08 December 2023: Articles 
Unusual Case of Splenic Metastasis in Adenosquamous Carcinoma of the Cervix Uteri: Diagnosis and Treatment Considerations
Unusual clinical course
Gilbert Georg Klamminger12ABCDEF*, Caroline Burgard3BCD, Florian RosarDOI: 10.12659/AJCR.941600
Am J Case Rep 2023; 24:e941600
Abstract
BACKGROUND: Due to several factors such as its specific cellular and biochemical microenvironment, the spleen is not a predestined organ of frequent metastatic colonization in the case of primary solid carcinoma. Hence, the mode of diagnosis and the preferred treatment of a lesion highly suspicious of splenic metastasis must be decided on a case-by-case basis, considering not only the biological tumor entity but also the stage of the primary disease.
CASE REPORT: In the present case, we demonstrate the clinical course of a 37-year-old female patient who initially presented to our clinic with irregular vaginal bleeding. A consecutive gynecological examination revealed a 3×3-cm large mass of the cervix uteri, and the subsequent histomorphological workup led to the diagnosis of an adenosquamous carcinoma of the cervix uteri. Therapeutically, the patient received multimodal treatment, namely radical hysterectomy with adjuvant radio-chemotherapy. After 1.5 years, the patient presented to our Emergency Department with intermittent left-sided abdominal pain. Subsequent abdominal imaging (computed tomography scan, magnetic resonance imaging, positron emission tomography) determined a metabolically active splenic lesion with a central necrosis – signs of malignancy in line with a splenic metastasis. Presentation and discussion of the case within our interdisciplinary tumor board led to the decision of splenectomy followed by chemotherapy, a procedure that could be considered as therapeutic treatment in such exceptional cases.
CONCLUSIONS: The collection and reporting of atypical clinical courses remains a key factor in precision medicine to enable the most evidence-based decision making in such cases.
Keywords: Spleen, Neoplasm Metastasis
Background
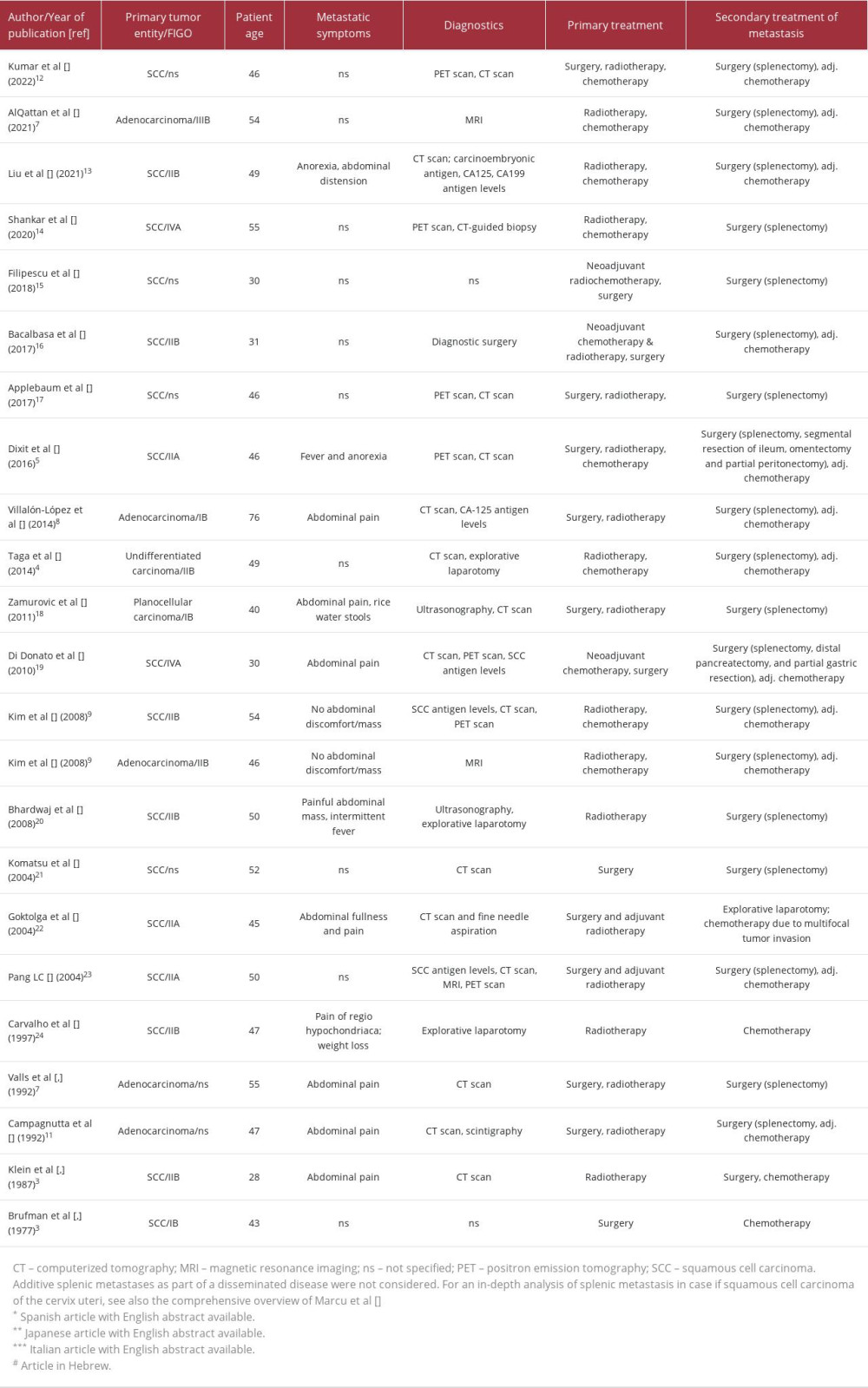
Clinical observations and reports of cervical carcinoma have a long historical tradition, ranging from the descriptions of Hippocrates and Aretaeus to Rigoni-Stern’s studies of its prevalence in Italian nuns [1,2]. The collection of exceptional cases and clinical data of this neoplasm and its rare clinical presentations is therefore not only part of a historical-scientific continuity, but rather aims for potential evidence-based therapeutic and diagnostic decision making also in individual situations. Even though single cases in the literature report on the rare phenomenon of splenic metastasis from squamous epithelial tumors of the cervix uteri [3–6], a literature review (Medline, Scopus, Embase) resulted in solely 5 published cases of splenic metastasis of cervical adenocarcinoma [7–11]; for a comprehensive overview of published cases known to date see Table 1 [12–26]. In the following case report, we present the clinical course of a 37-year-old female patient who was diagnosed with an adenosquamous carcinoma of the uterine cervix and a subsequent solitary splenic metastasis. To the best of our knowledge, this is the first description of a splenic metastasis of this distinct pathological entity. All details presented are in best alignment with the CARE writing guidelines [27,28].
Case Report
We report on a 37-year-old female patient who presented to our clinic with repetitive intermediate vaginal bleeding as well as irregular contact bleeding during intercourse. An initial clinical examination confirmed a 3×3-cm large mass of the cervix uteri, and subsequent collection of biopsies determined the presence of a malignant cervical neoplasm. Further staging examinations resulted in the clinical suspicion of a FIGO IIA tumor; therefore, the indication for surgical staging and sentinel lymphonodectomy with consecutive histopathological examination of frozen sections was given. Due to a negative lymph node status, laparotomy with radical hysterectomy (Piver II–III) and bilateral salpingectomy was performed [29,30]. An acute diffuse intraoperative hemorrhage and an emerging hemorrhagic shock caused by a cefuroxime/gelafundin allergy required transfusion of packed red blood cells and fresh frozen plasma as well as abdominal packing with 3 lab sponges to control the hemorrhage; a 2-stage procedure with re-laparotomy allowed for removal of the intraabdominal lab sponges and concurrent oophoropexy prior to adjuvant radio-chemotherapy with cisplatin 40 mg/m2. The gross examination of the surgical specimen showed a beige-reddish, firm mass of the cervix uteri with a diameter of 4.2×3×4.2 cm, extending toward the isthmus uteri and affecting the right parametrium. The histopathological assessment of the specimen revealed an infiltrating epithelial neoplasm of the cervix uteri, forming both atypical glands as well as a solid growth pattern, with densely packed eosinophilic cells showing keratinization (Figure 1). The moderately differentiated tumor cells displayed an increased nuclear-cytoplasmatic ratio, distinct nuclear atypia, and high rate of (partly atypical) mitosis. Further immunohistochemical analysis alternately stained the glandular (CK7, CEA, and PAX8 reactivity) and squamous (p40 reactivity) tumor aspects; only p16 showed cytoplasmatic reactivity in both morphological tumor components. In situ hybridization (INFORM HPV (human papillomavirus) III Family 16 Probe (B), Ventana Medical Systems, AZ, USA) of tumorous tissue fragments did not determine an oncogenic HPV type 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, or 66 association. No veins, lymphatic vessels, nor adjunct nerves were affected, and all included lymph nodes (sentinel and non-sentinel) as well as resection margins were tumor free. Based on the WHO classification of female genital tumors (5th edition), the neoplasm was classified as an adenosquamous carcinoma of the uterine cervix, HPV negative [31,32]. In accordance with the TNM (tumor, node, metastasis) Classification of Malignant Tumors (8th edition), the tumor stage was: pT2b, pN0 (0/5; sn-), L0, V0, Pn0, R0, G3. Post-therapeutically, no local or distant tumor progression was determined in the subsequent standard follow-up-screenings but due to intra-abdominal adhesions and a resulting mechanical ileus, the patient underwent re-surgery with adhesiolysis and small bowel resection with side-to-side anastomosis.
After a progression-free survival of 1.5 years, the patient presented to the Emergency Department with intermittent left-sided abdominal pain. Consecutive abdominal computed tomography (CT) scans revealed a lesion with a central hypodense (necrotic) area within the mediodorsal area of the spleen (Figure 2A). Primary splenic tumors such as benign hamartoma or splenic angiosarcoma could already be ruled out after CT because of the extensive, but somehow well-circumscribed, necrotic area. For more precise diagnosis, magnetic resonance imaging (MRI) and positron emission tomography (PET) scans were performed and showed a capsulated lesion with an intense glucose metabolism at tumor margins and a central necrosis, aspects highly suspicious of splenic metastasis (Figures 2B, 2C and 3). On calculated ADC maps, the solid rim showed somewhat lower signal intensities correlating to a diffusion restriction, whereas the necrotic center displayed high signal intensities consistent with a T2 shine through. Since the rim comprised only a very narrow zone, measurement of ADC values was dispensed with and a visual evaluation was conducted instead. Subsequent discussion of the case in our interdisciplinary tumor board led to the decision of surgical metastasis removal, not only enabling further diagnostics and histopathological determination of the tumor origin, but also representing a potential therapeutic option in such a case. Accordingly, splenectomy was performed (Figure 4), and thorough pathological examination of all macroscopically suspicious foci revealed the presence of a poorly differentiated carcinoma composed of solid nests of eosinophilic tumor cells with pleomorphic nuclei, distinct nucleoli, a high rate of atypical mitosis, and partly necrotic areas (Figure 5). The lesion was morphologically and immunohistochemically (strong nuclear immunoreactivity for p40 in all tumor cells) without glandular tumor components. Given the absence of glandular components, the history of a known adenosquamous carcinoma of the cervix uteri and no other site of squamous cell carcinoma in the extension workup, the diagnosis of a metastasis of an adenosquamous carcinoma in the form of a poorly differentiated squamous cell carcinoma well in line with the squamous component of the previously diagnosed epithelial tumor was made. Additional analysis of the metastatic tumor tissue showed a positive membranous PD-L1 expression in over 90% percent of the tumor cells (Tumor Proportion Score PD-L1: 90%, Cologne Score: 5). Re-evaluation within the tumor board review resulted in the recommendation of adjuvant chemotherapy (6 cycles of carboplatin AUC5, paclitaxel 175 mg/ m2, pembrolizumab 200 mg, and bevacizumab 15 mg/kg/KG intravenously every 3 weeks, followed by maintenance pembrolizumab 200 mg and bevacizumab 15 mg/kg/KG); at the time of publication the patient is under treatment and with no further evidence of local or distant metastasis for 10 months.
Discussion
Splenic metastases are rare per se [33] and a condition to which many different potential causes, such as mechanical aspects of the splenic anatomy (capsule), but also physiological aspects, namely a high concentration of resident phagocytes and a pro-apoptotic microenvironment, can contribute. So far, they appear either as a solitary metastasis or as part of a disseminated disease [34,35]. A hematogenous spread and subsequent extravasation/colonization of squamous cervical cancer cells in the splenic parenchyma have been rarely described in the literature [3,7], although the present case is, to the best of our knowledge, the first description of splenic metastasis of an uncommon cervical tumor entity, namely an adenosquamous carcinoma of the cervix uteri. Our patient’s age was below the mean age of 46 years for patients with adenosquamous carcinoma of the cervix uteri [31]. In comparison to recent reports of splenic metastasis of squamous carcinomas of the cervix uteri, with more than 75% of patients older than 40 years [3], our patient was again somewhat younger, at 38 years old, when her abdominal metastasis was detected via abdominal imaging. Since imaging techniques are in general sensitive to detect malignant splenic lesions, adding 18F-fluorodeoxyglucose PET/CT may even improve the detection rate, as it proved diagnostically helpful also in our case; biopsy for diagnostic purposes should be reserved for lesions with unclear malignancy to rule out possible differential diagnoses, such as infectious causes or granulomatous diseases [12].
It is notable that solely the dedifferentiated squamous component of our reported adenosquamous neoplasm formed metastatic lesions, which is in line with single cases in the literature that described a change or a worse histological appearance of splenic metastasis tumors than that of the primary side tumors [5,16,19,20]. Nevertheless, initial diagnosis of adenosquamous carcinoma of the cervix uteri within the primary site required both malignant squamous and glandular components in routine hematoxylin and eosin sections as essential diagnostic criteria. The use of specific immunochemical methods could be helpful but is not mandatory for a definitive diagnosis. The preferably unimodal, therapeutic options of the primary tumor depend on the initial tumor stage and associated risk factors and provide a broad spectrum of possible treatment modalities (surgery/radio-chemotherapy) [29]; despite the existing potential therapeutic options for solitary splenic metastases [15], there is to date no evidence-based first-line therapy. In a recent literature review, Marcu et al highlighted the biological impact of splenectomy (diagnostic tissue assessment, prevention of local complications, such as rupture and thrombosis) and adjuvant chemotherapy (distant metastasis [5]) in solitary splenic squamous metastases, although the effect of surgery has been questioned in cases of disseminated disease [3,4]. In our review of cases of splenic metastasis of squamous cell carcinoma and adenocarcinoma of the cervix uteri, determination of explicit prognosis (5 to 30 months of median survival [7]) did not prove to be feasible, nor could correlation of clinical parameters and patient outcomes be made [3]. Since known survival data is based on tumor entities different from that in our presented case, explicit deduction remains questionable, especially since a prognostic evaluation of the primary tumor itself is largely unclear in case of adenosquamous carcinoma of the cervix uteri [31].
Conclusions
We presented a splenic metastasis of an adenosquamous carcinoma of the cervix uteri, indeed a rare course of one of the most frequent malignancies in women. Especially in such rare clinical cases, further data collection and reporting remain key to gain experience, enabling evidence-based decision making in those rare cases as well.
Figures
References:
1.. Scotto J, Bailar JC, Rigoni-Stern and medical statistics. A nineteenth-century approach to cancer research: J Hist Med Allied Sci, 1969; XXIV(1); 65-75
2.. Gasparini R, Panatto D, Cervical cancer: From Hippocrates through Rigoni-Stern to zur Hausen: Vaccine, 2009; 27(Suppl. 1); A4-5
3.. Marcu ML, Neacşu A, Stoica C, Clinical and pathological features of splenic metastasis from cervical squamous cell carcinoma: Rom J Morphol Embryol, 2017; 58(4); 1157-64
4.. Taga S, Sawada M, Nagai A, Splenic metastasis of squamous cell carcinoma of the uterine cervix: A case report and review of the literature: Case Rep Obstet Gynecol, 2014; 2014; 798948
5.. Dixit J, Mohammed N, Shetty P, Splenic metastasis from cancer of uterine cervix – a rare case: Indian J Surg Oncol, 2016; 7(4); 479-83
6.. Gupta T, Nair N, Fuke P, Splenic metastases from cervical carcinoma: A case report: Int J Gynecol Cancer, 2006; 16(2); 911-14
7.. AlQattan AS, Alqutub AA, Masoudi JH, Splenic oligometastasis from cervical adenocarcinoma three years after disease free survival: A case report and a review of literature: Ann Med Surg (Lond), 2021; 72; 103144
8.. Villalón-López JS, Souto-del Bosque R, Montañez-Lugo JI, Chávez-González B, [Isolated splenic metastases from cervical cancer: A rare entity.]: Cir Cir, 2014; 82(5); 556-62 [in Spanish]
9.. Kim JH, Choi YD, Lee JH, Solitary splenic metastases from uterine cervical cancer: Case reports and review of the literature: Korean J Pathol, 2008; 42(5); 317-22
10.. Valls C, Serra J, Isolated splenic metastasis from uterine cervical adenocarcinoma: Am J Roentgenol, 1992; 158(4); 919-20
11.. Campagnutta E, Zarrelli A, Stefanutti V, [Isolated splenic metastasis in a case of adenocarcinoma of the uterine cervix. A clinical case.]: Minerva Ginecol, 1992; 44(12); 667-70 [in Italian]
12.. Kumar A, Upadhyay A, Pandey V, A rare case of splenic metastasis from squamous cell carcinoma of the cervix detected on 18F-fluorodeoxyglucose PET/CT: Cureus, 2022; 14(11); e31974
13.. Liu Q, Wang M, Gayam V, Li XL, The clinical course and management of cervical cancer with splenic metastasis: Case report and review of the literature: Clin Case Rep, 2020; 9(2); 689-93
14.. Shankar ST, Panse M, Goel A, Solitary splenic metastasis in a case of treated cervical cancer: A case report: Int J Reprod Contracept Obstet Gynecol, 2020; 9(5); 2211
15.. Filipescu A, Balescu I, Bacalbasa N, Upper abdominal resection for isolated metastatic lesions in recurrent cervical cancer: Anticancer Res, 2018; 38(3); 1659-63
16.. Bacalbasa N, Balescu I, Marcu M, Solitary splenic metastasis after surgically-treated cervical cancer – a case report and literature review: Anticancer Res, 2017; 37(5); 2615-18
17.. Applebaum M, Schulz B, Isolated splenic metastasis in a patient with squamous cell carcinoma of the cervix: Appl Radiol, 2017; 6(46); 24-25
18.. Zamurovic M, Pesic-Stevanovic I, Perisic Z, Rare metastases of carcinoma of uterine cervix: Eur J Gynaecol Oncol, 2011; 32(5); 594-96
19.. Di Donato V, Palaia I, Perniola G, Splenic metastasis from cervical cancer: Case report and review of the literature: J Obstet Gynaecol Res, 2010; 36(4); 887-90
20.. Bhardwaj S, Mahajan D, Gupta YV, Metastatic squamous cell carcinoma of the cervix presenting as a splenic cyst: JK Sci, 2008; 10(3); 146
21.. Komatsu D, Koike S, Kobayashi N, [Case of solitary splenic metastasis from uterine cervical cancer.]: Jpn J Gastroenterol Surg, 2004(37); 193-97 [in Japanese]
22.. Goktolga U, Dede M, Deveci G, Solitary splenic metastasis of squamous cell carcinoma of the uterine cervix: A case report and review of the literature: Eur J Gynaecol Oncol, 2004; 25(6); 742-44
23.. Pang LC, Solitary recurrent metastasis of squamous cell carcinoma of the uterine cervix in the spleen: Case report: South Med J, 2004; 97(3); 301-4
24.. Carvalho L, Azevedo I, Salgado L, Squamous cell carcinoma of the cervix metastatic to the spleen – case report: Gynecol Oncol, 1997; 67(1); 107-10
25.. Klein B, Stein M, Kuten A, Splenomegaly and solitary spleen metastasis in solid tumors: Cancer, 1987; 60(1); 100-2
26.. Brufman G, Biran S, Goldschmidt Z, Freund U, [Solitary metastatic involvement of the spleen in squamous cell carcinoma of the cervix.]: Harefuah, 1977; 92(8); 349-50 [in Hebrew]
27.. Gagnier JJ, Kienle G, Altman DG, The CARE guidelines: Consensus-based clinical case reporting guideline development: Glob Adv Health Med, 2013; 2(5); 38-43
28.. Riley DS, Barber MS, Kienle GS, CARE guidelines for case reports: Explanation and elaboration document: J Clin Epidemiol, 2017; 89; 218-35
29.. [Accessed September 1, 2023]https://www.leitlinienprogramm-onkologie.de/leitlinien/zervixkarzinom/
30.. Ramirez PT, Frumovitz M, Pareja R, Minimally invasive versus abdominal radical hysterectomy for cervical cancer: New Engl J Med, 2018; 379(20); 1895-904
31.. Lokuhetty D: Female genital tumours WHO Classification of Tumours, 2020; 631, Lyon, Internal Agency for Research on Cancer (IARC)
32.. Brierley JD, Gospodarowicz MK, Wittekind C: TNM Classification of Malignant Tumours, 2016, Geneva, Union for International Cancer Control
33.. Lam KY, Tang V, Metastatic tumors to the spleen: A 25-year clinicopathologic study: Arch Pathol Lab Med, 2000; 124(4); 526-30
34.. Berge T, Splenic metastases. Frequencies and patterns: Acta Pathol Microbiol Scand A, 1974; 82(4); 499-506
35.. Compérat E, Bardier-Dupas A, Camparo P, Splenic metastases: Clinicopathologic presentation, differential diagnosis, and pathogenesis: Arch Pathol Lab Med, 2007; 131(6); 965-69
Figures
In Press
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250