16 August 2022: Articles 
Osteolytic Lesion of the Maxilla in an Undiagnosed Multiple Myeloma Patient Identified Incidentally by Cone Beam Computed Tomography
Unusual clinical course, Challenging differential diagnosis, Rare disease
Sarah AlFarabi AliDOI: 10.12659/AJCR.936585
Am J Case Rep 2022; 23:e936585
Abstract
BACKGROUND: Multiple myeloma is a hematological malignancy characterized by monoclonal plasma cell proliferation. Jaw lesions are found in nearly 35% of patients with symptomatic myeloma, and lesions occur in the mandible more often than in the maxilla. However, maxillary or mandibular lesions are rarely found as a primary manifestation of the disease. This report describes a case of a 65-year-old Palestinian woman with lytic lesions in the maxilla due to undiagnosed multiple myeloma identified incidentally on cone beam computed tomography (CBCT).
CASE REPORT: A 65-year-old Palestinian woman presented to the Oral Maxillofacial Surgery Clinic with an expansion of the maxilla which was initially thought of as an infection. CBCT imaging revealed diffuse osteolytic lesions involving multiple osseous structures. The patient was biopsied. Histopathological examination was suspicious for plasmacytic neoplasm. She was directly referred to the Hematology Department for further laboratory tests. These included complete blood count, liver function test, bone profile, protein electrophoresis, flow cytometry, and bone marrow biopsy, which were performed to confirm the diagnosis of multiple myeloma. The patient was treated with chemotherapy including zoledronic acid, dexamethasone, bortezomib, and cyclophosphamide. She went into remission for a year but unfortunately died 2 years later.
CONCLUSIONS: Primary myeloma of the maxilla is a rare presentation. The present report illustrates the role of CBCT imaging supported by a multidisciplinary approach to the diagnosis and management of myeloma. Consequently, it is recommended that dental practitioners be aware of radiographic features and possible oral manifestations to avoid any delay in medical intervention.
Keywords: Cone-Beam Computed Tomography, Incidental Findings, Maxilla, Mouth, Multiple Myeloma, Aged, Dentists, Female, Humans, Professional Role
Background
Multiple myeloma is a hematologic malignancy which represents around 10% of malignant hematological diseases [1]. It is characterized by neoplastic plasma cell proliferation in the bone marrow. The antibodies that are overproduced by these plasma cells, named M proteins, are monoclonal kappa or lambda light-chain antibodies with or without the heavy chain, which may be detected in serum or urine of myeloma patients [2]. These neoplastic cells stimulate atypical maturation of osteoclast precursor cells, which in turn function abnormally. An imbalance between bone formation and resorption occurs, resulting in osteolytic lesions, which may mimic a primary bone tumor. These occur frequently in the spine, femur, ribs, humerus, pelvis, and cranium of myeloma patients [3]. Jaw lesions have been reported in 35% of myeloma cases, albeit not as a primary manifestation of the disease [4]. The body, angle, and ramus of the mandible are the parts most affected [5]. Myeloma is preceded by monoclonal gammopathy of undetermined significance, and is characterized by hypercalcemia, renal insufficiency, anemia, and bone lesions (CRAB). The main features include bone pain, fatigue, and infections [6]. Since the detection of bone lesions is crucial to the diagnosis and treatment of multiple myeloma, the International Myeloma Working Group (IMWG) has published recommendations for optimal imaging at different disease stages. Cross-sectional imaging such as low-dose computed tomography is recommended [7]. Furthermore, the IMWG has published a guideline for diagnosis, investigation, and treatment of myeloma. [6,8].
Oral signs and symptoms include pain, bleeding, dysphagia, paresthesia, and amyloidosis [9]. The tongue is the most commonly affected site in the oral cavity; the condition may result in macroglossia due to amyloidosis [10]. Presentation of myeloma in the oral cavity is variable. It may appear clinically as a small gingival mass or as an intra-osseous lesion resulting in facial asymmetry [11]. This disease generally affects men and is considered predominantly a disease of the elderly, usually affecting those between the sixth and seventh decades [12]. Since myeloma in the oral cavity is a rare disease, knowledge of clinical symptoms and early manifestations is important for early diagnosis. Although the occurrence of either maxillary or mandibular lesions as an early indicator is relatively rare, a differential diagnosis of myeloma should be considered for jaw lesions, especially in geriatric patients with other manifestations. Early identification could influence both the management and outcome of the disease. Such was the case reported by Kasamatsu et al, who reported a maxillary swelling as an initial manifestation of myeloma [13]. In addition, Ali et al described a mandibular swelling as the first indication of multiple myeloma [14]. The present report describes the case of a 65-year-old Palestinian woman with a lytic lesion of the right maxilla due to undiagnosed multiple myeloma identified by cone beam computed tomography (CBCT).
Case Report
A 65-year-old Palestinian woman attended the Oral and Maxillofacial Surgery Clinic seeking treatment for a palatal lesion in the right maxilla which had been present for 10 months. Intraoral examination revealed buccopalatal expansion of the right maxilla with pus discharge and fetid odor. Clinically, the differential diagnosis included a wide range of diagnoses including osteomyelitis, fibrous dysplasia, and lymphoma. The patient’s medical history included diabetes mellitus, hypertension, osteoporosis and idiopathic thrombocytopenia purpura. The patient was taking 500 mg metformin, 15 mg amlodipine, 70 mg alendronic acid, and 5 mg predniso-lone. No other clinical symptoms were reported. A CBCT was requested for the area, after which an incisional biopsy was performed under local anesthesia.
CBCT imaging showed a total opacification of the right maxillary and frontal sinuses with an associated irregular destruction of the right maxillary sinus walls and maxillary tuberosity as well as sequestrations (Figure 1). Sclerotic changes and thickening of the right pterygoid plates were also evident. The radiographic findings of the maxillary bone and maxillary sinus were suggestive of a long-standing infection. However, further evaluation of the entire CBCT examination revealed that the skull, cervical vertebrae, and mandible demonstrated multiple, “punched-out”, osteolytic lesions with an associated perforation of the cortical boundaries (Figures 2, 3). These radiographic features are classically seen in multiple myeloma.
The sections submitted for microscopic evaluation consisted of viable bone trabeculae with active marrow intermixed with inflammatory cells (Figure 4A). Multiple areas showed sheets of atypical plasma cells. The plasmacytoid cells showed eccentric nuclei and abundant eosinophilic cytoplasm (Figure 4B). Immunohistochemical stains demonstrated positivity to CD138 with Lambda positivity (Figure 5A, 5B) and negativity to CD3 and CD20 (Figure 5C, 5D). Accordingly, the histologic picture was suspicious for plasma cell neoplasm.
The patient was then referred to the Hematology Department for diagnosis. Hematologic investigations were done (Table 1). These revealed low albumin, immunoglobulin M, aspartate aminotransferase, and gamma glutamyl transferase. On the other hand, C-reactive protein, alpha-1 protein, and B2 microglobulin were elevated. Serum-free light chain concentrations were within normal range. Complete blood count showed high white blood cell count, normal red blood cell count, and low red blood cell indices (hemoglobin, hematocrit, mean cell hemoglobin, and mean cell hemoglobin concentration). Protein electrophoresis displayed low albumin and high alpha-1 protein (Table 2). Bone function profile was within normal limits (Table 3).
The bone marrow aspirate was moderately hypercellular, megakaryocytes were adequate, myelopoiesis was hyperactive, and erythropoiesis was reduced with normoblastic maturation. Blasts were less than 1%, lymphocytes constituted about 14%, plasma cells were increased 16%, and rare binucleated forms were present. Histiocytes were prominent and active. Trephine biopsy was done showing hypercellular marrow with atypical plasma cells in different arrangements. There was reduced hematopoiesis. The myeloid/erythroid ratio was preserved.
Skeletal survey and urinalysis were negative. Flow cytometry results showed cells that were initially identified using CD138 and side scatter. These CD138 gated cells showed expression of CD56, while CD19 and CD45 were negative, which was consistent with multiple myeloma. The patient was treated with chemotherapy (Zoledronic acid, cyclophosphamide, bortezomib, and dexamethasone). The disease was controlled in a year. Three years after the initial diagnosis of the multiple myeloma, however, the patient died due to renal complications.
Discussion
Primary myeloma of the maxilla is a rare presentation. Since CBCT played a major role in the diagnosis of this case, it is recommended that dental practitioners to be aware of radio-graphic features and possible oral manifestations of myeloma to avoid any delay in medical intervention. In general, multiple myeloma is a malignant neoplasm of monoclonal plasma cells. Symptoms of bone resorption, bone pain, fractures, anemia, and thrombocytopenia are a result of the proliferation of these plasma cells in the bone marrow. In addition, they secrete a detectable abnormal immunoglobulin fragment known as M protein in serum or Bence-Jones protein in urine. Furthermore, these fragments may result in renal disease or amyloidosis [15].
It is important to be aware of common presenting symptoms to allow early diagnosis and management of the myeloma. At presentation, around a third of myeloma patients are asymptomatic. However, during routine examination, some incidental anomalies in renal or blood analysis may be observed [16]. Nonspecific symptoms are commonly reported, such as bone pain, anemia, fatigue, and osteolytic skeletal lesions. At initial diagnosis, extramedullary disease is found in roughly 1–2% of myeloma patients [15]. As proposed by the IMWG, in simple words, a myeloma diagnosis is based on the concentration of clonal plasma cells in the bone marrow (>10%), or a biopsy showing bony or extramedullary plasma cytoma and one or more of the CRAB features that indicate organ damage: hypercalcemia, renal insufficiency, anemia, or bony lesions [6]. Additionally, any one or more of the biomarkers of malignancy, such as a serum-involved/uninvolved light chain ratio of 100 or greater or more than one focal lesion on MRI that is at least 5 mm in size, can support the diagnosis of myeloma. In the current case, the patient had clonal bone marrow plasma cells of around 16% with extramedullary osteolytic bone involvement of the maxilla, and anemia.
According to the Saudi Cancer Registry, 1% of cancer cases in Saudi Arabia are due to myeloma, and the incidence is approximately 1% in males and 0.7% in females [17]. The World Health Organization country profile indicated that, as of 2019, 9.6–11% of cancer-related deaths in Saudi Arabia were attributable to myeloma or lymphoma [18]. Although it is considered a disease of the elderly, with an average age of diagnosis of about 70 years, patients in Saudi Arabia have been diagnosed with myeloma before the age of 50 [18]. Similarly, Kasamatsu et al reported a maxillary swelling as first evidence of myeloma in a 33-year-old Japanese male patient [13]. In addition, the male to female ratio of myeloma is about 1.5 [19]. Reported cases of myeloma patients in Saudi Arabia have a more favorable response to treatment despite being younger, with a worse prognosis, and having a higher disease staging than similarly described populations. The lower myeloma incidence in Saudi Arabia may be attributable to high levels of misdiagnosis and misclassification. Furthermore, due to delayed diagnosis and age, patients are more likely to be offered palliative care as opposed to a referral to a specialized hospital [18]. A myeloma consensus in Saudi Arabia, similar to the IMWG, determined that the diagnostic criteria for multiple myeloma should include more than 10% clonal bone marrow plasma cells or biopsy with evidence of plasmacytoma, either bony or extramedullary. In addition, recognized CRAB symptoms and positivity of 3 specific biomarkers are needed to establish myeloma-defining features [18]. It is crucial to note that the time between the onset of symptoms and diagnosis can be detrimental for hematological malignancies. Importantly, as of 2016, the average time to reach a diagnosis of myeloma was 3–5.5 months, and may extend beyond 12 months [20]. To date, in Saudi Arabia, there are no current data that reliably estimate the average time between initial presentation and diagnosis. Reports of referral to a specialist hematologist/oncologist can extend from 6 months to a year after noticing the initial myeloma symptoms. In the present case, the time between initial diagnosis and start of treatment was 3 months. The length of time before referral in Saudi can be attributed to lack of clarity in the system, making it rather complicated. Distance to the hospital and long waiting lists are also among the most common barriers [18].
As stated, seldom are oral manifestations the first sign of multiple myeloma; 30% of patients develop osteolytic lesions in the jaws and this usually indicates a more advanced disease with extensive skeletal involvement [21]. Nevertheless, in 12% of the cases, the first clinical signs of the disease may be oral manifestations. The most commonly reported oral symptoms of myeloma are intraoral swelling 65%, bone pain 33%, pares-thesia 27%, and amyloidosis 11%. Osteolytic lesions have been detected in 90% of cases, radiographically [22]. As was the case with the current reported patient, intraoral swelling was the main presenting feature. Previous publications, such as those by Kasamatsu et al and Ali et al, also describe gnathic swelling (maxillary and mandibular, respectively) as the first evidence of myeloma in otherwise healthy patients [13,14]. Once the suspicion of myeloma is present, the achievement of diagnosis requires the demonstration of malignant plasma cells histologically, as well as immunohistochemistry analysis to establish clonality. Histologically, myeloma cells show a variety of morphological features, including normal plasma cell morphology and large nuclear pleomorphism [23]. They are classified into 4 types: mature, immature, pleomorphic, and plasmablastic. Plasmablastic myeloma cells are characterized by large size, nuclear polymorphism, and mitotic forms resembling diffuse large B-cell lymphoma. They display increased cellular atypia, and their presence indicates a poor prognosis [24]. Accordingly, 3 cytological features of plasma cells are important: nuclear pleomorphism, cytoplasmic clearing, and high nucleo-cytoplasmic ratio [25]. It is important to distinguish between reactive plasmacytosis and malignant disease. In the present case, sheets of atypical monoclonal plasma cells were seen. This histologic criterion is important for the diagnosis of myeloma, especially since the pattern of infiltration and plasma cell morphology could affect the prognosis of the myeloma [24]. The confirmation of plasma cell monoclonality is mandatory for diagnosing myeloma. The standard for cytogenetic analysis is fluorescence in situ hybridization (FISH) [26]. Conversely, numerical aberrations are highly detectable by single nucleotide polymorphism (SNP)-based mapping arrays and comparative genomic hybridization [27]. Numerous studies have reported a correlation between morphological and morphometrical features of myeloma cells and clinical outcome, including prognosis with clinical stages and survival. Certain features that indicate a worse prognosis include atypical plasma cells, plasma cells constituting more than 15% of cells in the bone marrow aspirate, high levels of B2 microglobulin, and the presence of plasmablastic myeloma cells [28]. Flow cytometry analysis revealed abnormal expression of antigens, including CD56, CD20, CD117, and CD10, in nearly 90% of myeloma cases. The most commonly expressed of these markers is CD56, the presence of which is sufficient for a definitive diagnosis of myeloma and a poor prognosis, whereas CD117 expression correlates with a better prognosis [29]. As reported by Alaskar et al in the Saudi Arabian multiple myeloma consensus, the lack of availability of gene expression profiling, a significant prognostic tool, in Saudi Arabia hinders the identification of a high-risk profile [18,30].
Radiographically, the presence of multiple punched-out osteolytic lesions with no adjacent bone reactions is characteristic of multiple myeloma. The differential diagnosis of myeloma includes bone metastases and other hematopoietic malignancies such as lymphoma and leukemia. The radiographic features, in our case, were the initial drivers of myeloma suspicion, and this truly highlights the importance of an accurate radiologic interpretation and the complete evaluation of the entire CBCT examination. Misdiagnosis of myeloma may result in delayed or inappropriate management, such as root canal therapy; reports have shown a misdiagnosis of periapical inflammatory lesions, odontogenic cysts, and even temporomandibular disorders [30]. Reports about incidental findings on CBCT are common, with the majority being of a benign nature [31]. Price et al reported that 90% of the 300 reviewed CBCT scans contained an incidental finding. An average of 16% required intervention and 15% required monitoring. The authors showed that no incidental discoveries of malignancies were observed in their study, indicating that they are relatively unusual findings [32]. In addition, reports of undiagnosed myeloma discovered incidentally on dental imaging are uncommon [33,34].
Conclusions
This report illustrates the role of CBCT imaging, supported by a multidisciplinary approach, in the diagnosis and management of multiple myeloma. In the current case, a maxillary lesion was the first symptom of myeloma, emphasizing the dentist’s critical role in the detection and early diagnosis of systemic diseases. Although gnathic bones are affected in 30% of the cases, it is rare as the initial presenting feature. Consequently, dental practitioners should be aware of radiographic characteristics and oral manifestations, especially in the elderly, to avoid any delay in management.
Figures
References:
1.. Cardoso RC, Gerngross PJ, Hofstede TM, The multiple oral presentations of multiple myeloma: Support Care Cancer, 2014; 22(1); 259-67
2.. Pushpanshu K, Punyani S, Kaushik R, Mandibular mass as the primary manifestation of multiple myeloma: Braz J Otorhinolaryngol, 2014; 80(3); 266-67
3.. Vinayachandran D, Sankarapandian S, Multiple osteolytic lesions: J Clin Imaging Sci, 2013; 3(Suppl. 1); 6
4.. Fregnani ER, Leite AA, Parahyba CJ, Mandibular destructive radiolucent lesion: The first sign of multiple myeloma: J Clin Exp Dent, 2016; 8(4); e465-68
5.. Rocha TG, Feitosa EF, Maiolino A, Imaginological characterization of multiple myeloma lesions of the jaws through cone-beam computed tomography: Oral Radiol, 2020; 36(2); 168-76
6.. Rajkumar SV, Dimopoulos MA, Palumbo A, International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma: Lancet Oncol, 2014; 15(12); e538-48
7.. Hillengass J, Usmani S, Rajkumar SV, International myeloma working group consensus recommendations on imaging in monoclonal plasma cell disorders: Lancet Oncol, 2019; 20(6); e302-12
8.. Sive J, Cuthill K, Hunter H, Guidelines on the diagnosis, investigation and initial treatment of myeloma: A British Society for Haematology/UK Myeloma Forum Guideline: Br J Haematol, 2021; 193(2); 245-68
9.. Shah A, Ali A, Latoo S, Ahmad I, Multiple myeloma presenting as gingival mass: J Maxillofac Oral Surg, 2010; 9(2); 209-12
10.. Stoopler ET, Vogl DT, Stadtmauer EA, Medical management update: Multiple myeloma: Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2007; 103(5); 599-609
11.. Baykul T, Aydin U, MK OC, Unusual combination of presenting features in multiple myeloma: Dentomaxillofac Radiol, 2004; 33(6); 413-19
12.. Vincent Rajkumar S, Multiple myeloma: 2014 Update on diagnosis, risk-stratification, and management: Am J Hematol, 2014; 89(10); 999-1009
13.. Kasamatsu A, Kimura Y, Tsujimura H, Maxillary swelling as the first evidence of multiple myeloma: Case Rep Dent, 2015; 2015; 439536
14.. Ali IK, Parate AR, Kasat VO, Dora A, Multiple myeloma with primary manifestation in the mandible: Cureus, 2018; 10(3); e2265
15.. Kyle RA, Gertz MA, Witzig TE, Review of 1027 patients with newly diagnosed multiple myeloma: Mayo Clin Proc, 2003; 78(1); 21-33
16.. Smith A, Wisloff F, Samson D, Guidelines on the diagnosis and management of multiple myeloma 2005: Br J Haematol, 2006; 132(4); 410-51
17.. Bazarbashi S, Al Eid H, Minguet J, Cancer incidence in Saudi Arabia: 2012 Data from the Saudi Cancer Registry: Asian Pac J Cancer Prev, 2017; 18(9); 2437-44
18.. Alaskar A, Alsaeed A, Alsharif F, Multiple myeloma in Saudi Arabia: Consensus of the Saudi lymphoma/myeloma group: J Appl Hematol, 2019; 10(2); 37
19.. Abduljalil OZ, Mohiuddin A, Al Hashmi HH: Blood, 2014; 124(21); 5995
20.. Graziani G, Ihorst G, Waldschmidt JM, Time from first symptom onset to the final diagnosis of multiple myeloma – possible risks and future solutions: Large retrospective and confirmatory prospective analysis: Blood, 2016; 128(22); 5979
21.. Raut M, Bansal S, Sharma A, Desai R, Mandibular involvement as a first sign in multiple myeloma: A case report: Braz Dent Sci, 2018; 21(4); 498-503
22.. Almeida TMX, Cavalcanti EFF, Freitas ADS, Can dentists detect multiple myeloma through oral manifestations?: Rev Bras Hematol Hemoter, 2018; 40(1); 43-49
23.. van Marion AMW, Lokhorst HM, van den Tweel JG, Pathology of multiple myeloma: Curr Diagn Pathol, 2003; 9(5); 322-27
24.. Greipp PR, Leong T, Bennett JM, Plasmablastic morphology – an independent prognostic factor with clinical and laboratory correlates: Eastern Cooperative Oncology Group (ECOG) myeloma trial E9486 report by the ECOG Myeloma Laboratory Group: Blood, 1998; 91(7); 2501-7
25.. Hu Y, Chen W, Chen S, Huang Z, Cytogenetic abnormality in patients with multiple myeloma analyzed by fluorescent in situ hybridization: Onco Targets Ther, 2016; 9; 1145-49
26.. Ross FM, Avet-Loiseau H, Ameye G, Report from the European Myeloma Network on interphase FISH in multiple myeloma and related disorders: Haematologica, 2012; 97(8); 1272-77
27.. Sonneveld P, Avet-Loiseau H, Lonial S, Treatment of multiple myeloma with high-risk cytogenetics: A consensus of the International Myeloma Working Group: Blood, 2016; 127(24); 2955-62
28.. Seili-Bekafigo I, Valkovic T, Babarovic E, Myeloma cell morphology and morphometry in correlation with clinical stages and survival: Diagn Cytopathol, 2013; 41(11); 947-54
29.. Pozdnyakova O, Morgan EA, Li B, Patterns of expression of CD56 and CD117 on neoplastic plasma cells and association with genetically distinct subtypes of plasma cell myeloma: Leuk Lymphoma, 2012; 53(10); 1905-10
30.. Chng WJ, Chung TH, Kumar S, Gene signature combinations improve prognostic stratification of multiple myeloma patients: Leukemia, 2016; 30(5); 1071-78
31.. Edwards R, Altalibi M, Flores-Mir C, The frequency and nature of incidental findings in cone-beam computed tomographic scans of the head and neck region: A systematic review: J Am Dent Assoc, 2013; 144(2); 161-70
32.. Price JB, Thaw KL, Tyndall DA, Incidental findings from cone beam computed tomography of the maxillofacial region: A descriptive retrospective study: Clin Oral Implants Res, 2012; 23(11); 1261-68
33.. Biun J, Lok V, Koong B, Huang TC, A significant incidental finding on cone beam computed tomography: Multiple myeloma: Aust Dent J, 2019; 64(3); 293-96
34.. Lae ME, Vencio EF, Inwards CY, Myeloma of the jaw bones: A clinicopathologic study of 33 cases: Head Neck, 2003; 25(5); 373-81
Figures
Tables
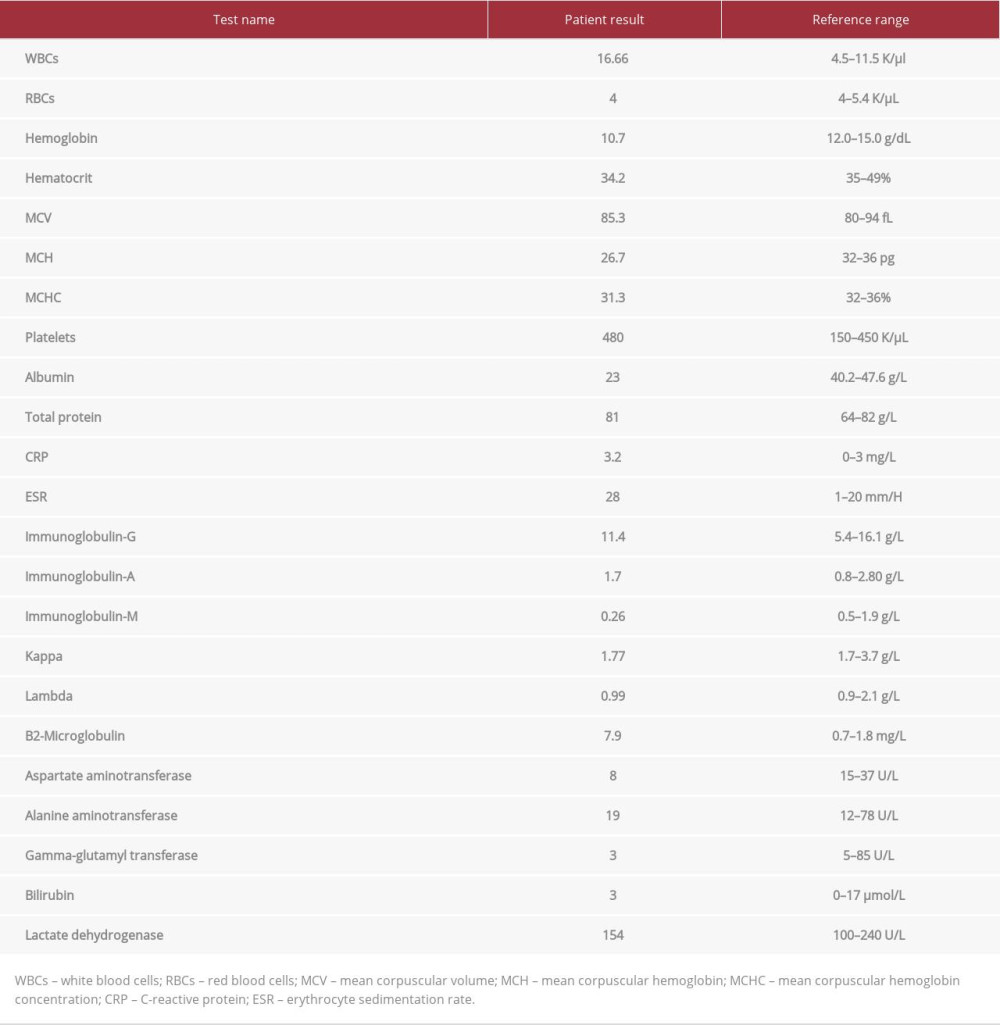 Table 1.. Laboratory investigations at the time of initial diagnosis.
Table 1.. Laboratory investigations at the time of initial diagnosis.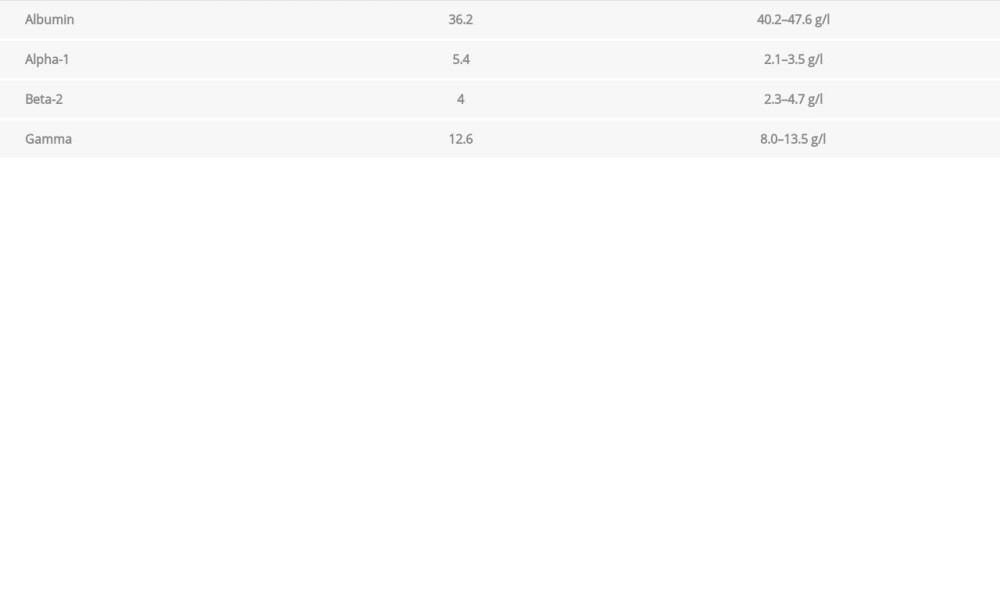 Table 2.. Protein electrophoresis at the time of initial diagnosis.
Table 2.. Protein electrophoresis at the time of initial diagnosis. Table 3.. Bone function profile at the time of initial diagnosis.
Table 3.. Bone function profile at the time of initial diagnosis.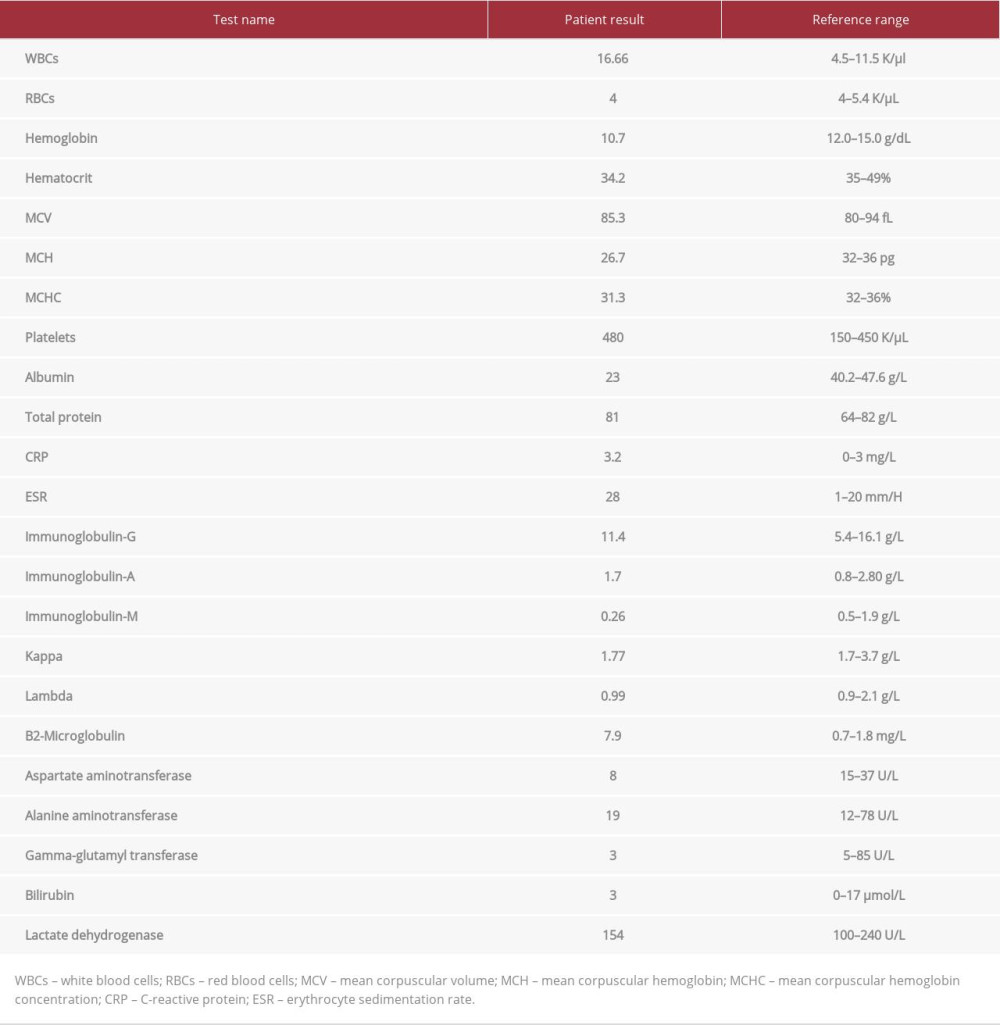 Table 1.. Laboratory investigations at the time of initial diagnosis.
Table 1.. Laboratory investigations at the time of initial diagnosis.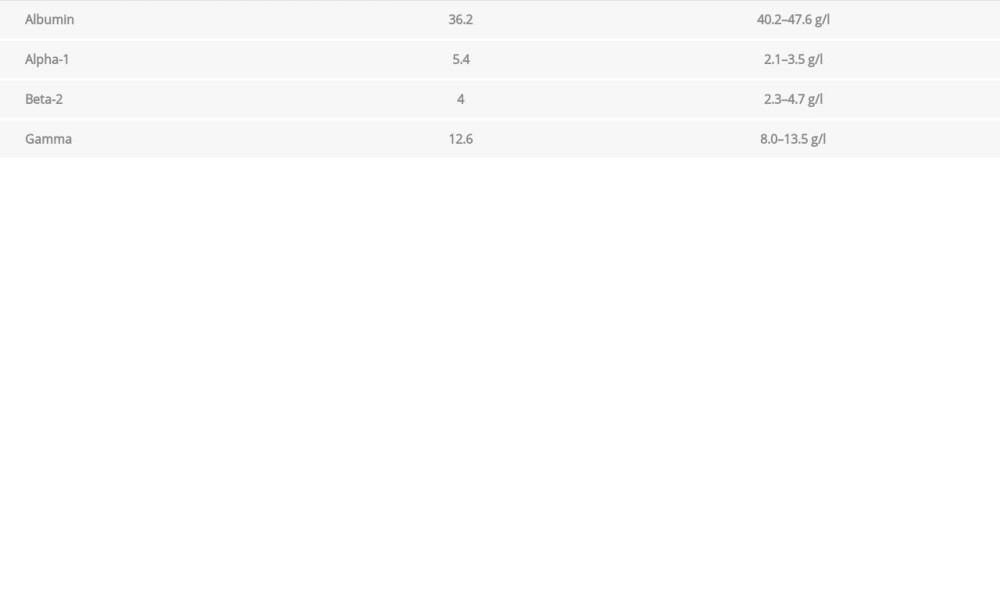 Table 2.. Protein electrophoresis at the time of initial diagnosis.
Table 2.. Protein electrophoresis at the time of initial diagnosis. Table 3.. Bone function profile at the time of initial diagnosis.
Table 3.. Bone function profile at the time of initial diagnosis. In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








