16 July 2020: Articles 
Acute Cytomegalovirus (CMV) Hepatitis in an Immunocompetent Adult
Challenging differential diagnosis
Maleeha Zahid1ABCDEF*, Nisha Ali1ABCDEF, Muhammad Saad1ABCDEF, Paul Kelly2ABCDEF, Alfonso Ortiz1ABCDEFDOI: 10.12659/AJCR.925495
Am J Case Rep 2020; 21:e925495
Abstract
BACKGROUND: Cytomegalovirus (CMV) is a member of Herpesviridae family with its name derived from the fact that it causes enlargement of the infected cell resulting in the characteristic inclusion bodies seen on microscopy. CMV virus has an incubation period of about 4 to 6 weeks. Symptoms of CMV infection vary and depend on factors including the age and immune status of the patient. It usually presents as asymptomatic infection in immunocompetent individuals whereas severe disease is usually seen in immunocompromised patients. Here we present a case of an immunocompetent patient who presented with acute CMV hepatitis.
CASE REPORT: A 35-year-old male with no significant prior medical history who presented to the Emergency Department with a 2-week history of low-grade fever. Acute CMV infection was diagnosed by positive CMV antibody and polymerase chain reaction (PCR) testing. The patient was treated with valganciclovir that resulted in rapid improvement in clinical status as well as normalization of the liver enzymes.
CONCLUSIONS: This article presents a rare case of immunocompetent young male with acute CMV hepatitis who responded favorably to antiviral therapy.
Keywords: Hepatitis, Immunocompetence, Antiviral Agents, Hepatitis, Viral, Human, Valganciclovir
Background
Cytomegalovirus (CMV), also known as human herpes virus 5, was first isolated in 1956. The name of this virus is derived from the fact that it causes enlargement of the infected cell resulting in the characteristic inclusion bodies seen on microscopy [1]. Symptoms of CMV infection vary and depend on factors including the age and immune status of the patient. Transmission occurs via body secretions such as saliva, urine, tears, blood, or genital secretions. CMV virus has an incubation period of about 4 to 6 weeks [2]. Infections with CMV are not rare and worldwide seroprevalence for CMV ranges from 60% to 100% [3]. CMV remains latent in the body in most cases, however, in immunosuppressed individuals, CMV can present with severe disease involving multiple organs resulting most commonly in esophagitis or colitis, but also pneumonia, encephalitis, retinitis, myocarditis, hemolytic anemia, and portal vein thrombosis. In immunocompetent individuals, it usually follows an asymptomatic course or presents with a mononucleosis-like syndrome [4–6]. There have been sporadic case reports of acute hepatitis in immunocompetent patients [4,7].
We present a case of young immunocompetent male who presented with acute hepatitis due to CMV infection.
Case Report
Our patient was a 35-year-old male with no significant prior medical history who presented to the Emergency Department with a 2-week history of low-grade fever. Fever pattern was described as irregular without any diurnal variation and ranged from 38.3°C (100.9°F) to 39.4°C (103°F). The patient reported subjective chills and rigors which were partially relieved with the use of acetaminophen. The night before admission, his temperature was 39.4°C (103°F) with chills, profuse diaphoresis, and mild generalized muscle pain after the fever episode. Patient also reported an episode of mild dull right upper quadrant abdominal pain which lasted 2 hours and self-resolved. He had mild coughing at night and had used azithromycin a month earlier for a sore throat and upper respiratory symptoms. Travel history was significant for a trip to Miami within the last month. Of note, the patient’s son was diagnosed with Roseola infection 3 weeks prior to his presentation. Our patient reported allergies to seafood with which he develops itchy rash. Family history was significant for hypertension in father, and breast cancer and diabetes mellitus in mother. He lived with his family and worked as a physician. He denied tobacco use or use of illicit drugs but acknowledged that he drinks alcohol socially, about 1 to 2 beers a month.
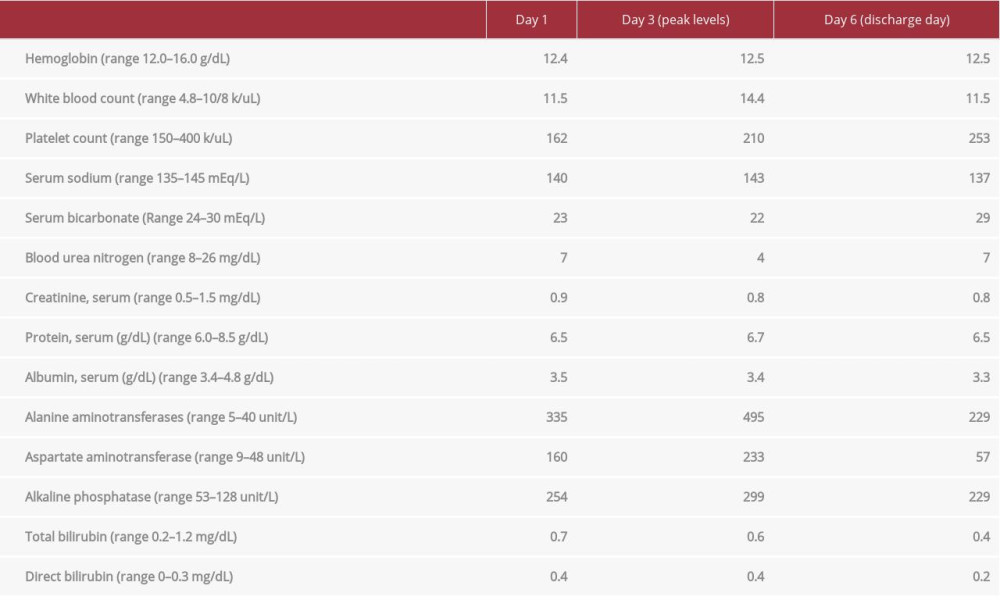
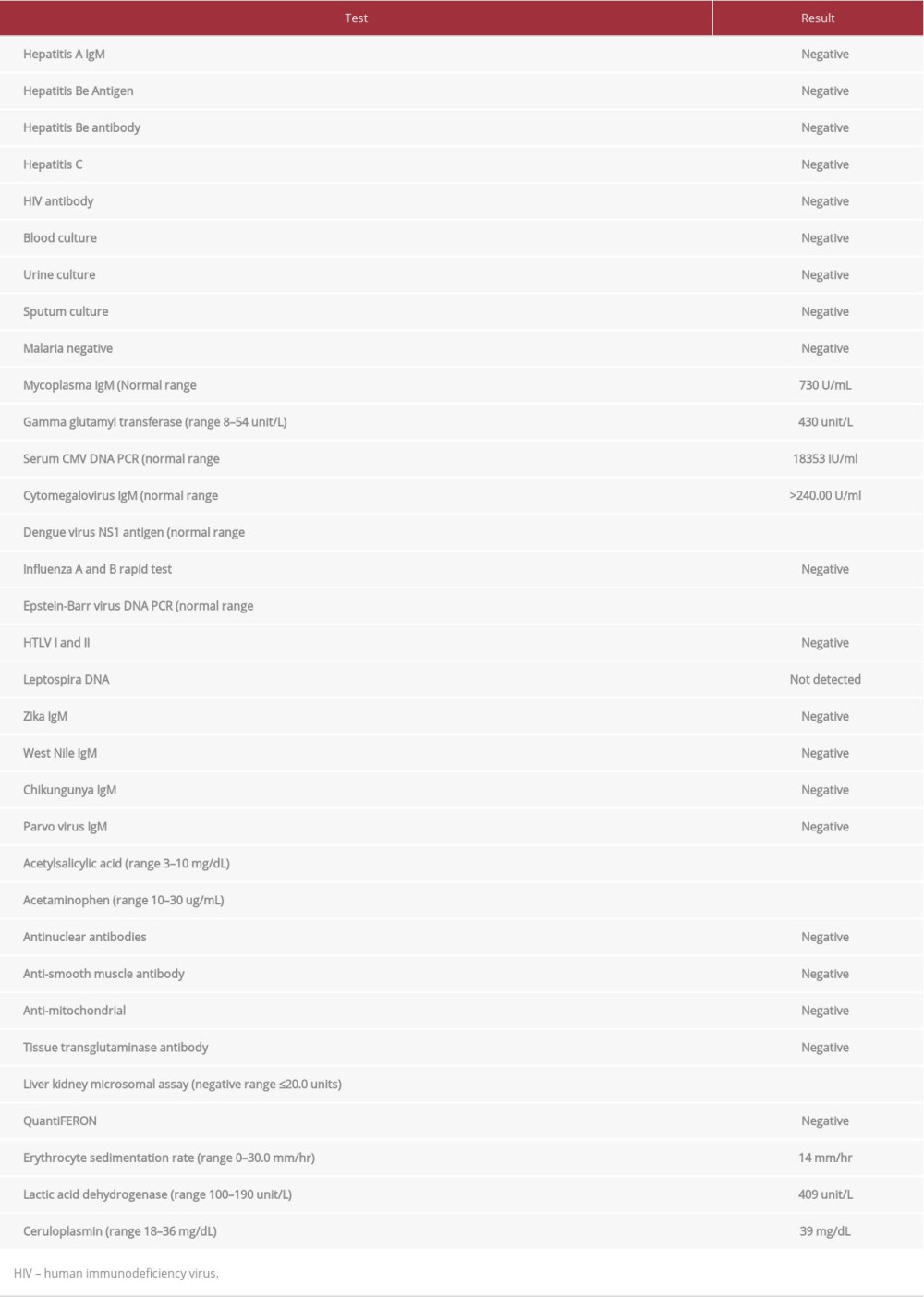
At the time of presentation, the patient had a temperature of 37.2°C (99°F), heart rate 88 beats per minute, blood pressure 120/80 mmHg and respiratory rate of 12 breaths per minute. On physical examination there was no rash, jaundice, or palpable cervical lymphadenopathy. There was no hepatosplenomegaly or abdominal tenderness. Laboratory tests (Table 1) revealed normal metabolic panel, renal function, and complete blood count except for mild leukocytosis (11.5 k/uL). Liver function test (LFTs) showed alanine aminotransferase (ALT) of 335 unit/L (range, 5–40 unit/L), aspartate aminotransferase (AST) of 160 unit/L (range, 9–48 unit/L), alkaline phosphatase (ALKP) of 254 unit/L (range, 53–128 unit/L) and gamma glutamyl transferase (GGT) of 430 unit/L of (range, 8–54 unit/L). Bilirubin and serum protein levels were normal. Urinalysis revealed pH of 8.0 (range, 6.0–8.0), specific gravity of 1.020 (range, 1.005–1.030), small bilirubin and was negative for protein, blood, nitrite, and leukocyte esterase. Abdomen ultrasound showed mild splenomegaly but unremarkable liver. Computed tomography of the abdomen was negative for any abdominal pathology or hepatosplenomegaly. Initial differentials included drug induced liver injury from recent use of azithromycin and infectious hepatitis. Patient was started on ceftriaxone and doxycycline pending testing for leptospirosis and anaplasmosis. Serologic workup (Table 2) was negative for acute hepatitis A, B, and C, Leptospira DNA, Epstein-Barr virus (EBV) DNA PCR, human T-lymphotropic virus type (HLTV)-I and HLTV-II antibody. Serum drug screen for acetaminophen and autoimmune workup was also negative. On Day 3 the patients LFTs continued to rise with ALT of 495 unit/L (range, 5–40 unit/L), aspartate AST of 233 unit/L (range, 9–48 unit/L), and ALKP of 299 unit/L (range, 53–128 unit/L). Serologic studies for CMV revealed IgM levels of >240.00 U/mL (range, <30.00 U/mL), IgG levels of 2.0 U/mL (range, <0.60), and CMV DNA PCR levels of 18353 IU/mL (range, <200 IU/mL). The patient was diagnosed with acute CMV hepatitis and he was started on treatment with valganciclovir on Day 3. Thereafter, the patient improved symptomatically with abatement of fever as well as decline in transaminitis. Given this improvement, a liver biopsy was not pursued. The patient was discharged on Day 6 of his hospitalization. He later followed up in the clinic where his liver enzymes continued to resolve to within normal limits.
Discussion
In a survey done on the United States of the general population aged 12 to 49 years old, the rate of CMV infection was 1.6 per 100 susceptible persons per year and approximately 27 000 new CMV infections occurred among seronegative pregnant women every year [8]. In immunocompetent patients, severe CMV infection can involve almost any organ system, with the gastrointestinal tract (GIT) the most common site followed by the central nervous system (CNS) [9–11]. The most common GIT manifestations include gastroenteritis, enteritis, colitis, and proctitis. CNS involvement can lead to serious conditions such as meningoencephalitis, myelitis, and meningoradiculopathy. Thrombosis of the vascular system is another common presentation of CMV infection in immunocompetent hosts [12] and data shows that CMV virus directly invades the endothelial cells and causes membrane alterations and promotes coagulation. Studies have also linked CMV virus with overexpression of the platelet-derived growth factor, and transforming growth factor-β, which can lead to cell wall proliferation [13]. Ocular and pulmonary involvements are less common in immunocompetent patients.
In a patient presenting with significant transaminitis and parameters of cholestasis but without elevated bilirubin, a clinician must rule out other causes of acute hepatitis. As liver is responsible for concentrating and metabolizing most drugs, it also becomes a main target for drug-induced liver injury (DILI). Diagnosis usually relies on quickly establishing the temporal relationship with the offending agent and stopping it, which leads to resolution of most cases of DILI [14]. Other conditions that can cause hepatitis include autoimmune conditions such as primary biliary cirrhosis, non-alcoholic steatotic hepatitis, and hemochromatosis or infectious etiologies such as those from hepatitis A, B, and C, which are some of the common differential diagnoses. Other less common etiologies include Wilson disease, Budd-Chairi syndrome, ischemic hepatitis, congestive hepatopathy, and muscle disorders.
Steroid use, recent blood transfusion, sepsis, and acute respiratory distress syndrome have been suggested as few of the risk factors for CMV disease in immunocompetent patients [15,16]. However, none of these risk factors were present in our patient. Our patient also had normal CD4 count suggesting preserved cell-mediated immunity which is normally involved in protection against CMV reactivation. It is possible that more risk factors existed, which could trigger or facilitate CMV reactivation that have yet to be identified. Most patients present with mild mononucleosis-like syndrome with abnormal liver enzymes, with or without slight elevation in serum ALKP and bilirubin levels. Liver enzymes usually do not exceed 5 times the normal limit and are self-limiting in most cases and do not require any treatment. Diagnosis of CMV relies on detecting specific IgM antibodies with a cutoff value of >300 U/mL in the absence of other etiologies of hepatitis [17].
Antiviral treatment is reserved for severe cases due to its potential for serious adverse effects such as hepatotoxicity, myelosuppression, infertility, and teratogenesis. When treatment is indicated, it is usually continued for 2 to 3 weeks followed by documented clearance of virus from the blood [2]. A recent case series of CMV infection in immunocompetent patients who received anti-CMV therapy showed significant improvement in symptoms within a few days of starting therapy [18]. Our patient was treated with valganciclovir for total of 21 days. In addition to symptomatic recovery, his liver function tests improved to ALT of 75 unit/L (range, 5–40 unit/L), aspartate AST of 38 unit/L (range, 9–48 unit/L), and ALKP of 107 unit/L (range, 53–128 unit/L) suggesting an overall favorable clinical response.
Conclusions
We presented a case of a young male with acute CMV hepatitis who responded favorably to antiviral therapy. Future randomized trials are recommended to explore the role of antiviral therapy in symptomatic patients.
References:
1.. Schottstedt V, Blümel J, Burger R, Human cytomegalovirus (HCMV) – revised: Transfus Med Hemother, 2010; 37(6); 365-75
2.. Jensen KO, Angst E, Hetzer FH, Gingert C, Acute cytomegalovirus hepatitis in an immunocompetent host as a reason for upper right abdominal pain: Case Rep Gastroenterol, 2016; 10(1); 36-43
3.. Staras SA, Dollard SC, Radford KW, Seroprevalence of cytomegalovirus infection in the United States, 1988–1994: Clin Infect Dis, 2006; 43; 1143-51
4.. Gupta P, Suryadevara M, Das A, Cytomegalovirus-induced hepatitis in an immunocompetent patient: Am J Case Rep, 2014; 15; 447-49
5.. Eddleston M, Peacock S, Juniper M, Severe cytomegalovirus infection in immunocompetent patients: Clin Infect Dis, 1997; 24; 52-56
6.. Gueddi S, Righini M, Mezger N, Portal vein thrombosis following a primary cytomegalovirus infection in an immunocompetent adult: J Thromb Haemost, 2006; 95; 199-201
7.. Serna-Higuera C, Gonzalez-Garcia M, Milicua JM, Acute cholestatic hepatitis by cytomegalovirus in an immunocompetent Patient: J Clin Gastroenterol, 1999; 29(3); 276-77
8.. Colugnati FA, Staras SA, Dollard SC, Cannon MJ, Incidence of cytomegalo-virus infection among the general population and pregnant women in the United States: BMC Infect Dis, 2007; 7; 71
9.. Galiatsatos P, Shrier I, Lamoureux E, Szilagyi A, Meta-analysis of outcome of cytomegalovirus colitis in immunocompetent hosts: Dig Dis Sci, 2005; 50; 609-16
10.. Karakozis S, Gongora E, Caceres M, Life-threatening cytomegalovirus colitis in the immunocompetent patient: report of a case and review of the literature: Dis Colon Rectum, 2001; 44; 1716-20
11.. Rafailidis PI, Mourtzoukou EG, Varbobitis IC, Falagas ME, Severe cytomegalovirus infection in apparently immunocompetent patients: A systematic review: Virol J, 2008; 5; 47
12.. Abgueguen P, Delbos V, Chennebault JM, Vascular thrombosis and acute cytomegalovirus infection in immunocompetent patients: Report of 2 cases and literature review: Clin Infect Dis, 2003; 36; E134-39
13.. Ofotokun I, Carlson C, Gitlin SD, Acute cytomegalovirus infection complicated by vascular thrombosis: A case report: Clin Infect Dis, 2001; 32; 983-86
14.. David S, Hamilton JP, Drug-induced liver injury: US Gastroenterol Hepatol Rev, 2010; 6; 73-80
15.. Ko J-H, Peck KR, Lee WJ, Clinical presentation and risk factors for Cytomegalovirus colitis in immunocompetent adult patients: Clin Infect Dis, 2015; 60(6); e20-26
16.. Papazian L, Hraiech S, Lehingue S, Cytomegalovirus reactivation in ICU patients: Intensive Care Med, 2016; 42(1); 28-37
17.. Wreghitt TG, Teare EL, Sule O, Cytomegalovirus infection in immunocompetent patients: Clin Infect Dis, 2003; 37(12); 1603-6
18.. Nangle S, Mitra S, Roskos S, Havlichek D, Cytomegalovirus infection in immunocompetent adults: Is observation still the best strategy?: ID Cases, 2018; 14; e00442
In Press
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250