases should be the priority before making a decision about surgery. Our patient had combined diseases (CKD and severe osteoarthritis), so we first took care of the 2 metabolic diseases and planned not to perform our surgery until the overall condition improved and local inflammation was controlled. With respect to methods of surgery, internal fixation definitely is the traditional and most widely known surgical method, as it provides satisfactory post-surgical stability. However, when the patient has an extreme loss of bone materials, internal fixation simply may not work. Therefore, emerging materials like intramedullary nails and titanium cages can be considered to better strengthen the bone. In addition, this patient was complicated with osteoarthritis in the previous several surgeries, which we thought might have contributed to the nonunion. Osteoarthritis is characterized by an abnormally high accumulation of inflammatory molecules around the bone, with concomitant sclerotin loss. Thus, this condition complicates post-surgical rehabilitation. We thought the best way to avoid nonunion is to improve the quality of surgery and try to increase the amount of sclerotin simultaneously.
Renal osteopathy is an important complication of CKD, which can increase fracture risk and induce post-operative nonunion [8,9]. Renal osteopathy can interfere with the metabolism of calcium, phosphorus, parathyroid hormone (PTH), and vitamin D, thus causing subsequent abnormalities in bone transformation, bone mineralization, bone quantity, and bone density [10]. Serum concentrations of these substances and the consequent clinical symptoms change with the periods of CKD [11]. Kim et al. and Babayev et al. discovered a 2–14 times higher fracture risk and nonunion rate in renal osteopathy patients with grade 3-5 CKD [12,13], which could be attributed to decreasing bone density induced by increasing bone transformation and bone cortex perforation rates [14]. According to pathology, the priority to treat biochemical disorders in renal osteopathy is to maintain normal calcium and phosphorus concentrations, control secondary progressive hyperparathyroidism, and alleviate osteoporosis [15]. Following this principle, controlling hypocalcemia and hyperphosphatemia is essential, which can be achieved by either using activated vitamin D or inhibiting PTH secretion. Because the stage of CDK has great influence on prognosis, specific pathophysiological process and clinical characteristics need to be investigated further. Additionally, corresponding medications for different stages should also be researched.
In our case, besides rather poor basic health conditions, the primary surgical option is also an important factor for the patient’s poor prognosis. In our case, the first 2 surgeries the patient underwent were applied in almost the same module, by using DCS to perform an internal fixation, which had not been able to provide a satisfactory outcome. According to X-rays, the first operation had not provided adequate fixation and reduction as well as the stability of the fracture end. Meanwhile, complicated obesity and renal osteopathy had added to the risk of nonunion. Therefore, it is essential to review the materials to perform internal fixation since only when titanium cage and intramedullary nails were implanted, the patient gradually regained good ambulation. In addition, a cage can be a satisfactory choice to restore the limb length in patients with massive bone loss after repeated surgical failures. So far, a quantity of surgical selections has been recommended for distal femoral fracture. Chi-Chuan Wu helped 7 out of 8 distal femoral fracture patients recover from nonunion by using static locked nails and corticocancellous bone grafting [16]. In other research, 18 out of 20 elderly patients with osteoporosis were healed from nonunion by modified retrograde-locked nailing [17]. Volker Alt et al. applied recombinant human bone morphogenetic protein-2 (rhBMP-2) loaded on an absorbable collagen sponge to distal femoral nonunion sites, which helped the patient regain ambulation [18]. For patients with poor health and primary diseases, reducing the number of surgeries and providing the best surgical option is mandatory. It is also important to select a surgical method that can lead to satisfactory and quick recovery. For our patient, we supposed the external fixation with violin method could promote better recovery.
In this patient, we found a severe loss of bone tissue, suggesting that replacing the screws or plate would not heal the non-union. Titanium cages have long been employed in repairing skull fractures, especially the orbits and basis cranii, which can treat fractures and nonunion with a great deal of bone loss. Thus, we coupled titanium cage and intramedullary nails in replacement of screws and plate for internal fixation to supplement potential spaces created by bone loss. In distal femoral fracture patients with osteoporosis, the titanium cage acts like mesh which combines once-separated bony fragments so that the density and stability increase. Therefore, we recommend use of a titanium cage with intramedullary nails for fracture healing in patients with osteoporosis. However, there are also some disadvantages of this surgical method. Most importantly, this surgery using intramedullary nails and a titanium cage is generally a much more complicated surgery compared with simple internal fixation, and the risks are therefore higher.
Clinically, it is important to be aware of risk factors which can potentially contribute to femoral nonunion after distal femoral fracture. Taitman et al. found that major risk factors were fracture type (open or closed), tobacco smoking, and delay to weight bearing [19]. Lynch et al. found that risk factors of nonunion included avascularity resulting from excessive surgical stripping, aggressive reaming, open fracture, infection, and bone loss resulting from osteoporosis or other reasons [5]. McKee et al. also found a correlation between the use of NSAIDS, medical comorbidities, and nonunion [20].
The patient we described also reminded us to carefully select surgical methods in patients complicated by underlying diseases which could interfere with substances metabolism and osteogenesis equilibrium. In patients with diseases that can decrease osteogenesis and increase bone metabolism, we should be aware of potential osteoporosis, which can induce chronic nonunion.
Conclusions
In this report we described a distal femoral fracture patient with poor health and renal osteopathy who had not benefited from 2 screw and plate replacements. We analyzed therapeutic strategies to treat renal osteopathy before the operation and reviewed different surgical methods for distal femoral fracture. We also introduced the use of titanium cages and intramedullary nails in patients with osteoporosis. Finally, we reviewed the risk factors for femoral nonunion to put more emphasis on the patient’s basic conditions.
Figures
References:
1.. Koval KJ, Seligson D, Rosen H, Fee K, Distal femoral nonunion: Treatment with a retrograde inserted locked intramedullary nail: J Orthop Trauma, 1995; 9(4); 285-91
2.. Chapman MW, Finkemeier CG, Treatment of supracondylar nonunions of the femur with plate fixation and bone graft: J Bone Joint Surg Am, 1999; 81(9); 1217-28
3.. Horwitz DS, Kubiak EN, Surgical treatment of osteoporotic fractures about the knee: J Bone Joint Surg Am, 2009; 91(12); 2970-82
4.. , Nonunion following intramedullary nailing of the femur with and without reaming. Results of a multicenter randomized clinical trial: J Bone Joint Surg Am, 2003; 85-A(11); 2093-96
5.. Lynch JR, Taitsman LA, Barei DP, Nork SE, Femoral nonunion: Risk factors and treatment options: J Am Acad Orthop Surg, 2008; 16(2); 88-97
6.. Thomson AB, Driver R, Kregor PJ, Obremskey WT, Long-term functional outcomes after intra-articular distal femur fractures: ORIF versus retrograde intramedullary nailing: Orthopedics, 2008; 31(8); 748-50
7.. Lujan TJ, Henderson CE, Madey SM, Locked plating of distal femur fractures leads to inconsistent and asymmetric callus formation: J Orthop Trauma, 2010; 24(3); 156-62
8.. Kurajoh M, Inaba M, Nagata Y, Association of cystatin C- and creati-nine-based eGFR with osteoporotic fracture in Japanese postmenopausal women with osteoporosis: Sarcopenia as risk for fracture: J Bone Miner Metab, 2019; 37(2); 282-91
9.. Blaslov K, Katalinic L, Kes P, What is the impact of immunosuppressive treatment on the post-transplant renal osteopathy?: Int Urol Nephrol, 2014; 46(5); 1019-24
10.. Ayme S, Bockenhauer D, Day S, Common elements in rare kidney diseases: Conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference: Kidney Int, 2017; 92; 796-808
11.. Biggar PH, Liangos O, Fey H, Vitamin D, chronic kidney disease and survival: A pluripotent hormone or just another bone drug?: Pediatr Nephrol, 2011; 26(1); 7-18
12.. Babayev R, Nickolas TL, Bone disorders in chronic kidney disease: An update in diagnosis and management: Semin Dial, 2015; 28(6); 645-53
13.. Kim SM, Long J, Montez-Rath M, Hip fracture in patients with non-dialysis-requiring chronic kidney disease: J Bone Miner Res, 2016; 31(10); 1803-9
14.. Malluche HH, Mawad HW, Monier-Faugere MC, Renal osteodystrophy in the first decade of the new millennium: Analysis of 630 bone biopsies in black and white patients: J Bone Miner Res, 2011; 26(6); 1368-76
15.. Zura R, Mehta S, Della Rocca GJ, Steen RG, Biological risk factors for non-union of bone fracture: JBJS Rev, 2016; 4(1); 01874474-201601000-00005
16.. Wu CC, Treatment of femoral shaft aseptic nonunion associated with plating failure: Emphasis on the situation of screw breakage: J Trauma, 2001; 51(4); 710-13
17.. Wu CC, Modified retrograde-locked nailing for aseptic femoral supracondylar nonunion with severe osteoporosis in elderly patients: J Trauma, 2011; 71(2); E26-30
18.. Alt V, Meyer C, Litzlbauer HD, Schnettler R, Treatment of a double nonunion of the femur by rhBMP-2: J Orthop Trauma, 2007; 21(10); 734-37
19.. Taitsman LA, Lynch JR, Agel J, Risk factors for femoral nonunion after femoral shaft fracture: J Trauma, 2009; 67(6); 1389-92
20.. McKee MD, DiPasquale DJ, Wild LM, The effect of smoking on clinical outcome and complication rates following Ilizarov reconstruction: J Orthop Trauma, 2003; 17(10); 663-67
Figures
Tables
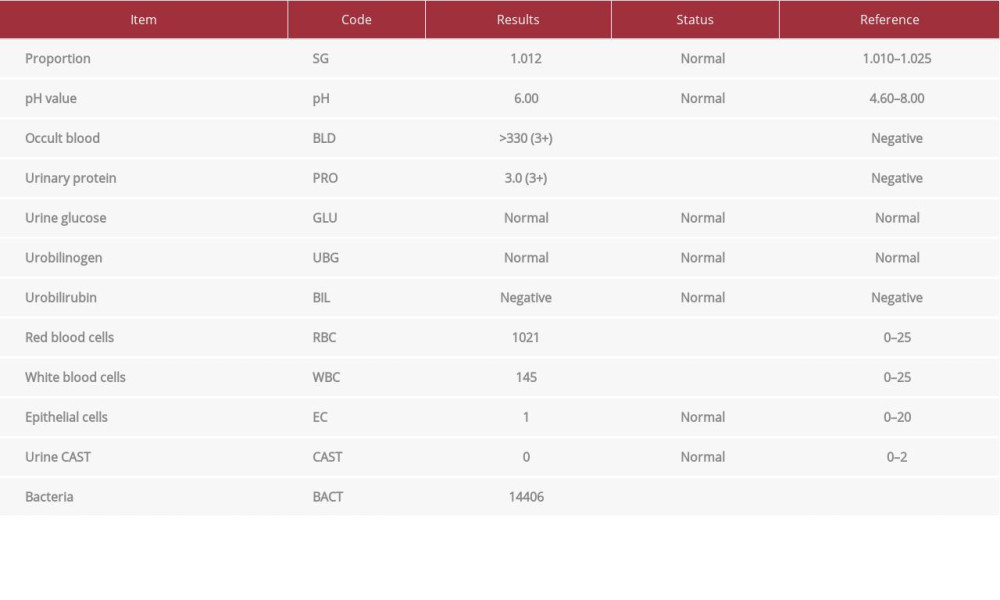 Table 1.. Results of urine tests on admission to West China Hospital (some items are not shown).
Table 1.. Results of urine tests on admission to West China Hospital (some items are not shown).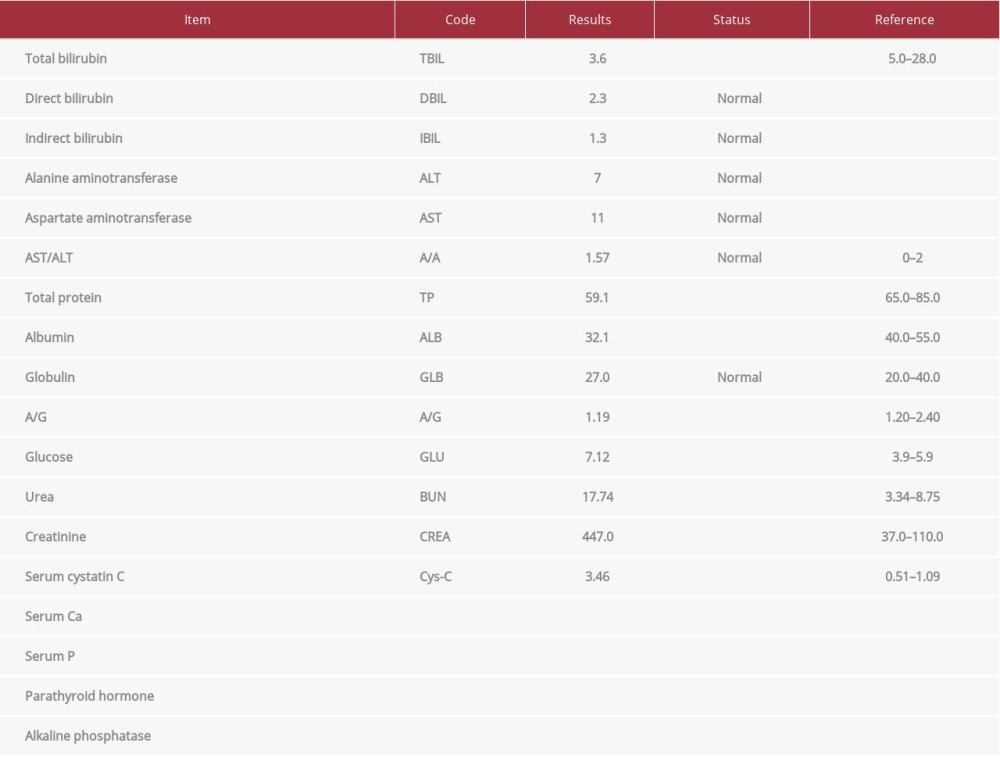 Table 2.. Results of biochemical tests on admission to West China Hospital (some items are not shown).
Table 2.. Results of biochemical tests on admission to West China Hospital (some items are not shown).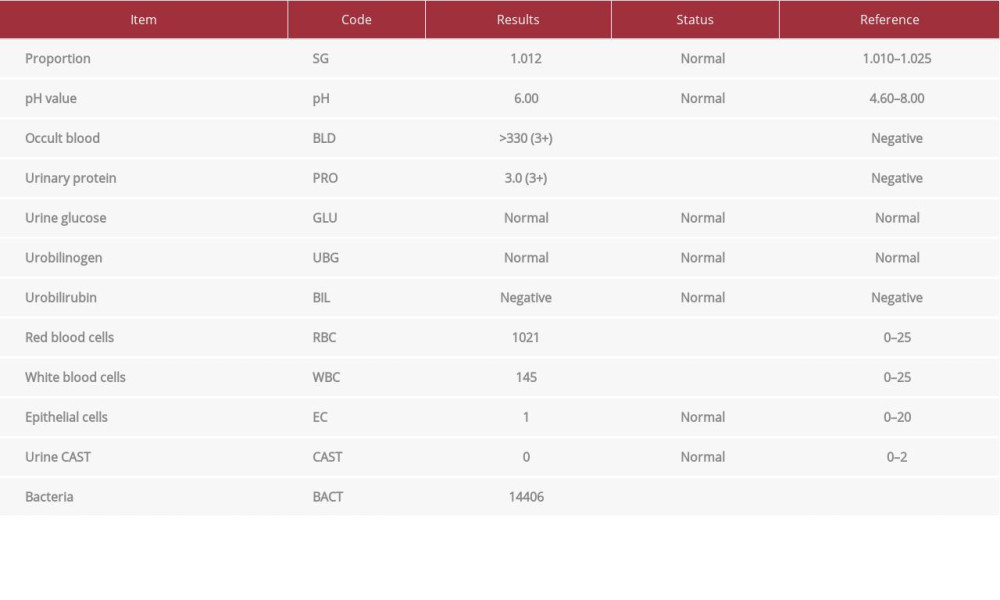 Table 1.. Results of urine tests on admission to West China Hospital (some items are not shown).
Table 1.. Results of urine tests on admission to West China Hospital (some items are not shown).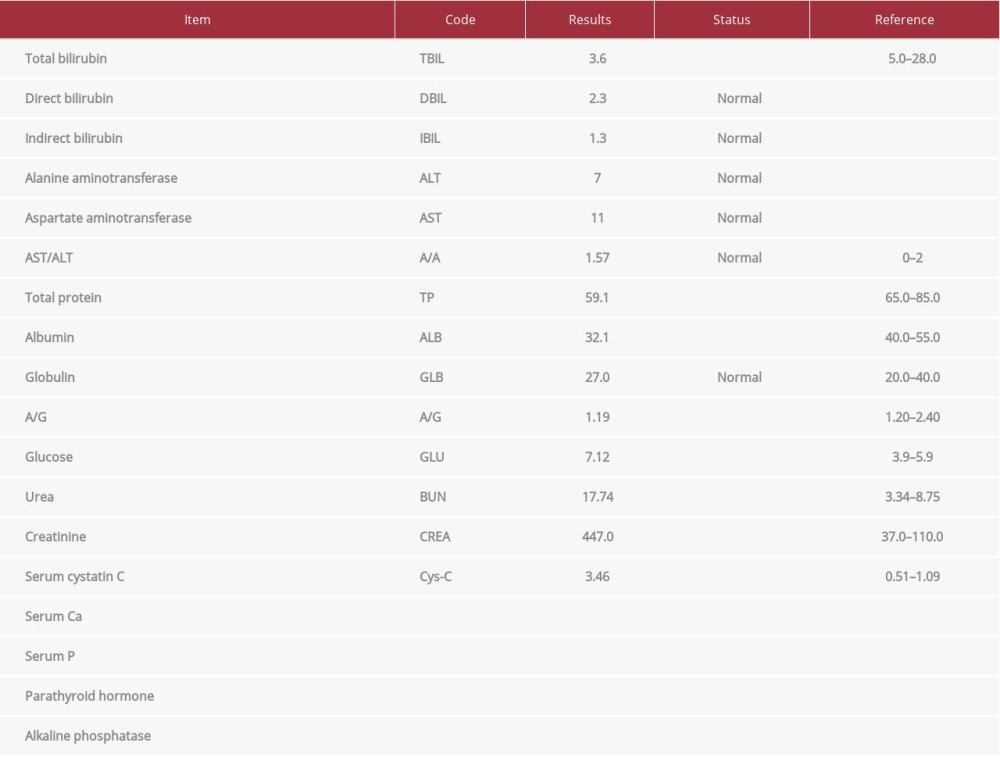 Table 2.. Results of biochemical tests on admission to West China Hospital (some items are not shown).
Table 2.. Results of biochemical tests on admission to West China Hospital (some items are not shown). In Press
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








