24 February 2024: Articles 
Herpes Simplex Keratitis as a Complication of Pterygium Surgery
Mistake in diagnosis, Unusual or unexpected effect of treatment, Diagnostic / therapeutic accidents, Rare disease, Educational Purpose (only if useful for a systematic review or synthesis)
Xinhan Cui1BCDEFG, Jini Qiu1BC, Feifei Huang1BE, Chaoran Zhang1EG, Tingting Shao1AEF, Yan Wang1AEF*DOI: 10.12659/AJCR.942401
Am J Case Rep 2024; 25:e942401
Abstract
BACKGROUND: Infectious keratitis after pterygium surgery is a rare but potentially devastating complication. The present study presents 5 cases of herpes simplex keratitis (HSK) after pterygium surgery.
CASE REPORT: This study was conducted in our clinic in a 5-year period from February 2017 to September 2021. The 5 patients were men, aged between 42 and 73 years, with no prior history of herpes simplex virus (HSV) infections. Symptoms appeared near 1 month (median 30 days, range 10 to 70 days) after primary pterygium surgery. Diagnosis was based on clinical symptoms and laboratory test results, such as tear HSV-sIgA, corneal tissue polymerase chain reaction, and next-generation sequencing of metagenomics. The epithelial (1/5) and stromal (4/5) subtypes of HSK were identified. The patients received topical ganciclovir gel, immunosuppressive eyedrops, and oral acyclovir tablets, along with additional surgical interventions if necessary. Three were healed with conservative therapy, 1 eye required amniotic membrane transplantation due to corneal melt, and 1 was perforated and followed by corneal grafting. Finally, a literature review of previous publications on HSK after ocular surgeries was conducted.
CONCLUSIONS: HSK is a rare but serious complication that can arise after uneventful pterygium surgery. It is worthy of attention that both epithelial and stromal forms can occur. Timely diagnosis and treatment are crucial to prevent unfavorable outcomes. Consequently, routine corneal fluorescein staining, tear sIgA examination, and corneal scraping for polymerase chain reaction or next-generation sequencing of metagenomics should be performed in any suspected cases.
Keywords: DNA polymerase, Simplexvirus, Metagenomics, Pterygium
Background
Pterygium surgery is a mature technique that generally has a low rate of infectious complications. In the literature, few cases of microbial keratitis have been reported after pterygium removal [1–3]. The prevalence is difficult to estimate statistically owing to the limited number of cases. Soleimani et al reported the incidence of keratitis as 2 cases in 1000 pterygium operations [2]. Among the documented cases, bacteria were the most commonly isolated organisms [2,3]. However, there has been comparatively limited attention paid to viral infections after pterygium surgery.
Herpes simplex keratitis (HSK) is a sight-threatening condition caused by herpes simplex virus (HSV) infection, including HSV-1 and HSV-2, which is widely spread worldwide [4]. Several studies have reported HSK affecting eyes after ocular surgical procedures, such as cataract surgery [5], penetrating keratoplasty [6], and laser-assisted in situ keratomileusis [7]. It is interesting that HSV is connected with pterygium. HSV-1 was detected in surgically excised symptomatic pterygia by several studies, and was indicated to be associated with postoperative recurrence [8–10]. This intriguingly raises the possibility of HSK occurrence following pterygium surgery.
Clinical diagnosis in acute keratitis is usually not difficult, but laboratory diagnosis is frequently recommended, since HSK ulcers do not often present a classic dendritic or geographic appearance, particularly if it is the first episode of occurrence without a previously confirmed diagnosis [4]. Detecting HSV-specific tear secretory IgA (sIgA) has been shown to be highly efficient, with the benefits of safety and convenience [11,12]. This retrospective study describes the presentation of HSK after pterygium surgery in 5 patients without a history of herpetic disease. Finally, we review the literature on HSK cases after ocular surgery, in an attempt to collect the distinguishing characteristics of this form of keratitis.
Case Report
This was a retrospective review of case records from 5 patients with HSK after removal of pterygium who were seen at the Eye and ENT Hospital of Fudan University between February 2017 and September 2021. Each patient was subjected to a thorough history and examination before starting therapy, with slit lamp photography used to determine the area of the corneal ulcer. Corneal scrapings were performed in all cases under topical anesthesia and then inoculated directly into primary culture media for bacteria and fungi. Tear samples from the lower fornixes of both eyes were collected and assayed by enzyme-linked immunosorbent assay (ELISA) to detect HSV sIgA [12]. For cases with negative tear HSV-sIgA, small cornea tissue around the ulcer was scraped and processed for DNA extraction, and then a corneal HSV DNA polymerase chain reaction (PCR), or next-generation metagenomics sequencing (mNGS) test was chosen to detect the HSV pathogen load [13].
Once they were suspected of having HSK, all patients received topical ganciclovir gel and oral acyclovir tablets, with immunosuppressive eyedrops for cases of stromal HSK. Corticosteroids and additional surgery, such as amniotic membrane transplantation or therapeutic corneal grafting, would be performed if necessary. The patients were closely visited until the symptoms disappeared. The main outcome measure for each patient was complete epithelialization of the corneal ulcer in epithelial HSK and the absence of corneal infiltrate in stromal HSK [14]. Finally, a review of the literature on HSK after ocular surgery was performed.
Details of the HSK cases after pterygium surgery are listed in Tables 1 and 2. All 5 patients were men, aged 42 to 73 years (median 64 years). Of the 5 cases, only 1 patient (case 3) had his pterygium resected with a conjunctival graft in our clinic and was prescribed a bandage contact lens after surgery. The other 4 patients received previous pterygium surgery at other centers, and were referred to our center due to uncontrolled keratitis, receiving treatments for periods of 20 to 80 days.
All patients presented to our eye clinic with pain, redness, photophobia, and tearing in the affected eye. Symptoms were reported around 1 month (median 30 days, range 10 to 70 days) after primary pterygium surgery. A nasal peripheral epithelial defect was observed in all eyes, with (stromal HSK, 4/5) or without (epithelial HSK, 1/5) a corneal stromal infiltrate (Figure 1). The case of epithelial HSK (case 3) had the shortest latency period after pterygium surgery (10 days). Measurements of corneal infiltrate area were taken for the 4 eyes with stromal infiltration; the smallest measurement was about 9 mm2, and the largest around 24 mm2. In addition, 2 of our 5 patients (cases 2 and 5) showed a recurrence of pterygium.
Corneal scrapings obtained from all patients revealed negative growth of any bacteria or fungal cultures. A single eye (case 3) was noted with scattered dendritic lesions with terminal bulbs and intraepithelial infiltrates and was quickly diagnosed with fluorescence staining. After cessation of steroid drops and use of 0.15% ganciclovir gel 4 times a day and oral acyclovir tablets 400 mg 5 times a day, there was a significant improvement in symptoms and corneal findings. Ten days later, the dendritic lesion resolved completely, and the drugs were tapered and ultimately discontinued after another week.
Two of the 4 patients (cases 2 and 5) with dense stromal infiltrate were diagnosed with elevated tear HSV-sIgA. Both were treated with 0.1% tacrolimus (FK-506) eyedrops 4 times daily, 0.15% ganciclovir gel 4 times daily, and oral acyclovir tablets 400 mg 5 times daily. The case of patient 2, who received amniotic membrane transplantation treatment, is described in detail. After a 2-week trial of conservative treatment, the patient continued to experience epithelial defects and stromal melt, resulting in a 3-mm hypopyon. In response to this challenge, amniotic membrane transplantation was administered. Additional oral prednisone and antiviral treatments were prescribed, leading to a successful resolution of keratitis within 2 months. The other patient (case 5) responded well to the drugs, and 0.1% fluorometholone eyedrops were prescribed once the epithelium healed, 3 weeks after treatment. No more surgical intervention was necessary.
One of the 2 eyes with negative tear HSV-sIgA was perforated at the first visit to our clinic and soon acquired a therapeutic corneal patch graft (case 1). Viral PCR from the cornea achieved in surgery revealed a positive result for HSV-1. The last patient (case 4) was diagnosed by mNGS. The infections in both eyes gradually decreased with the application of FK-506, ganciclovir gel, and acyclovir tablets. Tobramycin and dexamethasone eyedrops were prescribed 4 times a day after the epithelial defect healed. After 3 months of treatment, the infections resolved completely.
Discussion
HSK is a known complication after some ocular surgeries (details in Table 3). However, only a solitary case report has previously mentioned HSK after pterygium surgery [15]. Here, we provided clinical descriptions of 5 new-onset cases of HSK after pterygium surgery. We reported the patients’ clinical characteristics, including the features of corneal lesions, delay in diagnosis, treatments, and different outcomes.
Previous studies indicate that epithelial keratitis is the most common HSV eye involvement, seen in 79% of patients in the Herpetic Eye Disease Study [16]. This is in line with our findings summarized in Table 3, in which 64 of the 76 HSV-infected eyes after ocular surgery presented as epithelial HSK. However, our 5-case series had only 1 epithelial HSK after pterygium surgery. This may have been due to the delayed diagnosis and treatment, which caused the initial epithelial HSK to develop to stromal infiltration. On the other hand, research suggests that an abnormal limbal basal epithelial stem cell can dissolve the Bowman layer beneath the pterygium site in the cornea. This process can facilitate the spread of HSV from the epithelium to the stroma, potentially eliciting an inflammatory response [17].
Previous studies have found no relationship between the location of HSK lesions and the cataract incision [5,18]. Also, it is difficult to determine whether the lesions are adjacent to the former incision, such as penetrating keratoplasty, laser in situ keratomileusis, photorefractive keratectomy, and lamella keratoplasty, due to the round- or ring-shaped nature of the surgery incision. However, in our study, all infiltrates were located in the area of the cornea that had previously received pterygium excision surgery, which agreed with the report of Mahajan and Prasher [15]. The same location provides strong evidence for a correlation between HSK and pterygium surgery. It has been reported that surgical trauma to the subepithelial trigeminal nerve plexus can reactivate the latent HSV-1 virus, leading to viral shedding and secondary infections [5,6,19,20]. And considering previous studies that revealed the presence of HSV in pterygia, these are all the possible etiologies of HSK after pterygium surgery. On the other hand, the administration of topical corticosteroids postoperatively could also play a pivotal role in this process.
In terms of prognosis, epithelial HSK can be managed successfully without surgical intervention, but necrotizing HSV stromal keratitis is especially difficult to manage given its ability to quickly progress to corneal perforation [14]. As this is a rare complication after pterygium surgery, clinical signs can easily be neglected, leading to delayed diagnosis. In our report, only 1 of the 5 cases was promptly diagnosed with its typical dendritic shape under corneal fluorescent staining. Therefore, an early and accurate diagnosis is very important, for which the tear HSV-sIgA examination can be very useful in diagnosing stromal HSK and predicting recurrence, even for atypical or unsuspected cases [11,12]. Two of our cases were quickly diagnosed with elevated tear HSV-sIgA, and successfully controlled with antiviral treatment. It should be noted that for highly suspected cases with negative tear HSV-sIgA results, traditional HSV PCR or even mNGS can be applied. Laboratory proof of HSV plays an irreplaceable role in the diagnosis and treatment of HSK.
Conclusions
Based on the results of our study, we suggest that if a patient develops epithelial or stromal keratitis in the early postoperative period following pterygium excision, viral infection with herpes simplex should be considered. Regardless of the patient’s history of keratitis, routine corneal fluorescent staining, tear HSV-sIgA examination, and corneal scraping mNGS for HSV testing is highly recommended in suspicious cases. An accurate and early diagnosis is essential for a good prognosis in patients with HSK.
References:
1.. Shenoy R, Bialasiewicz AA, Al-Barwani B, Late corneal thinning and keratitis following mitomycin-C use in pterygium surgery: Sultan Qaboos Univ Med J, 2011; 11(2); 286-87
2.. Soleimani M, Tabatabaei SA, Mehrpour M, Infectious keratitis after pterygium surgery: Eye (Lond), 2020; 34(5); 986-88
3.. Liu X, Ye X, Bi Y, Staphylococcus-associated marginal keratitis secondary to pterygium surgery: A case report: BMC Ophthalmol, 2021; 21(1); 157
4.. Sibley D, Larkin D, Update on Herpes simplex keratitis management: Eye (London, England), 2020; 34(12); 2219-26
5.. Cho YK, Kwon JW, Konda S, Ambati BK, Epithelial keratitis after cataract surgery: Cornea, 2018; 37(6); 755-59
6.. Rezende RA, Uchoa UB, Raber IM, Rapuano CJ, New onset of herpes simplex virus epithelial keratitis after penetrating keratoplasty: Am J Ophthalmol, 2004; 137(3); 415-19
7.. Jain V, Pineda R, Reactivated herpetic keratitis following laser in situ keratomileusis: J Cataract Refract Surg, 2009; 35(5); 946-48
8.. Spandidos D, Xinarianos G, Ergazaki M, Giannoudis A, Tsamparlakis J, The presence of herpesviruses in pterygium: Int J Oncol, 1994; 5(4); 749-52
9.. Rykov SO, Usenko KO, Mogilevskyy SY, Zyablytsev SV, The role of herpesvirus and human papillomavirus in the onset of pterygium: Archive of Ukrainian Ophthalmology, 2018; 6(3); 41-45
10.. Detorakis ET, Sourvinos G, Spandidos DA, Detection of herpes simplex virus and human papilloma virus in ophthalmic pterygium: Cornea, 2001; 20(2); 164-67
11.. Qiu J, Huang F, Wang Z, The evaluation of diagnostic efficiency for stromal herpes simplex keratitis by the combination of tear HSV-sIgA and HSV-DNA: Graefes Arch Clin Exp Ophthalmol, 2017; 255(7); 1409-15
12.. Huang F, Wang Z, Zhang C, Tear HSV-specific secretory IgA as a potential indicator for recurrent stromal herpes simplex keratitis: A preliminary study: Cornea, 2013; 32(7); 987-91
13.. Ai JW, Zhang HC, Cui P, Dynamic and direct pathogen load surveil-lance to monitor disease progression and therapeutic efficacy in central nervous system infection using a novel semi-quantitive sequencing platform: J Infect, 2018; 76(3); 307-10
14.. Knickelbein JE, Hendricks RL, Charukamnoetkanok P, Management of herpes simplex virus stromal keratitis: An evidence-based review: Surv Ophthalmol, 2009; 54(2); 226-34
15.. Mahajan G, Prasher P, An unusual case of herpes simplex keratitis presenting as persistent epithelial defect after pterygium surgery: Indian Journal of Ophthalmology – Case Reports, 2023; 3(2); 281-82
16.. , Predictors of recurrent herpes simplex virus keratitis. Herpetic Eye Disease Study Group: Cornea, 2001; 20(2); 123-28
17.. Reid TW, Dushku N, What a study of pterygia teaches us about the cornea? Molecular mechanisms of formation: Eye Contact Lens, 2010; 36(5); 290-95
18.. Barequet I, Wasserzug Y, Herpes simplex keratitis after cataract surgery: Cornea, 2007; 26(5); 615-17
19.. Jhanji V, Ferdinands M, Sheorey H, Unusual clinical presentations of new-onset herpetic eye disease after ocular surgery: Acta Ophthalmol, 2012; 90(6); 514-18
20.. Beyer CF, Hill JM, Byrd TJ, Kaufman HE, Herpes simplex dendritic keratitis after keratoplasty: Am J Ophthalmol, 1991; 112(3); 355-56
Tables
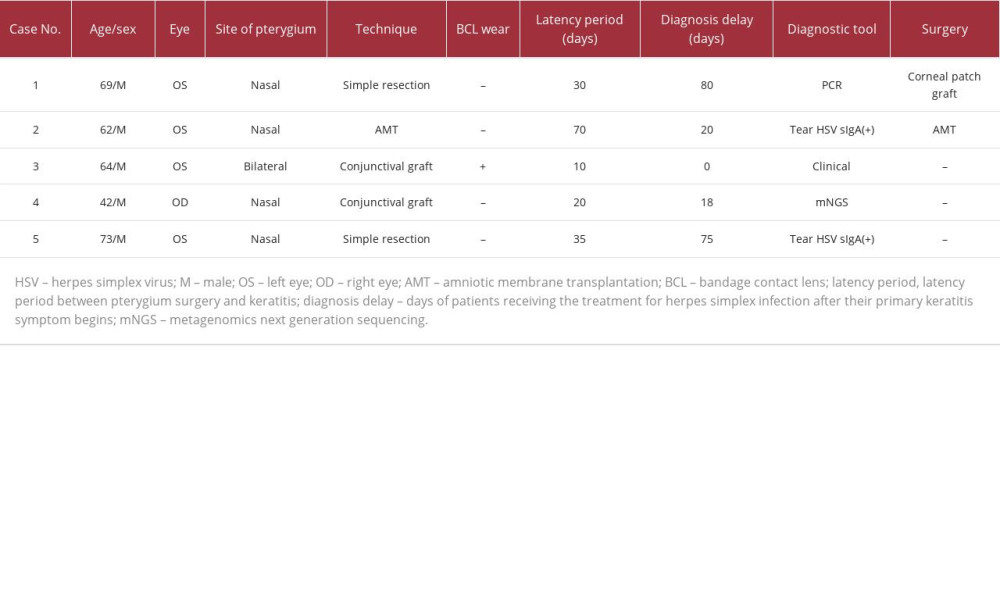 Table 1.. Details of the patients with herpes simplex keratitis after pterygium surgery.
Table 1.. Details of the patients with herpes simplex keratitis after pterygium surgery.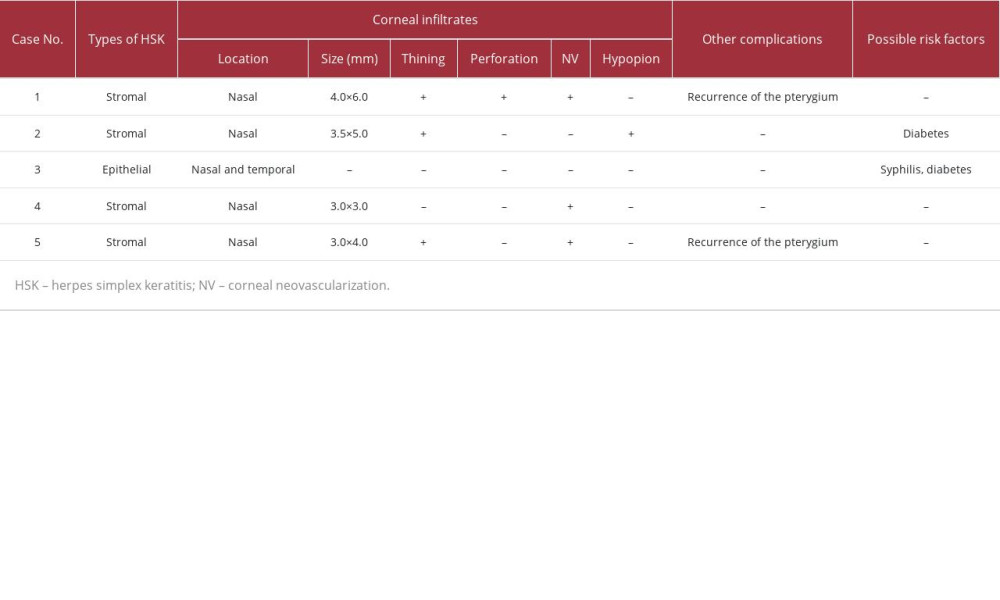 Table 2.. Details of herpes simplex keratitis and the prognosis in patients after pterygium surgery.
Table 2.. Details of herpes simplex keratitis and the prognosis in patients after pterygium surgery.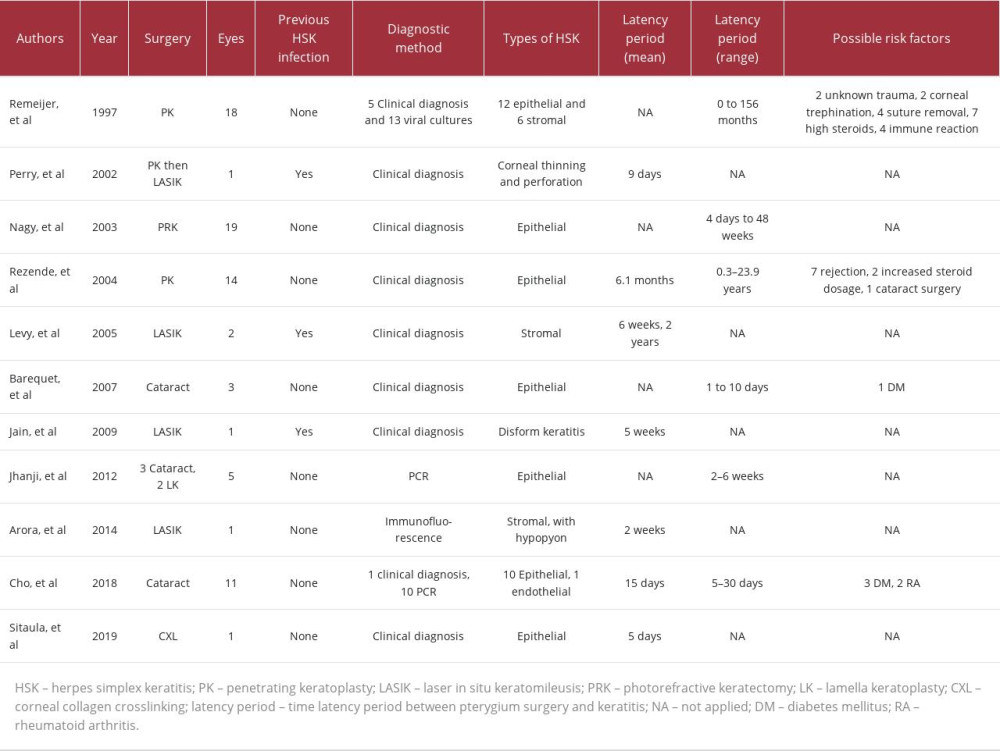 Table 3.. Clinical data of patients with herpes simplex keratitis after ocular surgery.
Table 3.. Clinical data of patients with herpes simplex keratitis after ocular surgery.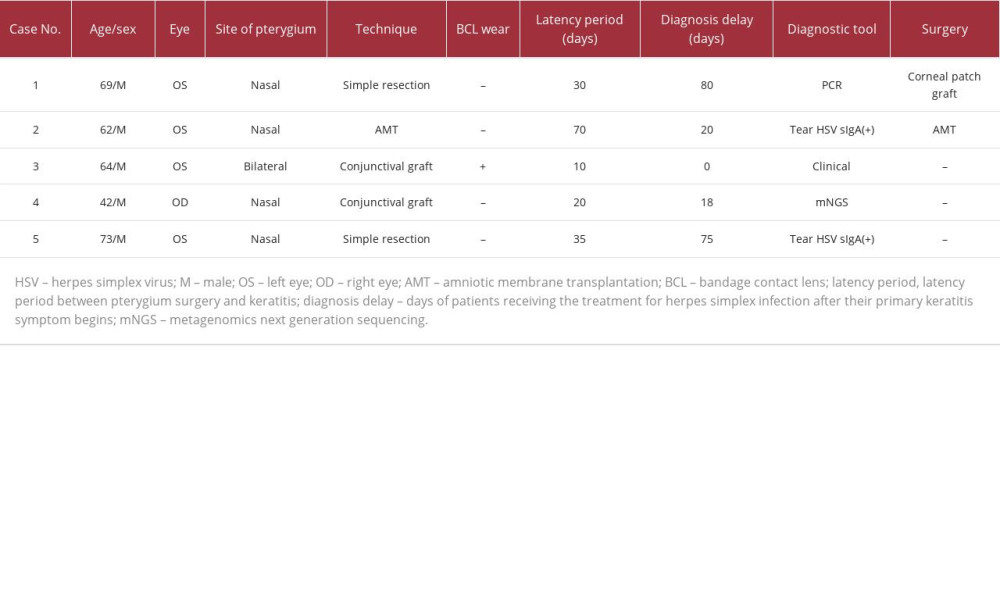 Table 1.. Details of the patients with herpes simplex keratitis after pterygium surgery.
Table 1.. Details of the patients with herpes simplex keratitis after pterygium surgery.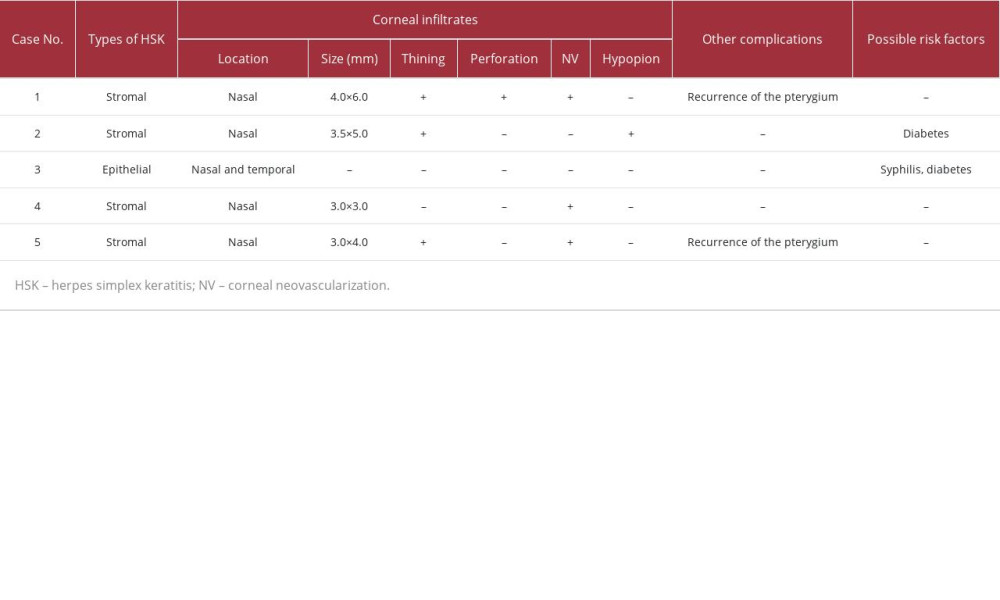 Table 2.. Details of herpes simplex keratitis and the prognosis in patients after pterygium surgery.
Table 2.. Details of herpes simplex keratitis and the prognosis in patients after pterygium surgery.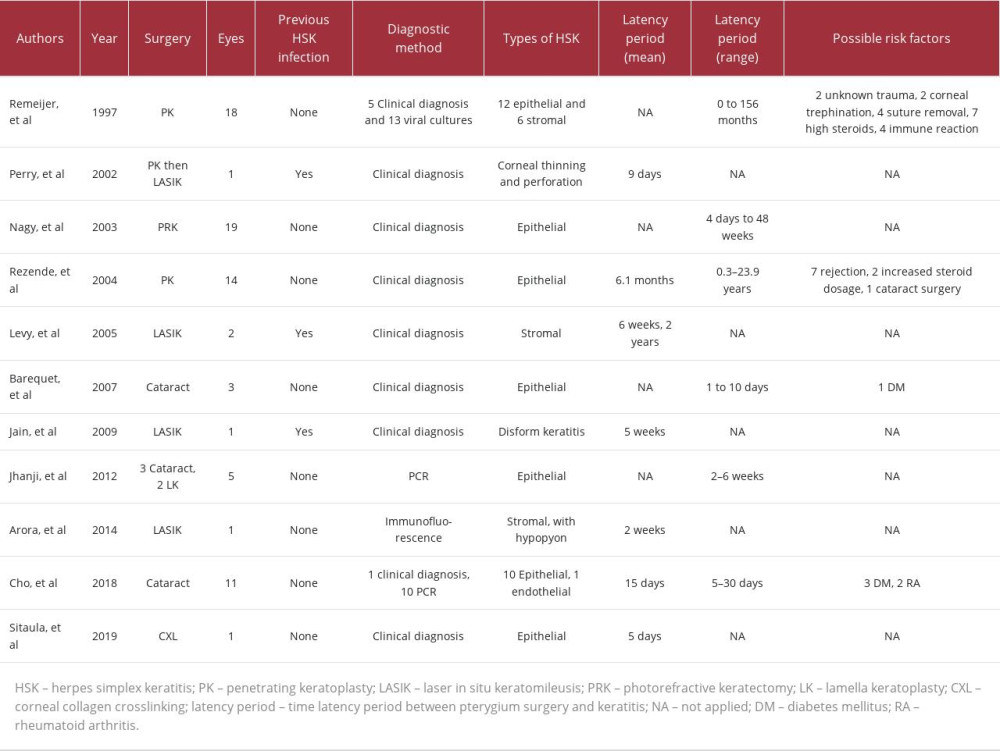 Table 3.. Clinical data of patients with herpes simplex keratitis after ocular surgery.
Table 3.. Clinical data of patients with herpes simplex keratitis after ocular surgery. In Press
24 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943560
26 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943893
27 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942126
27 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943098
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








