09 October 2020: Articles 
A Case of Takotsubo Cardiomyopathy with a Rare Transition Pattern of Left Ventricular Wall Motion Abnormality
Unusual clinical course
Masamichi Yasutomi1ABCDEF, Shotaro Nakamura1BCD, Yuya Makino1B, Ayako Kunimura1B, Kenzo Fukuhara1B, Masafumi Takeda1B, Akira Kimata1B, Sonoko Hirayama1B, Hiroyuki Mataki1B, Toru Ozawa1B, Nobutaka Inoue1ACDEF*DOI: 10.12659/AJCR.926670
Am J Case Rep 2020; 21:e926670
Abstract
BACKGROUND: Takotsubo cardiomyopathy is characterized by apical ballooning and excessive constriction of the base of heart. However, reverse takotsubo cardiomyopathy, wherein ballooning from the mid-ventricle to the base of the heart occurs with excessive constriction of the apex, has also been reported. We report a case of a transition from atypical wall motion abnormality to a typical takotsubo cardiomyopathy pattern.
CASE REPORT: A 54-year-old woman was following excessive sugar and dietary restrictions because of concerns regarding her blood sugar levels while receiving treatment for diabetes at another hospital. She presented at our hospital with general malaise and chest discomfort after several days of significantly increased workload. On admission, blood tests showed elevated cardiac enzymes. Electrocardiogram showed ST elevation of V2-V3 and poor R-wave enhancement of the anterior precordial lead. Coronary angiography showed no significant stenosis; however, left ventricular (LV) angiography showed a decrease in mid-ventricular wall motion. On the basis of these findings, she was diagnosed with a reverse takotsubo cardiomyopathy. We initiated conservative treatment for her condition. During her treatment, the LV wall motion showed a typical pattern of the apical ballooning that is characteristic of takotsubo cardiomyopathy. This LV wall motion was normalized on day 22 of the onset.
CONCLUSIONS: We observed a rare case of takotsubo cardiomyopathy where the pattern of LV wall motion abnormality changed over time. This case suggests that it is necessary to follow up LV abnormality over time rather than rely on single-point observations in cases with takotsubo cardiomyopathy.
Keywords: Cardiology, takotsubo cardiomyopathy, Occupational Health, Arrhythmias, Cardiac, Coronary Angiography, Echocardiography, Electrocardiography
Background
Acute stress-induced (takotsubo) cardiomyopathy has a dramatic clinical presentation similar to acute myocardial infarction. The dyskinetic wall motion in takotsubo cardiomyopathy frequently involves the apex of left ventricle (LV) or mid-ventricular cavity of LV. Takotsubo cardiomyopathy is characterized by apical ballooning and excessive constriction of the base of the heart. However, reverse takotsubo cardiomyopathy, wherein ballooning from the mid-ventricle to the base of the heart occurs with excessive constriction of the apex, has also been reported [1]. We report a case of a transition from atypical wall motion abnormality to a normal takotsubo cardiomyopathy pattern.
Case Report
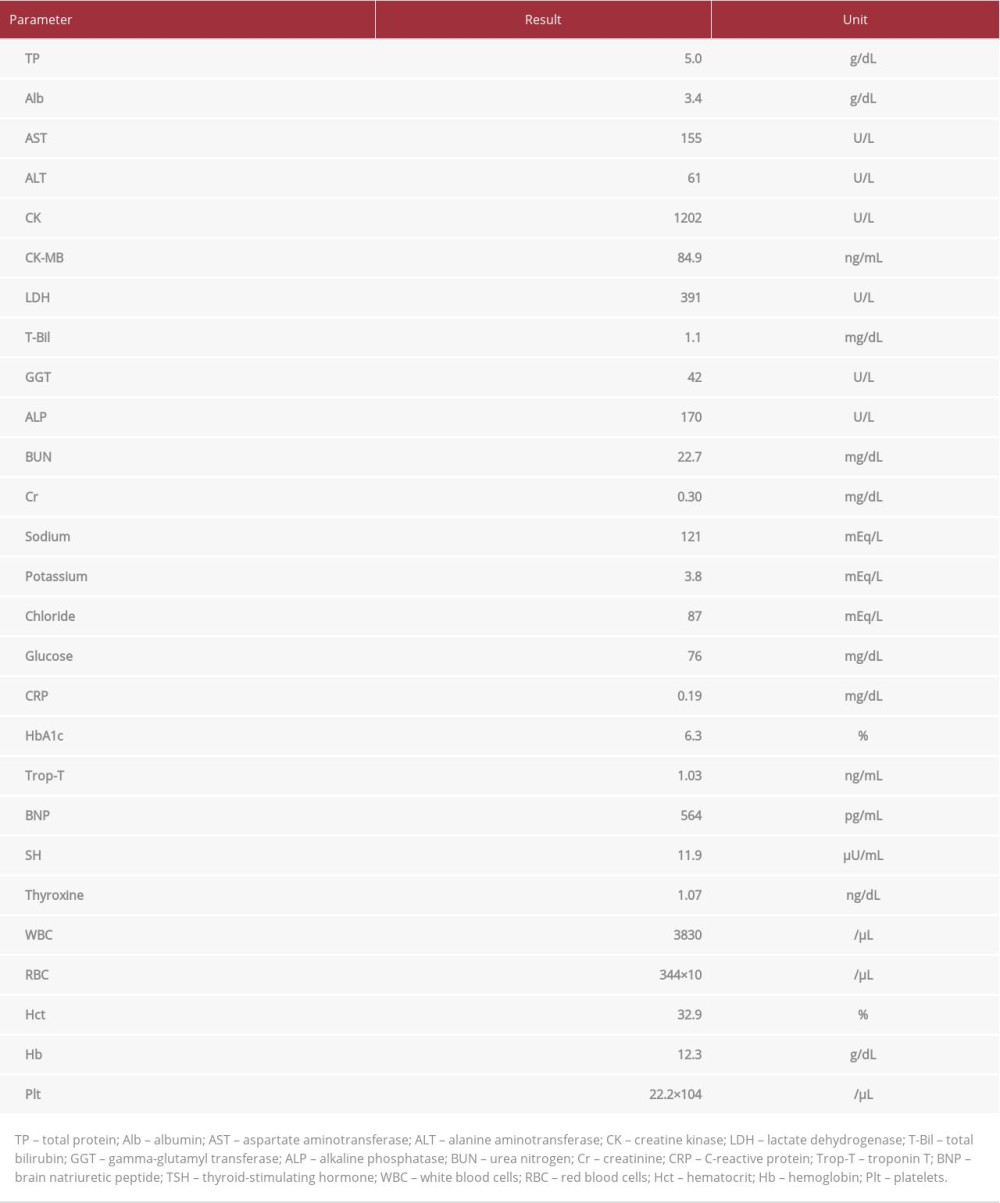
A 54-year-old woman was following excessive sugar and dietary restrictions herself because of concerns regarding her blood sugar levels while receiving treatment for diabetes at another hospital. She was self-employed selling health drinks. Her workload was significantly increased for several days before onset, the results of which included sleeping less than usual. At onset, she became aware of general malaise after returning home. Subsequently, she experienced worsening chest discomfort and she presented to our hospital. On admission, her body mass index (BMI) was 14.6 kg/m2. Her blood pressure was 124/96 mmHg, pulse 67 beats/min, respiratory rate 18 breaths/min with an O2 saturation of 100% in room air. There were no abnormal physical findings other than low BMI. Blood tests revealed electrolyte abnormalities such as hyponatremia and latent hypothyroidism, as well as elevated cardiac enzymes (Table 1). There were no signs of inflammation. Electrocardiogram showed ST elevation of V2–V3 and poor R-wave enhancement of the anterior precordial lead (Figure 1A). Chest X-ray showed neither pneumonia nor heart failure (Figure 1B). Emergency catheterization was performed on suspicion of acute coronary syndrome. No significant stenosis was observed in the left and right coronary arteries (Figure 2A); however, LV angiography showed a decrease in mid-ventricular wall motion (Figure 2B). She had neither signs nor symptoms of pheochromocytoma including headache, heavy sweating, tremor, and sudden rises in blood pressure. Furthermore, abdominal computed tomography showed no tumor in the adrenal gland, indicating that pheochromocytoma was negative as a clinical diagnosis. Since physical findings and blood test showed no evidence of inflammation, myocarditis was also negative. On the basis of the Mayo Clinic’s diagnostic criteria, she was diagnosed with takotsubo cardiomyopathy. However, wall motion abnormality in this case is so-called reverse takotsubo cardiomyopathy, a rare variant of takotsubo cardiomyopathy.
We initiated conservative treatment for her condition. She had a moderate fluid intake, and physical examination and blood tests showed no dehydration. Therefore, we corrected hyponatremia with physiological saline for several days until the fatigue was improved and her appetite was recovered. This patient was considered to be at high risk for refeeding syndrome, and oral nutrition was started with sufficient caution. Specifically, we started with a low-energy diet while supplementing with vitamin B1, and gradually increased calories. We carefully managed electrolytes such as phosphorus, potassium, and magnesium. During the course of treatment, she did not show symptoms and signs of refeeding syndrome. We did not use antithrombotic drugs, β-blockers, or angiotensin-converting enzyme inhibitors.
During the course of her treatment, the pattern of LV wall motion abnormality changed dramatically. Initially, the decrease in LV wall motion was observed in the middle of LV and the hyperkinetic motion was seen in the base and apical portion of the LV. After that, LV wall motion showed a typical pattern of apical ballooning (Figure 2C), which is characteristic of takotsubo cardiomyopathy. On day 22, the LV wall motion normalized. On electrocardiogram, the ST elevation of V2–V3 and the poor progression of R-wave enhancement of the anterior precordial lead were improved. Then, a negative inversion of the T wave of the anterior precordial lead that peaked appeared on day 14, and then improved (Figure 3). The elevation of cardiac enzymes peaked at 1796 IU/L on day 4, then decreased and did not increase again.
Discussion
Characteristics of takotsubo cardiomyopathy is apical ballooning and excessive constriction of the base of the heart. In contrast, reverse takotsubo cardiomyopathy, wherein ballooning from the mid-ventricle to the base of the heart occurs with excessive constriction of the apex, has also been reported. We report a case of a transition from atypical wall motion abnormality to a typical takotsubo cardiomyopathy pattern.
There are variations of LV wall motion abnormalities in takotsubo cardiomyopathy. They are divided into apical type, midventricular type, basal type, and focal type. Among them, the apical type of LV motion abnormality is known to be a typical takotsubo cardiomyopathy pattern. Recently, Templin et al. reported clinical features of takotsubo cardiomyopathy by large-scale clinical research [2]. According to their reports, 81.7% of the patients with takotsubo cardiomyopathy had apical type, 14.6% had mid-ventricular type, and basal type and focal type were 2.2% and 1.5%, respectively. In the current case, the wall motion abnormality transitioned from the mid-ventricular type to the apical type.
There are only a few reports of takotsubo cardiomyopathy in which the site of abnormal wall motion changed over time [3,4]. Yadlapati and Chandrasekaran reported a case demonstrating sequential transition of mid-ventricular type to apical type of takotsubo cardiomyopathy [4]. In their case, the wall motion abnormality transited from the mid-ventricular type to the apical type. However, an investigation of 1750 patients with takotsubo cardiomyopathy by Templin et al. did not find this pattern [2], suggesting that it is necessary to follow up LV abnormality over time rather than just consider a single-point observation.
In the current case, the pattern of LV wall motion abnormality changed over time dramatically. We think that the phenomenon of the transition of LV wall motion abnormality provides an insight into the pathogenesis of takotsubo cardiomyopathy. It is hard to identify its cause, since the etiology of takotsubo cardiomyopathy itself is still unknown. At present, there are various theories that have been proposed, including multi-vessel coronary artery spasm theory, the microcirculatory disorder theory, the catecholamine myocardial disorder theory, and the estrogen decrease theory. It is now evident that the disturbance of epicardial coronary circulation is not involved in the pathogenesis of takotsubo cardiomyopathy because the regions of LV wall motion abnormality are not related to coronary perfusion area [5,6]. Furthermore, the absence of obstructive coronary artery disease is one of Mayo Clinic criteria for diagnosis of takotsubo cardiomyopathy [7]. Recently, there has been accumulating evidence indicating that the dys-regulation of cardiac autonomic nerves plays a possible role. Paur et al. demonstrated that the cause of ventricular dysfunction in takotsubo cardiomyopathy is due to an epinephrine-induced β2-adrenergic receptor Gs/Gi switch [8]. Furthermore, Borchert et al. demonstrated that induced pluripotent stem cell-derived cardiomyocytes from patients with severe takotsubo cardiomyopathy phenotype showed strong catecholamine sensitivity and altered β-adrenergic signaling as a potential disease cause [9]. Thus, the enhancement of sympathetic nerve activity, the distribution of adrenoceptors and muscarinic receptors, and the difference in the mutual relationship between sympathetic nerves and parasympathetic nerves may be involved in takotsubo cardiomyopathy. According to the cardiac autonomic nerve theory, the regions of LV wall motion abnormality should depend upon the innervation of cardiac autonomic nerves. The previous investigations revealed that the innervation of intrinsic cardiac autonomic nerves including cardiac ganglia is very complex and still controversial, and cardiac autonomic neural networks highly regulate the regional cardiac function [10]. The regionality of LV wall motion abnormality in takotsubo cardiomyopathy could be partially explained by the cardiac autonomic neural networks. The area where the dysregulation of cardiac autonomic nerves occurred might temporally and spatially be changed in the present case. Temporal and spatial changes of the area of dysregulation in cardiac autonomic neural networks might contribute to an altered wall motion abnormality observed in the present case.
In the present case, occupational stress was a possible cause of the onset of takotsubo cardiomyopathy. There are only a few case reports of takotsubo cardiomyopathy caused by occupational stress. Mielczarek et al. reported a case of a 55-year-old female teacher who developed the disease because of a quarrel with the headmaster [11]. Malik et al. also reported a case of a 48-year-old newly appointed female manager who developed the disease because of workplace bullying [12]. Both cases in these previous reports seemed to be mainly caused by psychological stress; however, the occupational stress in the present case was mainly due to physical stress caused by increased workload. Occupational stress can be measured by qualitative constructs such as job control, job demands, and social support in the workplace. A work environment with high occupational stress is a situation where job control is low, that is, discretionary power at work is low, and job demands are high, that is, a workload is large [13]. In the present case, job demands especially were increased. The increase in occupational stress associated with various physical and mental stresses can cause various reactions, including hypertension, gastric and duodenal ulcers, and depression. Taken together with previous reports, occupational stress is emerging as an important inducer of takotsubo cardiomyopathy.
Conclusions
We encountered a rare case of takotsubo cardiomyopathy where the pattern of LV wall motion abnormality changed over time. From this case, we confirmed that it is necessary to follow up LV abnormality over time rather than rely on a single-point observation. It is reported that mental and physical stresses are often the triggers for the onset of takotsubo cardiomyopathy. Intense occupational stress could be the cause of the onset, so it is necessary to pay attention to its development in workers.
Figures
References:
1.. Patankar GR, Choi JW, Schussler JM, Reverse takotsubo cardiomyopathy: Two case reports and review of the literature: J Med Case Rep, 2013; 7; 84
2.. Templin C, Ghadri JR, Diekmann J, Clinical features and outcomes of takotsubo (stress) cardiomyopathy: N Engl J Med, 2015; 373; 929-38
3.. Chattopadhyay S, John J, Tako-Tsubo and reverse Tako-Tsubo cardiomyopathy: Temporal evolution of the same disease?: Eur Heart J, 2009; 30; 2837
4.. Yadlapati A, Chandrasekaran K, Sequential transition of mid-basilar variant to apical form of takotsubo syndrome: J Cardiol Cases, 2013; 8; 99-104
5.. Del Buono MG, Potere N, Chiabrando JG, Takotsubo syndrome: Diagnostic work-up and clues into the differential diagnosis: Curr Opin Cardiol, 2019; 34; 673-86
6.. Komamura K, Fukui M, Iwasaku T, Takotsubo cardiomyopathy: Pathophysiology, diagnosis and treatment: World J Cardiol, 2014; 6; 602-9
7.. Scantlebury DC, Prasad A, Diagnosis of takotsubo cardiomyopathy – Mayo Clinic criteria: Circ J, 2014; 78; 2129-39
8.. Paur H, Wright PT, Sikkel MB, High levels of circulating epinephrine trigger apical cardiodepression in a β2-adrenoceptor/Gi-dependent manner: A new model of takotsubo cardiomyopathy: Circulation, 2012; 126; 697-706
9.. Borchet T, Hubscher D, Guessoum CI, Catecholamine-dependent βadrenergic signaling in a pluripotent stem cell model of takotsubo cardiomyopathy: J Am Coll Cardiol, 2017; 22; 70 : 975–91
10.. Wink J, van Delft R, Notenboom RGE, Human adult cardiac autonomic innervation: Controversies in anatomical knowledge and relevance for cardiac neuromodulation: Auton Neurosci, 2020; 227; 102674
11.. Mielczarek A, Kasprzak JD, Marcinkiewicz A, Broken heart as work-related accident: Occupational stress as a cause of takotsubo cardiomyopathy in 55-year-old female teacher – role of automated function imaging in diagnostic workflow: Int J Occup Med Environ Health, 2015; 28; 1031-34
12.. Malik H, Kangaharan N, Agahari I, Takotsubo cardiomyopathy associated with work-place bullying: Occup Med, 2018; 68; 67-69
13.. Inoue N, Otsui K, Yoshioka T, A simultaneous evaluation of occupational stress and depression in patients with lifestyle-related diseases: Intern Med, 2016; 55; 1071-75
Figures
In Press
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250