10 June 2023: Articles 
Diagnostic Dilemma in a Case of Lyme Borreliosis Presenting as Severe Anion Gap Metabolic Acidosis: A Case Report
Unusual clinical course, Challenging differential diagnosis, Rare coexistence of disease or pathology
Lindsey A. Wallace1ABDEF*, Sarah Cullison1AE, Jacob Bowdon1BCDEF, Aditya Shah2DE, Sumera Ahmad3ADEFDOI: 10.12659/AJCR.939196
Am J Case Rep 2023; 24:e939196
Abstract
BACKGROUND: Lyme disease is a common tickborne disease with a common presentation. Untreated Lyme disease can affect other organs. This can lead to anion gap metabolic acidosis through severe renal failure. Unlike anion gap metabolic acidosis, osmolar gap can be caused by ingestion of ethanol, toxic alcohols, solvents, and salicylates. Therefore, a presentation with osmolar gap and anion gap metabolic acidosis yields a variety of differential diagnoses.
CASE REPORT: A 72-year-old man presented after being found down. There were few historical cues, and workup was negative for seizures or any acute cerebrovascular incident. Laboratory results were revealing of severe anion gap acidosis with osmolar gap. During clinical decision making and diagnostic dilemma, toxidrome syndromes for potential ingestions and inhalations were sought in addition to thorough workup, which expanded to include infectious etiologies. This patient’s presentation was unique: Lyme disease in the setting of severe anion gap metabolic acidosis with an osmolar gap.
CONCLUSIONS: The outcome of critically ill patients can be determined by the clinician’s method to address the diagnostic dilemma and quality of supportive care. Critically ill patient outcomes can be subject to the clinician’s method to address a diagnostic quandary. This unique case poses an important reminder for clinicians to maintain their standard methodologies of critical thinking amidst the noise of distracting medical information.
Keywords: Acidosis, Critical Care, Infectious Disease Medicine, Lyme Disease, Neurotoxicity Syndromes, Male, Humans, Aged, Acid-Base Equilibrium, Critical Illness, Ethanol
Background
Tickborne illnesses such as Lyme disease have higher incidences in the northeastern and midwestern areas of the United States [1,2]. Tickborne infections typically present as a febrile illness with headache, fatigue, and myalgias [1–4]. In the initial 3 to 30 days, the symptoms of Lyme disease are similar to those of other tickborne diseases, but also include first-degree atrioventricular (AV) nodal block, lymphadenopathy, and erythema migrans rash [5]. After a month of exposure, severe symptoms include facial palsy, arthritis, meningitis, and paresthesias [5]. Patients with Lyme neuroborreliosis have demonstrated cranial neuropathy, lymphocytic pleocytosis, and radiculopathy, a triad that has been identified as Bannwarth syndrome [6]. A previous case report demonstrated neurological changes, presumably from chronic Lyme disease treatment [7]. Antibodies for Lyme can take weeks to develop and can remain for years after active infection is gone [5]. Polymerase chain reaction (PCR) testing for Lyme in the cerebral spinal fluid (CSF) has low sensitivity and should not be used to exclude the diagnosis [8]. CSF analysis can demonstrate elevated protein, lymphocytic pleocytosis, and increased IgG antibody index of CSF to serum for
Acute renal failure can cause anion gap metabolic acidosis and potentially, osmolar gap acidosis. However, typical etiologies for an osmolar gap include methanol, ethylene glycol, diethylene glycol, propylene glycol, or isopropanol [9]. In addition to renal failure, osmolar gap in the setting of anion gap metabolic acidosis could be attributed to diabetic or alcoholic ketoacidosis, chronic kidney disease, or lactic acidosis [9]. This case report presents a uniquely complex critically ill patient with Lyme disease that presented as severe metabolic acidosis with anion gap. The aim of this report is to demonstrate the importance of differential methodology to address a diagnostic dilemma in critically ill patients amidst the noise of distracting medical information.
Case Report
The patient was a 72-year-old man who presented to the hospital for altered mental status and subsequent coma. He had a history of hypertension, sensorineural hearing loss, and a recent episode of generalized weakness and presumed transient ischemic attack 1 week prior, without residual deficits. He was not on any home medications. History was obtained by his wife, owing to his mental status. His wife denied history of tobacco, alcohol, or illicit drug use. He lived in a highly endemic area of the Midwest and lived in a rural, wooded setting. A few days prior to admission, he had been working in the brush, and the day of admission, had been cleaning mold from his garage without any solvents or chemical cleaners.
That night he woke up altered, had an episode of urinary incontinence, and became unconscious, at which time his family called Emergency Medical Services. He did not have any witnessed tremors or neurological changes. He was not witnessed to be inhaling or ingesting substances.
Upon arrival at the Emergency Department, he had bradycardia, with a heart rate of 54 beats per min and a first-degree atrioventricular (AV) block, and had hypertension, with a blood pressure of 223/54 mmHg. He had hypothermia, at 33.4°C. No focal neurologic deficits were identified, and he had a low Glasgow Coma Scale of 6 and profound metabolic acidosis (pH of 6.9), for which he was intubated. There was initial concern for seizures, for which he was treated with levetiracetam. Head computed tomography (CT) was unremarkable for acute intracranial changes. Ultimately, given concern for seizure, he was transferred to the neurological Intensive Care Unit (ICU).
In the neurological ICU he was treated with a rewarming protocol for hypothermia. He was initially normotensive, but still had bradycardia. Spot electroencephalogram (EEG) and continuous EEG off sedation were both unremarkable for seizure activity. He remained comatose. A brain magnetic resonance image showed no acute infarct or restricted diffusion (Figure 1). Initial abnormal laboratory values are shown in Table 1; there was no obvious cause of encephalopathy aside from metabolic encephalopathy. Notable laboratory results on admission in the normal range included blood urea nitrogen, creatinine, hemoglobin, international normalized ratio, and beta hydroxy-butyrate. Since the patient did not appear to have a primary neurological condition, he was transferred to the medical ICU.
He remained bradycardic but developed hypertension, with systolic blood pressures 200 mmHg, requiring clevidipine infusion. Due to his significant lactic acidosis, a CT angiogram of the abdomen and pelvis was obtained and was negative for mesenteric ischemia. He was started on empiric broad spectrum antibiotics for an unclear source of infection, after negative urine studies and chest X-ray and no obvious skin source. Given his osmolar gap, leukocytosis, and unresponsive mental status, a lumbar puncture was performed (Table 2). An encephalopathy, autoimmune/paraneoplastic evaluation was unremarkable. A repeat brain magnetic resonance image also showed no acute intracranial abnormalities (Figure 2).
With his clinical presentation resulting in coma, cyanide toxicity and solvent ingestions were considered [11]. For possible cyanide toxicity, he was administered hydroxocobalamin, and for possible solvent ingestion, he was empirically given formaldehyde.
However, it was later found that his urine drug, volatile, and heavy metal screening tests were negative. However, given his profound acidosis with severe electrolyte derangements, he underwent 1 run of intermittent hemodialysis, with improvement in his metabolic profile. He started to wake up, with some encephalopathy, but ultimately self-extubated on day 3 of hospitalization. His creatinine level continued to trend up to 3.67 mg/dL by day 2 of hospitalization, but he did not require further dialysis, as his electrolytes remained stable, with adequate urine output.
Studies returned from the CSF after 30 h were positive for Lyme IgM and IgG; however, the Lyme antibody index was within the reference range, indicating that this was Lyme disease, not Lyme neuroborreliosis. Additional negative serum PCR tests included
Discussion
This case demonstrates a diagnostic dilemma of a common disease with an unusual presentation. Although clinicians can be faced with a plethora of distracting medical data, this case highlights that patient outcomes are associated with careful differential methodology by clinicians. The profound metabolic acidosis with a pH of 6.94 and bicarbonate level of 7 mmol/L on venous blood gas in the setting of an anion gap of 27 and osmolar gap of 20 mOsm/kg suggested a differential of potential causes to include glycol intoxication, oxoproline toxicity, L-lactate, D-lactate, methanol, aspirin, renal failure, and ketoacidosis. Ethylene and propylene glycol were negative, acetaminophen and salicylate levels were negative, methanol level was negative, and the patient did not have any ketones in his urine to suggest ketoacidosis. The lactate level and white blood cell count were rising, but after initial intensive care management, including broad spectrum antibiotics, intravenous fluids, and hemodialysis, the lactate level normalized, as well as the leukocytosis. The source of the patient’s anion gap metabolic acidosis seems to be most related to renal failure in the setting of an uncovered tickborne infection.
Despite the patient’s initial presentation of hypothermia, he was harboring Lyme disease, which is traditionally associated with fever [2]. Upon collection of the tickborne panel, the patient’s wife noted that he often spent time outdoors. This patient had a reactive IgG antibody in the CSF for
We retrieved 1 case report related to Lyme disease presenting with severe metabolic acidosis with anion gap. This case demonstrated a similar metabolic presentation, but was from known chronic Lyme disease, which was actively being treated [7]. However, although the patient was altered on presentation, since he was being treated for chronic Lyme disease, his diagnosis was already established to guide a differential diagnosis more specifically. That patient also developed neurological deficits, which were appreciated on brain imaging. In contrast, the patient in our case was unable to provide a history on presentation and did not have a known history of Lyme disease or specific signs on presentation to suggest Lyme disease. Therefore, not only was this case unique in the setting of acute Lyme disease with severe anion gap metabolic acidosis with profound altered mentation without intracranial changes on imaging, the diagnostic dilemma of differentiating the plethora of medical data adds to the uniqueness of this case. The initial presentation widens the possibilities for differentials that can distract from a common illness such as Lyme disease.
When clinicians obtain an abundance of data, they can develop cognitive overload that can distract from the typical approach to differential diagnosis. In the present case, the differential diagnosis based on distractors included (1) previous evaluation for transient ischemic attack prior to presentation could suggest primary neurological issue; (2) comatose state with no obvious story to suggest inhalation or ingestion; (3) osmolar gap metabolic acidosis, which more commonly coincides with toxicological etiologies; (4) the patient improved with initial round of dialysis and near simultaneous administration of hydroxocobalamin for possible cyanide poisoning; and (5) positive serologies for IgG and IgM Lyme antibodies that resulted after the previous 4 distractors were already in process. Objectively, the patient presented with an anion gap and osmolar gap metabolic acidosis. Drug screening tests were negative, and there was no history of ingestion or inhalation of foreign substances. While it is possible the patient ingested or inhaled something to explain his osmolar gap, it is less likely given his history and laboratory results.
Conclusions
Ultimately, the patient presented with an interesting version of Lyme disease with both osmolar and anion gap metabolic acidosis. A patient’s history is an important piece of information, in addition to signs and symptoms, to develop a diagnosis, and when this is unable to be obtained due to altered mentation on presentation, it is crucial to seek collateral information. The outcome of critically ill patients can be determined by the clinician’s method to address the diagnostic dilemma and quality of supportive care. This unique case poses an important reminder for clinicians to maintain their standard methodologies of critical reasoning despite the temptation of distracting medical information.
Figures
References:
1.. , Center for Disease Control and Prevention Reviewed January 19, 2022. Available from: [Accessed June 22, 2022]https://www.cdc.gov/lyme/
2.. , Center for Disease Control and Prevention Reviewed August 6, 2021. Available from: [Accessed June 22, 2022]https://www.cdc.gov/anaplasmosis/index.html
3.. Aguero-Rosenfeld ME, Horowitz HW, Wormser GP, Human granulocytic ehrlichiosis: A case series from a medical center in New York State: Ann Intern Med, 1996; 125(11); 904-8
4.. Ismail N, McBride JW, Tick-borne emerging infections: Ehrlichiosis and anaplasmosis: Clin Lab Med, 2017; 37(2); 317-40
5.. Schoen RT, Lyme disease: Diagnosis and treatment: Curr Opin Rheumatol, 2020; 32(3); 247-54
6.. Shah A, O’Horo JC, Wilson JW, An unusual cluster of neuroinvasive Lyme disease cases presenting with bannwarth syndrome in the midwest United States.: Open Forum Infect Dis, 2018; 5(1); ofx276
7.. Frankl S, Hadar PN, Yakhkind A, Devastating neurological injury as a result of treatment of “chronic Lyme disease.”: Mayo Clin Proc, 2021; 96(7); 2005-7
8.. Nocton JJ, Bloom BJ, Rutledge BJ: J Infect Dis, 1996; 174(3); 623-27
9.. Kraut JA, Xing SX, Approach to the evaluation of a patient with an increased serum osmolal gap and high-anion-gap metabolic acidosis: Am J Kidney Dis, 2011; 58(3); 480-84
10.. Marts LT, Hsu DJ, Clardy PF, Mind the gap: Ann Am Thorac Soc, 2014; 11(4); 671-74
11.. Hendry-Hofer TB, Ng PC, Witeof AE, A review on ingested cyanide: Risks, clinical presentation, diagnostics, and treatment challenges: J Med Toxicol, 2019; 15(2); 128-33
12.. McFee RB, Tick borne illness: Anaplasmosis.: Dis Mon, 2018; 64; 181-84
Figures
Tables
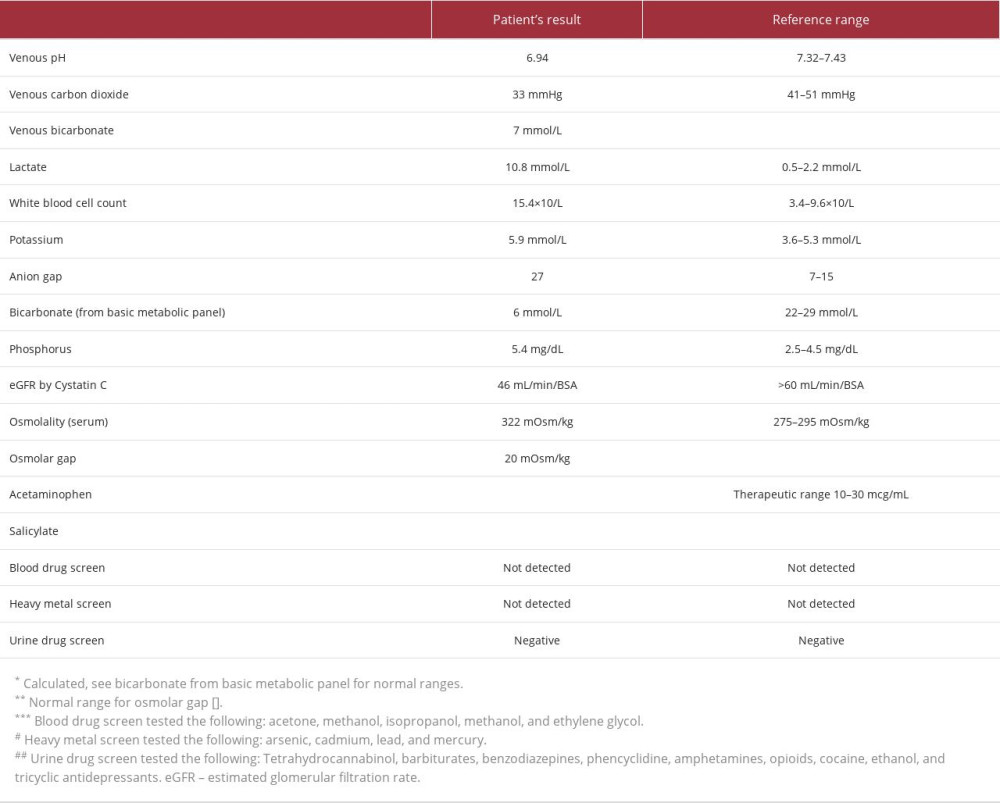 Table 1.. Pertinent abnormal laboratory values on day of admission.
Table 1.. Pertinent abnormal laboratory values on day of admission.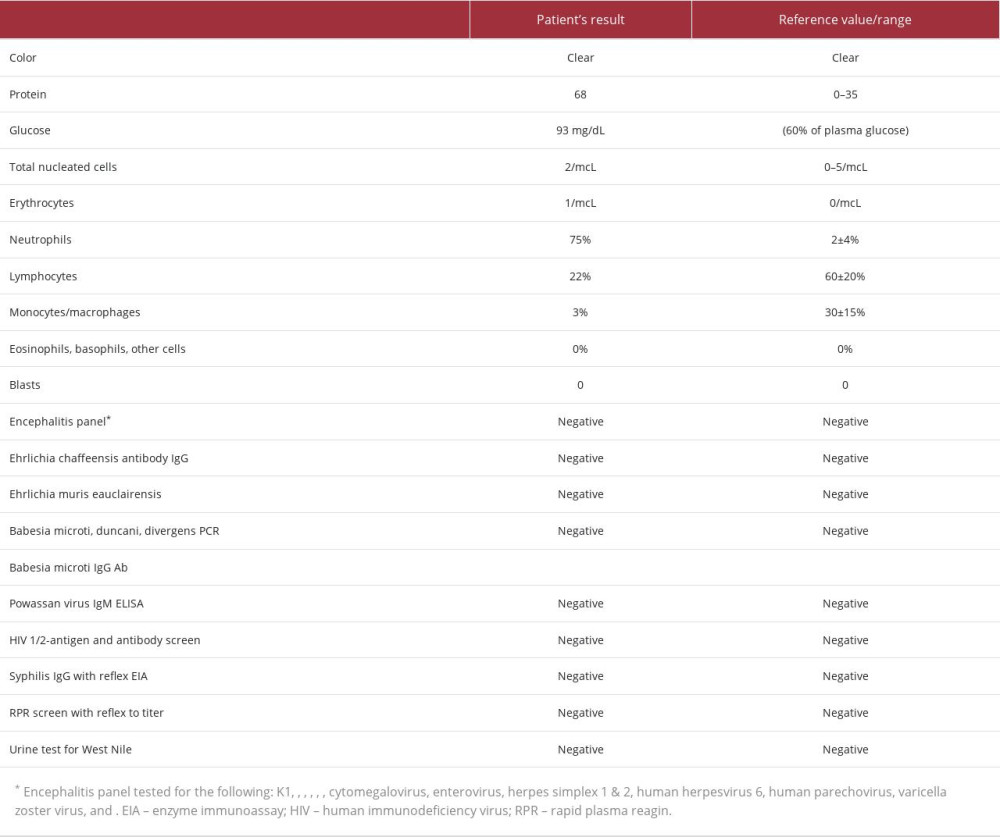 Table 2.. Cerebrospinal fluid analysis from lumbar puncture.
Table 2.. Cerebrospinal fluid analysis from lumbar puncture.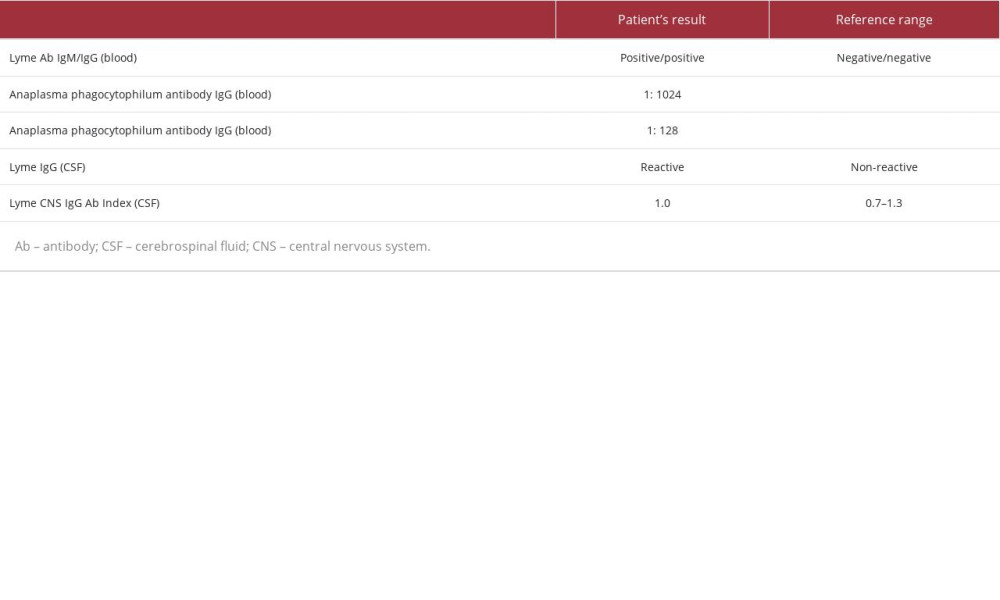 Table 3.. Tickborne laboratory results.
Table 3.. Tickborne laboratory results.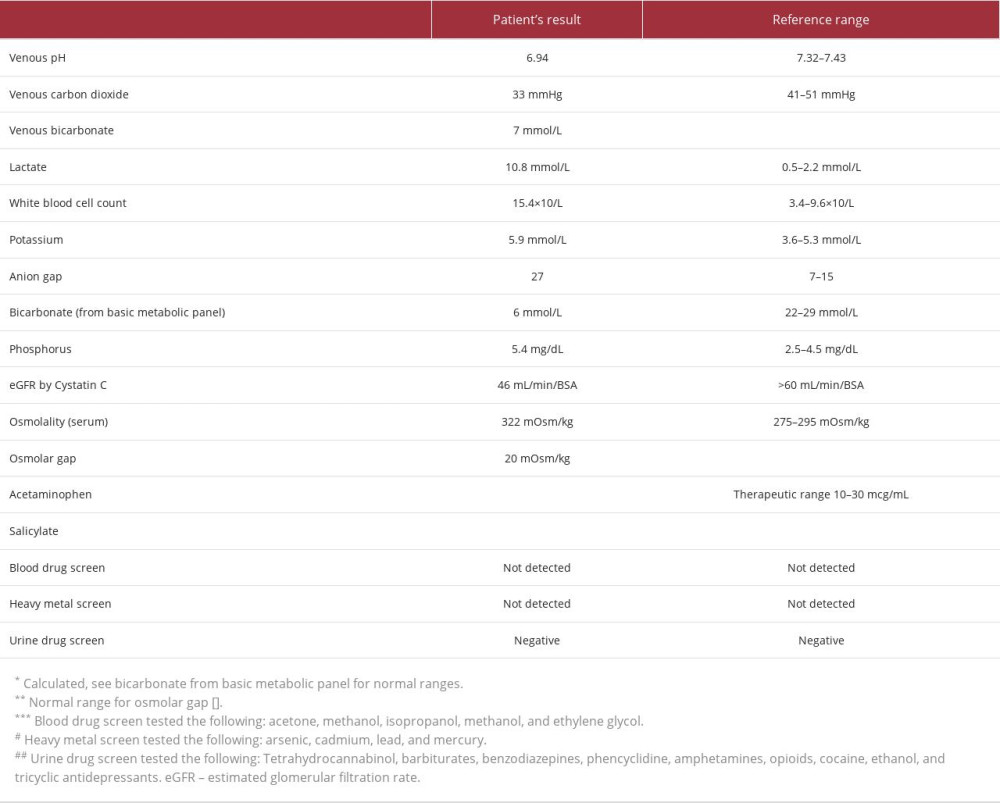 Table 1.. Pertinent abnormal laboratory values on day of admission.
Table 1.. Pertinent abnormal laboratory values on day of admission.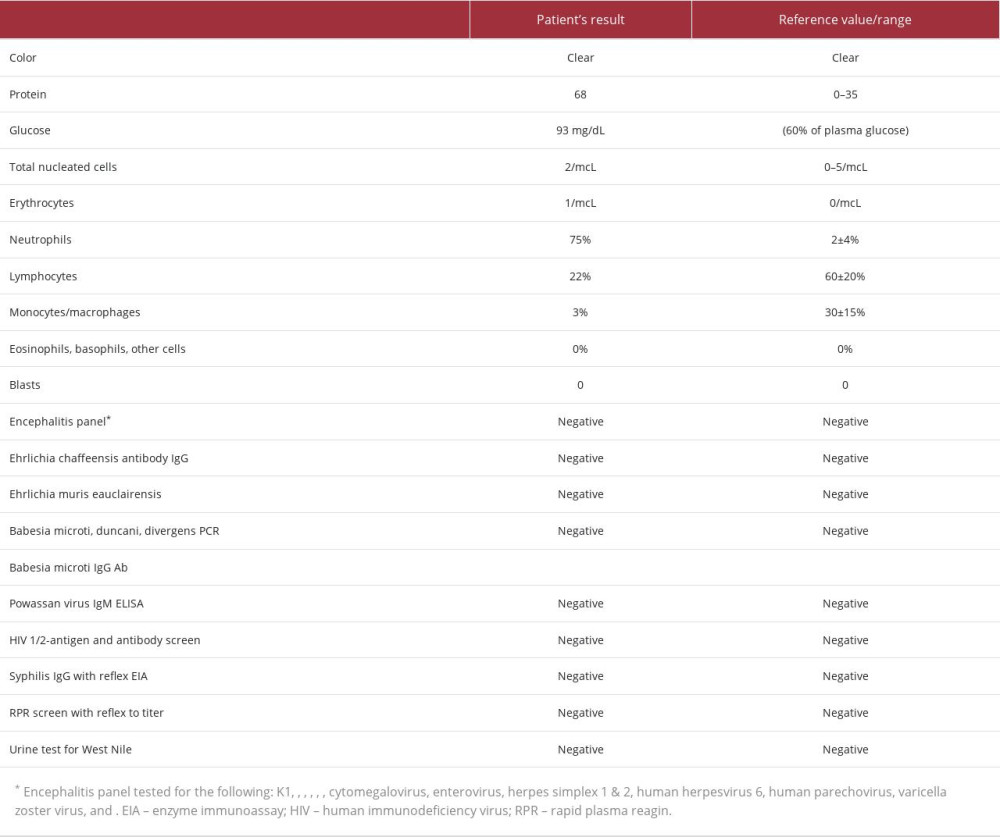 Table 2.. Cerebrospinal fluid analysis from lumbar puncture.
Table 2.. Cerebrospinal fluid analysis from lumbar puncture.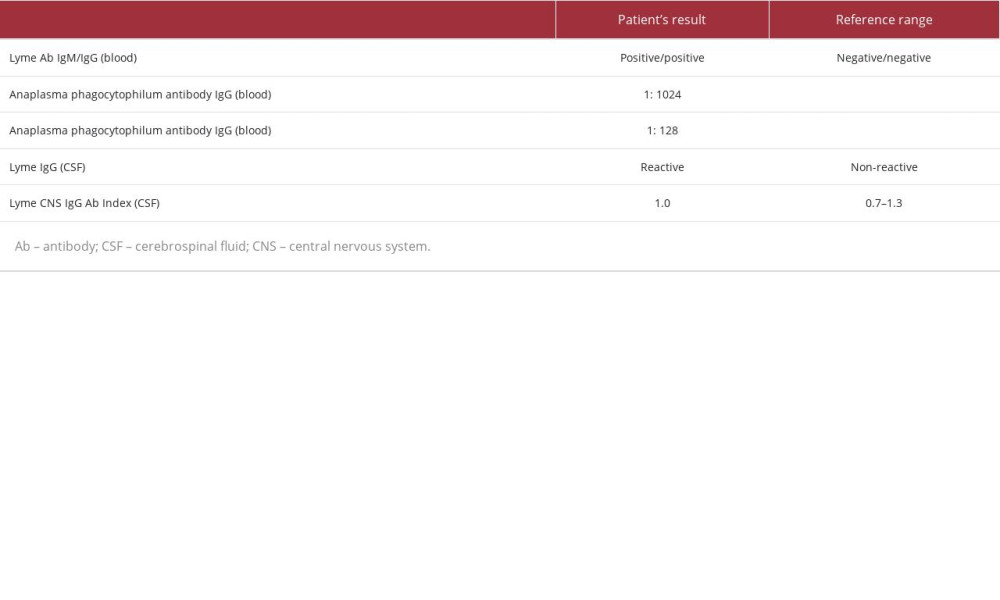 Table 3.. Tickborne laboratory results.
Table 3.. Tickborne laboratory results. In Press
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943645
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942921
22 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943346
24 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943560
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








