14 November 2023: Articles 
A Rare Case of Acute Myocardial Infarction in Pregnancy: Successful Treatment Strategies
Management of emergency care, Rare disease
Paweł Andrzej Zieliński12ACDG, Łukasz Gawlik3EF, Joanna KrupińskaDOI: 10.12659/AJCR.940790
Am J Case Rep 2023; 24:e940790
Abstract
BACKGROUND: Acute myocardial infarction during pregnancy is rare, but is associated with a high mortality rate, particularly during labor and delivery. This article concerns a 23-year-old woman with a history of insulin-treated gestational diabetes and hypothyroidism treated with levothyroxine presenting at 32 weeks of pregnancy with acute chest pain and coronary artery occlusion requiring angioplasty followed by cesarean delivery. The aim of this report is to outline the diagnostic difficulties of acute coronary syndromes during pregnancy and to present their treatment.
CASE REPORT: A 23-year-old female patient at 32 weeks’ gestation treated for insulin-dependent diabetes mellitus and hypothyroidism was admitted to the hospital due to acute chest pain. The ECG showed ST-segment elevation in leads I, aVL, and V4-V6 and elevated troponin T. Based on this, the patient was diagnosed with myocardial infarction and given low-molecular heparin, followed by primary coronary angioplasty with revascularization. After the procedure, she received dual antiplatelet therapy (DAPT) with acetylsalicylic acid and clopidogrel. The pregnancy was terminated at 38 weeks by cesarean section, delivering a healthy baby.
CONCLUSIONS: This report shows the importance of rapid and accurate diagnosis and management of acute myocardial infarction during pregnancy, and delivery by cesarean section, to ensure survival of the mother and the child.
Keywords: acute coronary syndrome, Myocardial Infarction, Pregnancy Complications, Cardiovascular, Angioplasty, case reports
Background
The main causes of death in Poland are cardiovascular diseases and cancer. They affect more than 70% of deaths [1]. Cardiovascular diseases affect women much more often than men, with a slightly higher mortality rate than in men [1]. Among cardiovascular diseases, ischemic heart disease, including myocardial infarction, has been the cause of the highest number of deaths for many years. Cardiovascular diseases mainly affect older people, aged 65 and over [2]. The cause of myocardial infarction is sudden closure of one of the coronary arteries supplying blood to the heart muscle. Acute ischemic necrosis develops in this area. The most common symptom of acute myocardial infarction is severe, sudden, diffuse pain behind the sternum. It may be described as a squishing pain or characterized by pressure, very often with radiation to the shoulders, throat, jaw, or abdomen [2]. Acute myocardial infarction during pregnancy or in the postnatal period is extremely rare (3 to 10 cases per 100 000 births) [3,4]. It complicates 0.4–4% of all pregnancies and is associated with a mortality rate of 5.1% up to 37% [5]. Maternal deaths most often occur during the course of a myocardial infarction and up to 2 weeks afterwards, mainly due to delivery. The percentage of fetal deaths ranges from 12% to 34% of cases, with the majority caused by death of the mother [3,6]. Survival of the mother usually results in a good prognosis for the fetus [5]. Myocardial infarction can occur at any stage of pregnancy and is becoming more common over time. The incidence of coronary artery disease (CAD) in pregnant women has increased in recent years [7].
Risk factors for myocardial infarction include classical risk factors such as hypertension, diabetes, dyslipidemia, and smoking [2,6] and risk factors directly related to pregnancy. Pregnancy itself increases the risk of CAD due to hemodynamic changes in the cardiovascular system [8]. There is also an increase in estrogen and progesterone level, which, when administered orally (eg, with hormone replacement therapy) increase the risk of coronary heart disease [9]. Diagnosis of acute coronary syndrome in pregnancy is difficult and carries a high risk for the fetus [5]. The use of minimally invasive examinations such as vital signs monitoring, laboratory tests, and electro- and echo-cardiographic diagnostics should be considered first [3,5] The use of X-ray imaging should be considered on the basis of the balance of benefits and losses due to its teratogenic effects [3]. During treatment, the care of a multidisciplinary team comprising gynecologists, internists, cardiologists, and anesthetists is important. The treatment process includes all therapeutic methods as in the general population, including the use of revascularization methods. Among the drugs used for therapy are acetylsalicylic acid (ASA) and clopidogrel, but only when necessary and for the shortest possible time [10]. The use of P2Y12 receptor inhibitors such as ticagrelor or prasugrel is not recommended due to the lack of data on their use in pregnant patients. During cardiovascular interventions, it is important to keep the dose of ionizing radiation as low as possible [10]. After recovery from myocardial infarction, delivery should be performed at least 2 weeks after the incident, if possible [5]. The type of delivery should be chosen based on the determination of which route will provide less hemodynamic burden. In literature reviews, the mortality rate for women in vaginal deliveries was 14%, while for cesarean sections it was 23% [6]. The present report concerns a 23-year-old woman with a history of gestational diabetes on insulin and hypothyroidism treated with levothyroxine presenting at 32 weeks of pregnancy with acute chest pain and coronary artery occlusion requiring angioplasty followed by cesarean delivery.
Case Report
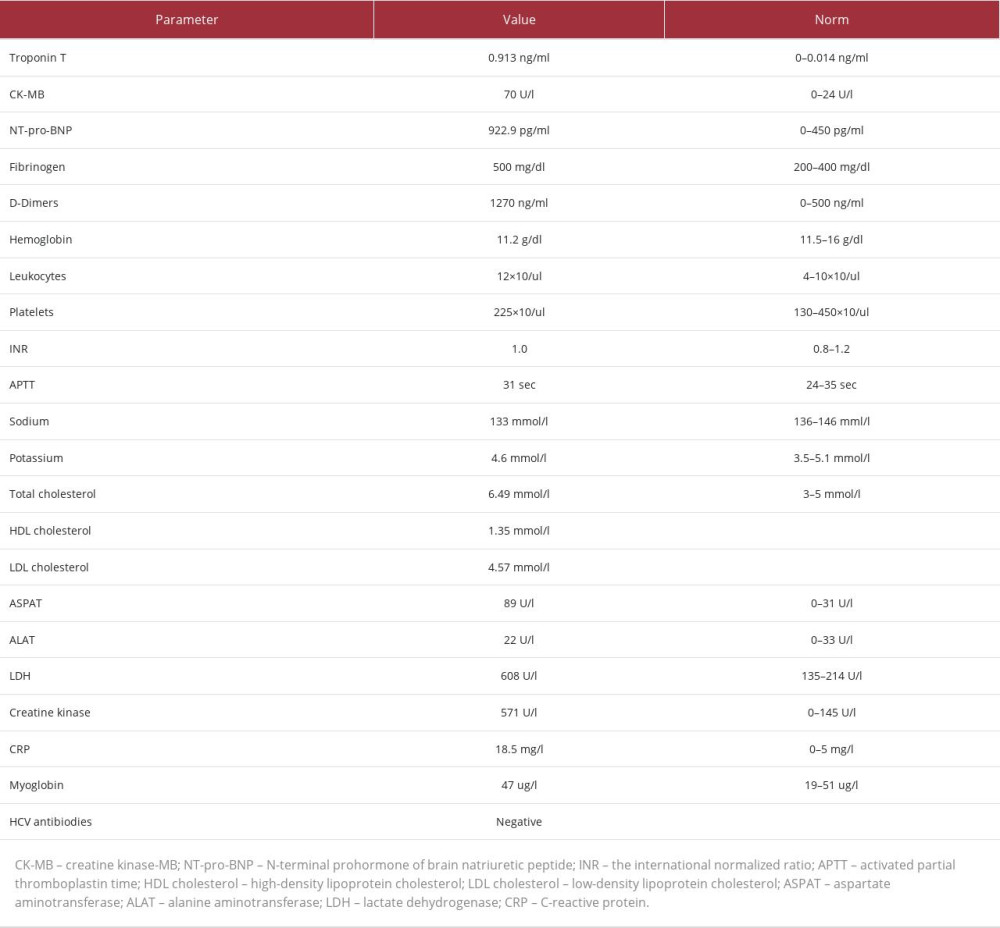
A 23-year-old patient with a first pregnancy (32 weeks) was brought by the Medical Rescue Team to the Pregnancy Pathology Department of the Provincial Specialist Hospital in Biała Podlaska from one of the Public Health Care Centres in the Lubelskie Voivodeship. She was hospitalized at the above-mentioned hospital because of fainting, shoulder pain, and numbness in her hands that occurred after lifting a heavy object. After 2 days in the Obstetrics-Gynaecology and Pregnancy Pathology Unit in the Public Health Care Centre, she was referred and transferred to the Pregnancy Pathology Ward of the Provincial Specialist Hospital (Wojewódzki Szpital Specjalistyczny [WSzS]) in Biała Podlaska with the diagnosis suspected myocarditis. On admission, she reported having chest pain. Her history included gestational diabetes (treated with insulins) and hypothyroidism (levothyroxine supplementation 150 ug 1-0-0). Her family history was nonsignificant, as was other history information. Immediately after admission to the Pregnancy Pathology Unit in WSzS, laboratory tests were ordered (Table 1).
Subsequently, ultrasound examination of the fetus was performed. An electrocardiogram (ECG) was performed and an urgent cardiology consultation was ordered. In the assessment of the on-call cardiologist, the ECG showed a sinus rhythm of approximately 94/min. ST-segment elevation >1 mm in the leads: I, aVL, V4–V6, meeting the criteria for the diagnosis of ST-elevation myocardial infarction of the lateral wall and apical infarction (Figure 1). Hospitalization in the Invasive Cardiology Unit was recommended. An echocardiogram was performed, which showed akinesis of the apical segment of the lateral wall. Therefore, the patient was urgently qualified for coronary angiography, which revealed occlusion of the middle part of the diagonal artery, and coronary angioplasty of the above-mentioned artery with predilatation was performed (Figures 2–4). An Onyx 2.0×18 mm stent was implanted. Enoxaparin was ordered in preparation for the percutaneous coronary angioplasty procedure. A follow-up ECG was performed 10 hours after these procedures (Figures 5, 6), showing a sinus rhythm of approximately 100/min, ST-elevation of Pardee wave type in leads I, aVL, V3–V6 with reduction of R-wave and developed Q-waves in these leads, indicating evolution of a lateral wall/ apical myocardial infarction.
Dual antiplatelet therapy (DAPT) with acetylsalicylic acid (ASA) and clopidogrel was started after percutaneous coronary interventions (PCI). On the sixth day after the above-described procedures, the patient was transferred to the Pregnancy Pathology Department with appropriate recommendations. The pregnancy was delivered between 38 and 39 weeks by cesarean section. Clopidogrel and low-molecular-weight heparin were temporarily discontinued in preparation for cesarean section. A healthy, full-term male infant was delivered, weighing 3260 g. The course of the puerperium observed in the Obstetric Unit was normal. On the third day after the cesarean section, the patient was discharged from the Obstetric Unit in good general condition with many recommendations. The patient has been feeling well for more than a year after cardiovascular and obstetric procedures and is under constant cardiac care (ASA 25 mg 1-0-0; Clopidogrel 75 mg 1-0-0; Metoprolol 25 mg 1-0-0; Insulin aspart 3 IU 1-0-0; Human insulin 23IU 0-0-1; and Levothyroxine 150 ug 1-0-0), and actively participates in volleyball twice a week. The diagnostic and treatment procedures that our patient underwent were consistent [10] with the ESC guidelines for the management of cardiovascular disease in pregnancy (2018).
Discussion
This report shows the correct management of a myocardial infarction in a pregnant woman and presents the diagnosis as it should be undertaken to clarify the causes of this disease in a young person. Any premature myocardial infarction requires extended diagnostics to determine the reason for its occurrence. Patients must undergo a detailed diagnostic workup to detect risk factors or concomitant diseases. Initially, the patient’s risk factors should be identified starting with the classic factors: dyslipidemia, diabetes, and hypertension. A detailed medical history is then established. Previous myocardial infarctions, strokes, heart failure, or arrhythmias are important in the history [11]. Additionally, in men, attention should be paid to erectile dysfunction. A thorough history of past infectious diseases (eg, HIV, chlamydia, tuberculosis, COVID-19) should be taken. Another potential cause that needs to be ruled out could be immune-mediated inflammatory diseases such as vasculitis or connective tissue inflammation [12]. Symptoms such as morning stiffness, joint pain, and aphthae in the mouth or on the genitals should be inquired about. In addition, the presence of cancers currently or in the past should be taken into account. It is very important that in a young person with myocardial infarction, the coagulation and fibrinolysis status should be assessed for possible thrombophilias (congenital or acquired), particularly in the case of unaltered coronary arteries on coronary angiography [12]. The possibility of atrial fibrillation, valvular heart defects, or infective endocarditis should also be borne in mind. The presence of cardiomyopathy and diagnosis for metabolic storage diseases is also important [13]. In addition, attention should be paid to the presence of triggers such as drugs, an excessive emotional response that may suggest takotsubo syndrome, or prolonged immobilization predisposing to venous thrombosis. Among the tests that may be performed in these patients are: lipid profile (including lipoprotein A), biochemical tests (transaminases, creatinine, albumin, uric acid, HbA1c, electrolytes, TSH, hemoglobin, platelets), tests to assess thrombophilia (laboratory fibrinogen, homocysteine, vitamin B12, folic acid, Protein C and S, and antithrombin III), and genetic tests such as factor V Leiden, prothrombin mutation, or Apo E polymorphism [14]. Immunological markers such as CRP, antinuclear antibodies, antiphospholipid antibodies, and anticardiolipin antibodies should also be determined [12,13]. In our patient, a full diagnosis of the causes of the infarction based on the above-mentioned tests was not made, as the hospital where she was staying did not have adequate diagnostic facilities. The patient was advised to undergo further diagnostics, but she did not continue treatment at our hospital; therefore, we were unable to obtain information on the follow-up. Regardless of a pregnant woman’s ‘classic’ coronary risk factors, it is important to remember that a common cause (43%) of myocardial infarction in young women both during pregnancy and in the postpartum period is spontaneous coronary artery dissection (SCAD) [15,16]. In the present era of widespread access to coronary angiography, such cases are increasingly being diagnosed, mainly in young women. It is estimated that SCAD may account for approximately 0.3–1.2% of all acute coronary syndromes [17]. Underlying disease may be a previously unidentified connective tissue disease, the stress and strain of childbirth, and the use of uncommon hormonal therapy [17]. If the angiographic picture is unclear in such a patient, coronary ultrasound (IVUS) may be helpful. A conservative strategy is preferred, with follow-up angiography approximately 1 month apart. Once again, it is worth emphasizing that acute myocardial infarction can occur at any stage of pregnancy and childbirth [3]. The prognosis becomes better when appropriate management is initiated as soon as possible. Currently, about half of pregnant women with acute myocardial infarction require coronary angiography followed by percutaneous coronary intervention. This type of patient requires multidisciplinary care involving an experienced multidisciplinary team (obstetricians, cardiologists, and GPs) [10]. In their paper, Michaelis et al [18] described the case of a 37-year-old patient in a 24-week twin pregnancy who was diagnosed with myocardial infarction. After the diagnosis, the patient received antiplatelet treatment consisting of ASA and clopidogrel followed by coronary angiography with stent placement. This pregnancy was terminated by cesarean section at 35 weeks, giving birth to 2 healthy babies. Sun et al [19] described the case of a 41-year-old woman at 31 weeks’ gestation with symptoms and clinical findings indicative of acute coronary syndrome, who also underwent coronary angiography, with closure of the occluded vessel. The pregnancy was terminated by cesarean section at 34 weeks’ gestation. Both the diagnostic process and the applied treatment of myocardial infarction and termination of pregnancy in the above cases correspond to the description of our patient. On the other hand, Argentiero et al [20] reported the case of a 37-year-old woman at 27 weeks’ gestation, who after diagnosis of STEMI was treated with ‘off-label’ ticagrelor and ASA followed by PCI. The pregnancy was terminated at 39 weeks by cesarean section. The baby was born healthy and no teratogenic effect of ticagrelor was observed.
Conclusions
Myocardial infarction in pregnant women, despite being a rare condition, will directly endanger the life of both mother and fetus. Diagnosis should be carried out with the least possible risk of harm to the fetus. Despite the risks to the fetus posed by coronary angiography, it should be remembered that early revascularization of occluded coronary arteries can be life-saving. Of the drugs used in the treatment of myocardial infarction, unfractionated heparin or low-molecular-weight heparin seem reasonable because they do not cross the placenta. In addition, studies have shown that the use of ASA and clopidogrel does not affect the fetus or the course of pregnancy [19]. At the moment, the use of ticagrelor or prasugrel is risky, as there are not enough studies to determine whether its use is safe in pregnancy [20]. It is worth pointing out that acute myocardial infarction can occur at any stage of pregnancy and the postpartum period and the chances of saving a patient are greater when appropriate management is implemented quickly [7]. This article demonstrates the importance of prompt and accurate diagnosis and careful management of pregnant women with acute myocardial infarction and the appropriate choice of subsequent delivery method to ensure the best chance of survival for both mother and child.
Figures
References:
1.. Nowicki GJ, Ślusarska B, Piasecka H, The status of cardiovascular health in rural and urban areas of Janów Lubelski District in Eastern Poland: A population-based study: Int J Environ Res Public Health, 2018; 15(11); 2388
2.. Thygesen K, Alpert JS, Jaffe AS, Fourth universal definition of myocardial infarction (2018) [Fourth universal definition of myocardial infarction (2018)]: Kardiol Pol, 2018; 76(10); 1383-415
3.. Roth A, Elkayam U, Acute myocardial infarction associated with pregnancy: Ann Intern Med, 1996; 125(9); 751-62
4.. Badui E, Enciso R, Acute myocardial infarction during pregnancy and puerperium: A review: Angiology, 1996; 47(8); 739-56
5.. Kealey A, Coronary artery disease and myocardial infarction in pregnancy: A review of epidemiology, diagnosis, and medical and surgical management: Can J Cardiol, 2010; 26(6); 185-89
6.. Hankins GD, Wendel GD, Leveno KJ, Stoneham J, Myocardial infarction during pregnancy: A review: Obstet Gynecol, 1985; 65(1); 139-46
7.. James AH, Jamison MG, Biswas MS, Acute myocardial infarction in pregnancy: A United States population-based study: Circulation, 2006; 113(12); 1564-71
8.. Gordon M, Maternal physiology in pregnancy: Normal and problem pregnancies, 2002; 63-92, New York, NY, Churchill Livingstone
9.. Manson JE, Hsia J, Johnson KC, Estrogen plus progestin and the risk of coronary heart disease: N Engl J Med, 2003; 349(6); 523-34
10.. Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy: Kardiol Pol, 2019; 78(3); 245-326
11.. , Expert consensus document on management of cardiovascular diseases during pregnancy: Eur Heart J, 2003; 24(8); 761-81
12.. Kayıkçıoğlu M, Yavuzgil O, Eroğlu Z, Hereditary thrombophilia (factor V R2-mutation) as a contributing factor in premature myocardial infarction associated with pregnancy: Anadolu Kardiyol Derg, 2014; 14(7); 652-54
13.. Kayikcioglu M, Ozkan HS, Yagmur B, Premature myocardial infarction: A rising threat: Balkan Med J, 2022; 39(2); 83-95
14.. Rosendaal FR, Siscovick DS, Schwartz SM, Factor V Leiden (resistance to activated protein C) increases the risk of myocardial infarction in young women: Blood, 1997; 89(8); 2817-21
15.. Elkayam U, Jalnapurkar S, Barakkat MN, Pregnancy-associated acute myocardial infarction: A review of contemporary experience in 150 cases between 2006 and 2011: Circulation, 2014; 129(16); 1695-702
16.. Tweet MS, Hayes SN, Codsi E, Spontaneous coronary artery dissection associated with pregnancy: J Am Coll Cardiol, 2017; 70(4); 426-35
17.. Krittanawong C, Kumar A, Virk HUH, Recurrent spontaneous coronary artery dissection in the United States: Int J Cardiol, 2020; 301; 34-37
18.. Michaelis T, Gunaga S, McKechnie T, Shafiq Q, Acute myocardial infarction in a patient with twin pregnancy: A case report: Clin Pract Cases Emerg Med, 2021; 5(4); 507-10
19.. Sun P, Liang XQ, Hong T, Zhang H, Perioperative management of acute myocardial infarction in the 31st week of pregnancy: A case report and literature review: Front Surg, 2022; 9; 1023551
20.. Argentiero D, Savonitto S, D’Andrea P, Iacovelli F, Ticagrelor and tirofiban in pregnancy and delivery: Beyond labels: J Thromb Thrombolysis, 2020; 49(1); 145-48
Figures
In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943174
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943136
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943645
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942921
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250