27 November 2021: Articles 
Nodular Sclerosing Mesenteritis: An Occasional Finding Mimicking a Spindle Cell Tumor
Challenging differential diagnosis, Rare disease
Giovanna Brancato1AE, Marcello Donati1AE, Lucia Salvatorelli2CF, Gaetano Magro2CD, Michela Zanatta1BE*, Francesca Lentini1BF, Guido Basile1DFDOI: 10.12659/AJCR.933189
Am J Case Rep 2021; 22:e933189
Abstract
BACKGROUND: The term “sclerosing mesenteritis” includes a spectrum of rare idiopathic diseases involving the small and/or large bowel. It appears as a diffuse, localized, or multinodular thickening of the mesentery, with a variable degree of chronic non-specific inflammation, fat necrosis, and fibrosis.
CASE REPORT: Here, we report a case of 83-year-old woman with symptoms of intestinal occlusion, vomiting, and abdominal pain. Radiographic examinations showed air fluid levels in right and left quadrants and in the mesogastric site, while computed tomography (CT) documented a strangulated inguinal hernia with ileal obstruction. Based on clinical examination and radiologic findings, the patient underwent surgery for inguinal hernia reduction. The examination of viscera revealed 2 tracts of ileum with ischemic signs and covered by fibrin; thus, the 2 intestinal loops were resected. Histological examination revealed chronic non-specific inflammation of the whole intestinal wall, including the subserosa in the resected tract of proximal ileum, while the distal ileal loop (not herniated tract) showed a subserosal fibrous nodule of 2 cm in greatest diameter, composed of a proliferation of spindle cells haphazardly arranged in a collagenized stroma. The diagnosis of sclerosing mesenteritis was rendered.
CONCLUSIONS: The present case shows the possibility of an incidental diagnosis during another intervention such as hernia surgery. Pathologists should be aware of this disease to avoid confusion with aggressive tumors such as intra-abdominal desmoid-type fibromatosis and gastrointestinal stromal tumor.
Keywords: Abdominal Wall, Hernia, Inguinal, Panniculitis, Peritoneal, Aged, 80 and over, Female, Humans, Intestinal Obstruction, Intestine, Small, Mesentery, Neoplasms
Background
The term “sclerosing mesenteritis” includes a wide spectrum of idiopathic diseases involving the small and/or large bowel. It may appear as a diffuse, localized, or multinodular thickening of the mesentery, with a variable degree of chronic non-specific inflammation, fat necrosis, and fibrosis [1,2]. Sclerosing mesenteritis, first described by Jura et al as “retractile mesenteritis” in 1924 [3], was later (1965) renamed by Ogden et al as “mesenteric panniculitis” [4]. Sclerosing mesenteritis has been reported in association with colorectal carcinoma, diverticular disease, and strangulated inguinal hernias as localized and nodular forms of panniculitis, sometimes with retraction and distortion of the intestinal loops, with adhesions between them [5].
The etiology and pathogenesis of this condition are unknown, although it is often associated with a clinical history of trauma, infections, ischemia, and autoimmune diseases. Many authors agree that sclerosing mesenteritis probably does not constitute a specific entity but is rather a reactive fibroblastic/myofibroblastic proliferation of intra-abdominal fat.
Herein, we present a case of nodular sclerosing mesenteritis incidentally diagnosed after surgical hernia reduction. Interestingly, the lesion was found in a tract of distal ileum not involved by mechanical obstruction and it was histologically composed of spindled myofibroblasts set in a collagenized stroma without evidence of an inflammatory component.
Case Report
An 83-year-old woman presented to our unit with obstruction signs, vomiting, and abdominal pain. Her clinical history was negative for neoplastic diseases. In the past clinical history of the patient, there was the endoscopic resection of 2 colonic polyps which were histologically classified as a “tubular adenomas with low-grade dysplasia”. In addition, the patient had already undergone right inguinal hernioplasty. Laboratory investigation results were normal, except for low sodium levels and increased levels of cardiac markers. Radiographic examination revealed air fluid levels in right and left quadrants and in the mesogastric site, while free subdiaphragmatic air was not evident. Computed tomography (CT) revealed a thickened intestinal wall in multiple loops in the context of a right inguinal hernia, while the loops upstream of the obstruction were expanded with multiple air fluid levels (Figure 1). Multiple enlarged lymph nodes were appreciable on the right side. Accordingly, the patient underwent hernioplasty. Xifo-pubic incision was performed. After opening the peritoneum jejuno-ileum tract distension was evident. An ileal loop was incarcerated in the crural region, showing ischemic signs. An ileal resection with manual termino-terminal anastomosis was performed. In addition, another loop (distal ileum), adjacent to the cecum, showed a fibrous nodule in the mesentery; therefore, resection with end-to-end anastomosis was performed. The distal ileal loop was approximately 10 cm in length. In the mesentery, a nodular, firm, whitish lesion, measuring 2 cm in greatest diameter, was observed. The proximal ileal loop was 3.5 cm in length and showed a thickened bowel wall and a slightly narrowed lumen. Histologically, the incarcerated loop showed subacute/chronic non-specific inflammation (lymphocytes, plasma cells, granulocytes) of the whole intestinal wall, and hemorrhage, resulting in slight subserosal thickening (Figure 2A). Notably, the mesenteric fibrous nodule in the distal ileal loop wa found to be histologically composed of a proliferation of spindle-shaped cells with slightly eosinophilic cytoplasm and elongated normochromic nuclei with mild to focally moderate atypia, haphazardly set in a collagenized stroma (Figure 2B). Only focally scattered lymphocytes and macrophages were observed. The submucosa was markedly edematous. Mucosal erosions and hemorrhage were absent. Immunohistochemical analyses, with diffuse staining for vimentin and α-smooth muscle actin (Figure 3A), revealed the myofibroblastic nature of the spindle cells. DOG1, CD117, CD34, β-catenin (Figure 3B–3D), S100 protein, pancytokeratins, and EMA were negative. Based on the morphological and immunohistochemical features, the diagnosis of “nodular sclerosing mesenteritis” was rendered.
Given the histologic results, the patient was submitted to a follow-up program consisting in a first CT scan after 6 months, followed by an annual CT scan for the first 2 years.
Discussion
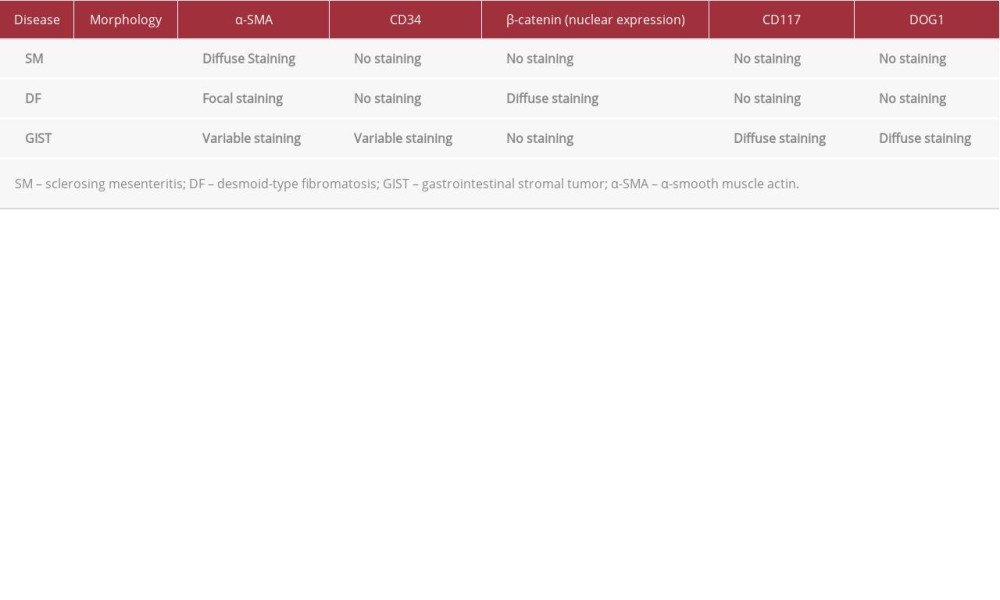
Sclerosing mesenteritis is a rare disease of uncertain etiology in the wide spectrum of mesenteric panniculitis. The diagnosis of mesenteric panniculitis is based on evaluation of the following 3 components: I) necrosis, II) chronic inflammation, and III) fibrosis. According to the predominant component, there are at least 3 distinct pathological phases: I) mesenteric lipo-dystrophy, when fat necrosis is predominant; II) mesenteric panniculitis, if both fat necrosis and inflammation are present; and III) sclerosing mesenteritis, when fibrosis is predominant [6,7]. The whole bowel wall can be involved, except for the mucosa, which remains intact [8]. Sclerosing mesenteritis is more often seen as a secondary rather than a primary pathological condition. Indeed, although the etiology of mesenteric panniculitis remains unknown, some cases have been reported in association with IgG4-related disease, a fibroinflammatory condition characterized by an inflammatory infiltration of IgG4-positive plasma cells, fibrosis, and obliterative phlebitis. In these cases, the lesions show a diffuse fibrosis and infiltration of IgG4-positive plasma cells [9–11]. Recently, a review on the topic [12] has discussed all the conditions that can be associated with mesenteric panniculitis, including previous abdominal surgeries or traumas, neoplasms (colorectal, lung, gastric carcinomas, lymphomas), autoimmune diseases (Sjogren’s syndrome, sclerosing cholangitis, Riedel’s thyroiditis), infectious diseases (tuberculosis) and vascular insufficiency. The differential diagnosis includes benign and malignant lesions, especially desmoid-type fibromatosis and gastrointestinal stromal tumor (Table 1). Sclerosing mesenteritis is a disease whose symptoms are unclear and difficult to identify. In the literature, the most frequently reported symptoms were abdominal pain, diarrhea, and weight loss [1], obstructive symptoms [2,7], abdominal mass [4,5,9], and unusual presentations due to the disease localization; in some cases, no relevant symptoms were reported [2,3,8]. Because of the low prevalence [10] and the heterogeneous presentations, sclerosing mesenteritis is seldom considered in the differential diagnosis. Frequently, the patient undergo surgery for the complications [4,6] and bowel and/or mass resection is performed [5,6,11,12]. Because the symptomatology is so uncertain and diverse, imaging may help in the diagnosis [13]. In CT study, the “fat-ring sign” or “fatty halo”, consisting in low-density fat surrounding nodules and vessel within the mass, even if non-pathognomonic, has been reported in 75–80% of sclerosing mesenteritis cases [10,14]; likewise, small soft-tissue nodules, usually less than 5 mm in diameter, are found within the mesenteric mass in 80% of patients [10]. Sclerosing mesenteritis localized to the small bowel mesentery may mimic a malignant neoplasm both clinically and radiologically, and sometimes even histologically. The present case is intriguing because the nodular sclerosing mesenteritis was incidentally found in the distal ileum of a patient who underwent hernia repair. Notably, histological examination showed a fibro-sclerotic myofibroblastic spindle cell tumor-like lesion lacking inflammatory components and fat necrosis, suggesting that an inflammatory or traumatic pathogenesis was unlikely. The differential diagnosis of our case mainly included desmoid-type fibromatosis, gastrointestinal stromal tumor, and leiomyosarcoma. Unlike desmoid-type fibromatosis, our lesion did not show infiltrative margins, an organized fascicular growth pattern, or expression of b-catenin. Gastrointestinal stromal tumor, the most common mesenchymal tumor of the gastrointestinal tract, shows more cellularity than sclerosing mesenteritis and it is characteristically stained with CD117, CD34, and DOG-1. In our case, none of these markers were found. As the spindle cells of our case exhibited a diffuse expression of α-smooth muscle actin, the possibility of a leiomyosarcoma had to be excluded. The absence of a clear-cut fascicular arrangement, severe nuclear atypia, and high mitotic index are all features which argue against the diagnosis of malignancy. In case of doubtful symptomatology, a careful imaging study together with an eventual exploration with biopsy and histopathological examination may help to define the suspected diagnosis before the onset of complications and the need for surgery, as reported in the literature [2, 15]. A multidisciplinary approach is therefore recommended. Steroid therapy may help reduce symptomatology [2,15] and is used in postoperative care [5].
Conclusions
In conclusion, sclerosing mesenteritis is a rare disease (prevalence <1%, incidence around 3.4%) [16] which should be considered in the differential diagnosis of inflammatory and/or neoplastic lesions of the intestine. The present case defines the possibility of an incidental diagnosis during another intervention such as hernia repair. Pathologists should be aware of this disease to avoid confusion with aggressive tumors such as intra-abdominal desmoid-type fibromatosis and gastrointestinal stromal tumor.
Sclerosing mesenteritis represents an incidental finding for the surgeon, a feast for the pathologist, and a relief for the patient.
Figures
References:
1.. Emory TS, Monihan JM, Carr NJ, Sobin LH, Sclerosing mesenteritis, mesenteric panniculitis and mesenteric lipodystrophy: A single entity?: Am J Surg Pathol, 1997; 21(4); 392-98
2.. Kelly JK, Hwang WS, Idiopathic retractile (sclerosing) mesenteritis and its differential diagnosis: Am J Surg Pathol, 1989; 13(6); 513-21
3.. , Mesenteric panniculitis: JAMA, 1966; 195(2); 164
4.. Ogden WW, Bradburn DM, Rives JD, Mesenteric panniculitis: Review of 27 cases: Ann Surg, 1965; 161; 864-75
5.. Bak M, Nodular intra-abdominal panniculitis: An accompaniment of colorectal carcinoma and diverticular disease: Histopathology, 1996; 29(1); 21-27
6.. Coulier B, Mesenteric panniculitis. Part 1: MDCT – pictorial review: JBR-BTR, 2011; 94(5); 229-40
7.. Coulier B, Mesenteric panniculitis. Part 2: Prevalence and natural course: MDCT prospective study: JBR-BTR, 2011; 94(5); 241-46
8.. Wat SY, Harish S, Winterbottom A, The CT appearances of sclerosing mesenteritis and associated diseases: Clin Radiol, 2006; 61(8); 652-58
9.. Minato H, Shimizu J, Arano Y, IgG4-related sclerosing mesenteritis: A rare mesenteric disease of unknown etiology: Pathol Int, 2012; 62(4); 281-86
10.. Kim EJ, Kim EY, Song JE, [A case of IgG4-related sclerosing mesenteritis associated with Crohn’s disease.]: Korean J Gastroenterol, 2014; 63(3); 176-82 [in Ko]
11.. Abe A, Manabe T, Takizawa N, IgG4-related sclerosing mesenteritis causing bowel obstruction: A case report: Surg Case Rep, 2016; 2(1); 120
12.. Hussein MR, Abdelwahed SR, Mesenteric panniculitis: An update: Expert Rev Gastroenterol Hepatol, 2015; 9(1); 67-78
13.. Akram S, Pardi DS, Schaffner JA, Smyrk TC, Sclerosing mesenteritis: Clinical features, treatment, and outcome in ninety-two patients: Clin Gastroenterol Hepatol, 2007; 5(5); 589-96
14.. Vlachos K, Archontovasilis F, Falidas E, Sclerosing mesenteritis: Diverse clinical presentations and dissimilar treatment options. A case series and review of the literature: Int Arch Med, 2011; 4; 17
15.. Nyberg L, Björk J, Björkdahl P, Sclerosing mesenteritis and mesenteric panniculitis – clinical experience and radiological features: BMC Gastroenterol, 2017; 17(1); 75
16.. Green MS, Chhabra R, Goyal H, Sclerosing mesenteritis: A comprehensive clinical review: Ann Transl Med, 2018; 6(17); 336
Figures
In Press
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250