27 March 2024: Articles 
Case Report of Overlapping Pyloric Obstruction Due to Dichlorvos Poisoning and Cholelithiasis with Choledocholithiasis
Unusual clinical course, Unusual or unexpected effect of treatment
Jie PengDOI: 10.12659/AJCR.943101
Am J Case Rep 2024; 25:e943101
Abstract
BACKGROUND: Pyloric obstruction after dichlorvos poisoning causes repeated vomiting and inability to eat. Choledocholithiasis and cholelithiasis are the common digestive diseases, with high morbidity and relapse in elderly patients. However, the complex situation of these diseases’ coexistence is a clinically intractable problem, and literature on selecting optimal surgical planning is scarce.
CASE REPORT: A thin 79-year-old woman took dichlorvos due to family conflicts. She improved after being urgently sent to local hospital for gastric lavage and detoxification. Over the next 3 months, she presented with intermittent nausea, vomiting, epigastric pain, and mental apathy, and was readmitted. Gastroscopy showed extensive scarring in the antrum, pyloric obstruction, and gastric retention. Magnetic resonance cholangiopancreatography revealed gallstones and choledocholithiasis. Also, she presented with gastric retention, hypertension, moderate anemia, hypoproteinemia, and electrolyte disturbances. After hospitalization, conservative treatment was performed, without improving vomiting, followed by surgical treatment. Gastrojejunostomy, Braun anastomosis, and nasojejunal feeding tube placement were performed for pyloric stenosis; cholecystectomy for cholelithiasis; and choledochotomy, intraoperative choledochoscopy examination, basket stone extraction, and primary suture of common bile duct without indwelling T tube for choledocholithiasis. Patient recovered and was discharged 9 days after surgery. She was recovered well, without vomiting, at 2-month follow-up.
CONCLUSIONS: Gastrojejunostomy plus Braun anastomosis is effective treatment of elderly patients with pyloric obstruction formed after pesticide-induced corrosion. Careful selection of choledocholithotomy with primary suture without indwelling T tube reduced postoperative pain and accelerated recovery. This complex case of pyloric obstruction with gallbladder and bile duct stones provides useful considerations for clinical treatment.
Keywords: Cholecystolithiasis, choledocholithiasis, Pyloric Stenosis, dichlorvos, Gastric Bypass
Introduction
The majority of suicides in China are due to pesticide poisoning [1]. Dichlorvos is an organophosphorus insecticide frequently used in agricultural production [2]. It is strongly corrosive and burns the digestive tract after oral ingestion and can present with symptoms such as ulcers, perforations, and bleeding. More importantly, pyloric stenosis and even pyloric obstruction can occur due to scar formation [3]. Choledocholithiasis and cholecystolithiasis often cause bile duct obstruction and inflammatory lesions. Approximately 10% to 20% of individuals with gallstones also have concurrent choledocholithiasis [4]. There is a high risk of morbidity and potential mortality from cholangitis or pancreatitis induced by obstructive choledocholithiasis; thus, current guidelines recommend biliary stone extraction for all identified choledocholithiasis, regardless of symptoms [5]. Pyloric obstruction and choledocholithiasis cause symptoms such as abdominal pain, nausea, and repeated vomiting in patients, bringing physical damage and mental stress. As yet, there are no relevant reports on multiple combined diseases of pyloric obstruction with biliary system calculus in elderly patients, and surgeons have no unified treatment plan. Herein, we describe the case of an elderly patient with dichlorvos-induced pyloric obstruction due to attempted suicide, with concomitant choledocholithiasis and gallstones, who underwent combined surgical procedures, including gastrojejunostomy (gastric bypass), Braun anastomosis, nasoenteric tube insertion, cholecystectomy, choledochotomy, intraoperative choledochoscopy examination, basket stone extraction, and one-stage suture of the common bile duct.
Case Report
A 79-year-old female patient with a body mass index of 17.3 kg/m2 was admitted due to “vomiting for 20 days” on June 14, 2023. The patient could not eat or drink water. After eating, even drinking, the patient developed nausea and vomiting, vomiting non-jet-like, and the vomitus was gastric contents containing persistent food from the previous day, with a spoiled fermented odor. During this period, the patient was treated in a community hospital for acid suppression and protection of gastric mucosa, including omeprazole and bismuth potassium citrate, and the symptoms were not significantly improved.
The patient’s past medical history was as follows. The patient drank almost 50 mL dichlorvos impulsively due to family conflict with her daughter-in-law and agitation on March 27, 2023. She was urgently sent to a local hospital for gastric lavage. The use of a proton pump inhibitor (omeprazole) to inhibit gastric acid secretion, cholinesterase reactivator (pralidoxime chloride), anticholinergic drug (atropine), and the maintenance of water-electrolyte balance (supplementing fluid with potassium and sodium) improved the patient’s symptoms. According to the family, this was the patient’s first and only suicide attempt to date. From March to June, the patient had experienced loss of appetite, nausea, vomiting, and epigastric discomfort but did not seek medical help. It is worth noting that there was intermittent epigastric discomfort after meals as early as about 1 year earlier, which could be relieved after rest and therefore did not attract enough attention. In addition, the patient had a history of hypertension for many years, orally took nifedipine, and the blood pressure control was fair. The patient denied a history of food and drug allergy, smoking and drinking, surgery and trauma, diabetes, and mental illness.
Physical examination showed a body temperature of 36.5°C, pulse of 82 beats/min, respiration of 18 breaths/min, blood pressure of 148/80 mmHg, thin body, malnutrition, apathy, confusion, pale skin and mucosa, no icteric sclera, equal and round pupils bilaterally, normal respiratory movement, clear breath sounds in both lungs, no murmur on auscultation of each valve of the heart, and a flat abdomen that was soft with no tenderness or rebound tenderness and no palpable mass. The liver and spleen were not palpable under the ribs. The Murphy’s sign was negative, there was no percussion pain in the renal area, no shifting dullness, and bowel sounds were 4 times/min. There was no edema in both lower limbs.
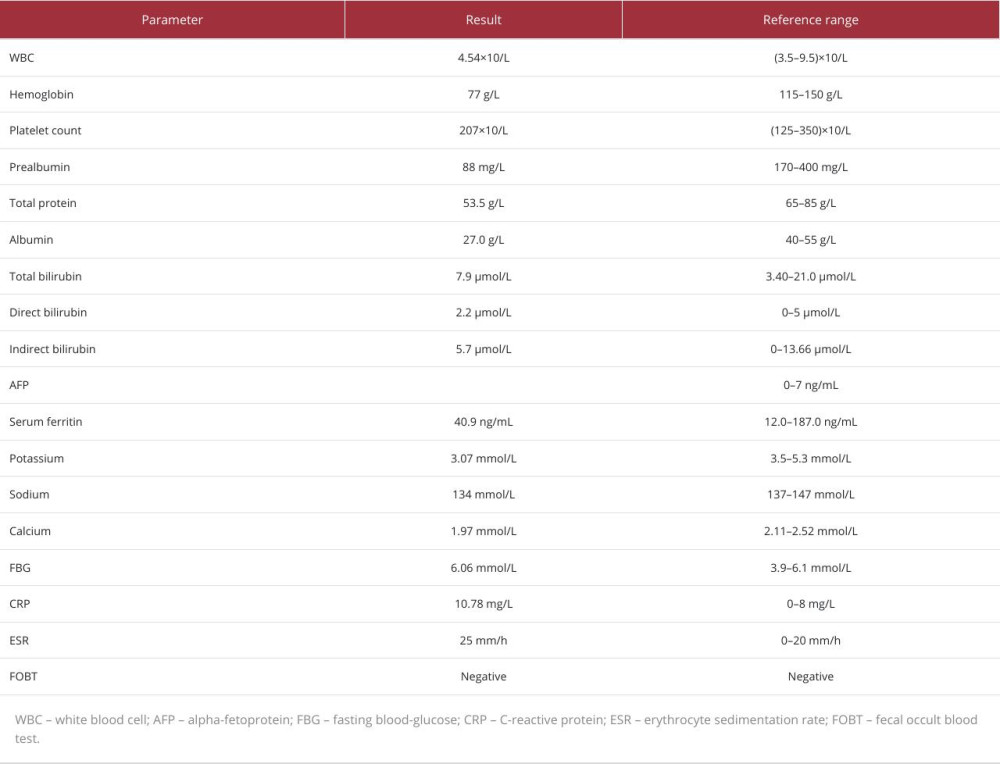
Laboratory test results showed white blood count of 4.54×109/L, low hemoglobin level of 77 g/L, platelet count of 279×109/L, low prealbumin level of 88 mg/L, low total protein level of 53.5 g/L, low albumin level of 27.0 g/L, low potassium level of 3.07 mmol/L, low sodium level of 134 mmol/L, low calcium level of 1.97 mmol/L, high C-reactive protein level of 10.78 mg/L, high erythrocyte sedimentation rate of 25 mm/h, total bilirubin level of 7.9 μmol/L, direct bilirubin level of 2.2 μmol/L, indirect bilirubin level of 5.7 μmol/L, blood glucose level of 6.06 mmol/L, and negative fecal occult blood test, and coagulation function, liver and kidney function, and 4 virus items showed no significant abnormality. The laboratory data for hematology tests and relative reference ranges are summarized in Table 1.
The examination results were as follows. (1) Gastroscopy revealed extensive scarring of the gastric mucosa and pyloric stenosis (Figure 1A). (2) Upper gastrointestinal radiography showed gastric peristalsis was slow, pyloric canal filling was poor, and gastroptosis was present (Figure 1B). (3) Computed tomography showed multiple cysts in the liver, gallbladder, and cystic duct and lower common bile duct stones, with mild intrahepatic bile duct dilatation, right renal cyst, and a small amount of bilateral pleural effusion (Figure 2A). (4) Magnetic resonance cholangiopancreatography showed cholecystitis, multiple stones in the gallbladder and common bile duct, with mild dilatation of the common bile duct, and multiple hepatic cysts (Figure 2B).
After admission, the patient was given conservative medical treatment, including acid suppression and stomach protection, fluid infusion, correction of electrolyte imbalance, parenteral nutrition support, and other treatments. Two weeks later, the patient was still unable to eat, and the symptoms of nausea and vomiting could not be relieved. The patient had poor mental status, but no professional psychiatric evaluation and consultation were performed during hospitalization, at the refusal of the patient’s family. Reexamination of upper gastrointestinal radiography still revealed slow gastric peristalsis, poor filling of the pyloric canal, and gastroptosis. Finally, surgery was performed, during which contracture of the pyloric part of the antrum was found, which was hard in consistency and widely adhered to the surrounding tissues, the fundus and body of the stomach were soft, and the gall-bladder was edematous. Gastrojejunostomy, Braun anastomosis, and nasojejunal feeding tube placement were selected for the surgical procedure. Meanwhile, cholecystectomy, choledochotomy, intraoperative choledochoscopy examination, basket stone extraction, and primary suture of the common bile duct were performed for biliary calculi. The whole operation lasted for 3 h and 5 min, and the intraoperative hemorrhagic volume was about 80 mL. The patient recovered and was discharged 9 days after surgery. At the 66-day postoperative follow-up, the patient had a good appetite, smooth eating, and no nausea, vomiting, acid regurgitation, abdominal pain, abdominal distension, jaundice, or other discomfort.
Discussion
Self-administered pesticide poisoning is a major public health problem, and at least 1 in 7 suicides worldwide are caused by self-administered pesticides [1]. Dichlorvos is an organo-phosphorus pesticide, with acute poisoning symptoms that are predominant in the early stage of poisoning and intermediate syndrome and delayed neurocognitive deficits that can occur in the late stage of poisoning [6]. Chemical corrosion of the digestive tract can cause inflammation, ulcers, bleeding, and perforation in the early stage, and later effects include pyloric obstruction, esophageal obstruction, esophageal cancer, and gastric cancer. Pyloric obstruction is often caused by a variety of malignant and benign lesions, and common nonneoplastic factors include peptic ulcer, ingestion of corrosive substances, chronic pancreatitis, non-steroidal anti-inflammatory drugs, Crohn disease, and stenosis caused by postoperative scars or adhesions. Conservative treatment is the mainstay of treatment in the early stages, and aggressive invasive intervention is required if it persists [7]. Endoscopic dilation combined with conservative treatment is very effective in the treatment of pyloric obstruction caused by ulcers, but there are still problems of recurrence [8]. For pyloric obstruction caused by corrosive injury, surgical intervention is generally required, and there are a variety of surgical methods available, including gastrojejunostomy, Billroth I, and Heineke Mickulicz pyloroplasty. Specific surgical methods currently lack a unified standard, and recently some scholars have performed a new surgical procedure, laparoscopic diamond duodenantroostomy, with the advantages of being minimally invasive and allowing early enteral nutrition [9,10]. Luo et al reported a patient with organophosphorus poisoning and pyloric obstruction who underwent distal gastrectomy with Bi-II anastomosis and jejunal feeding tube placement during the operation but developed anastomotic edema after the operation [11]. It is necessary to select the appropriate surgical approach according to the specific situation of the patient and the experience of the surgeon. In the present case, pyloric obstruction occurred 2 months after poisoning, and the causes of pyloric obstruction were analyzed, including: (1) the direct corrosion effect of the drug; (2) gastric lavage during poisoning rescue had a physical damage effect on the gastric mucosa; (3) organophosphorus inhibited AchE in the body, causing the accumulation of AchE, with increased release of epinephrine and norepinephrine, resulting in gastric wall vasospasm, increased vascular permeability, microcirculatory disturbance, causing gastric wall ischemia, edema, ulcer, and necrosis; (4) atropine, probably given as the first treatment modality for organophosphate poisoning, could precipitate acute pyloric obstruction; and (5) with smooth muscle weakness after organophosphorus poisoning, gastric emptying can be affected. After the occurrence of obstructive symptoms, conservative treatment was not effective, and finally surgical treatment with gastrojejunostomy was performed. To reduce reflux, Braun anastomosis was added. To facilitate postoperative nutritional support, a jejunal feeding tube was placed during the operation.
In addition, the patient was not found to have biliary calculous disease until this hospitalization examination due to dichlorvos poisoning. By retrospective analysis, the patient’s intermittent postprandial epigastric discomfort lasting about 1 year was most likely related to calculous disease of the biliary system. This elderly patient with biliary system stones, but no manifestations of cholangitis, was suitable for cholecystectomy and choledocholithotomy, with primary suture without an indwelling T tube. In fact, there is no causal relationship between dichlorvos poisoning and calculous disease of the biliary system in this case, but both could jointly have caused the patient’s epigastric pain. This elderly patient had multiple concurrent diseases, resulting in a relatively complex clinical situation. When developing the therapeutic regimen of patients, the surgeon needs to evaluate additional factors, such as the patient’s age, general condition, clinical symptoms, imaging examination, and mental status, to select the most appropriate treatment plan. Also, it is important to consider the physical tolerance of patients when performing multiple concomitant surgical procedures simultaneously, as the surgery itself is also a trauma.
Notably, the patient still developed apathy after surgery during hospitalization, which may have been related to the sequelae of the central nervous system following dichlorvos poisoning, psychological trauma after the suicide attempt, or prolonged pyloric obstruction for more than 2 weeks, which resulted in deficiencies of some trace elements, minerals, and vitamins. Wernicke encephalopathy, caused by vitamin B1 deficiency, may have caused the patient’s psychiatric symptoms. After follow-up, the patient had good food intake, weight gain, and improved mental status and was without acid regurgitation, jaundice, abdominal pain, or other symptoms.
Conclusions
Dichlorvos poisoning has a significant physical and mental impact on patients after pyloric obstruction, requiring active treatment. Gastrojejunostomy plus Braun anastomosis is an effective surgical approach for an elderly patient. Meanwhile, according to the condition of the biliary calculi and the width and inflammatory edema of common bile duct, surgeons must evaluate whether to perform primary anastomosis to avoid a long-term postoperative indwelling T tube, reduce the discomfort of patients with a T tube, and improve the prognosis of patients. This complicated case of concomitant diseases provides useful considerations for subsequent clinical diagnosis and treatment.
Figures
References:
1.. Mew EJ, Padmanathan P, Konradsen F: J Affect Disord, 2017; 219; 93-104
2.. Ben Salem I, Boussabbeh M, Pires Da Silva J, Effects of Dichlorvos on cardiac cells: Toxicity and molecular mechanism of action: Chemosphere, 2023; 330; 138714
3.. Hall AH, Jacquemin D, Henny D, Mathieu L, Corrosive substances ingestion: A review: Crit Rev Toxicol, 2019; 49(8); 637-69
4.. Podboy A, Gaddam S, Park K, Management of difficult choledocholithiasis: Dig Dis Sci, 2022; 67(5); 1613-23
5.. Manes G, Paspatis G, Aabakken L, Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline: Endoscopy, 2019; 51(5); 472-91
6.. Dassanayake TL, Weerasinghe VS, Gawarammana IB, Buckley NA, Changes of attention-related brain activity over 6 months after acute organophosphate pesticide poisoning: A prospective follow-up study: Clin Toxicol (Phila), 2022; 60(5); 576-84
7.. Papanikolaou IS, Siersema PD, Gastric outlet obstruction: Current status and future directions: Gut Liver, 2022; 16(5); 667-75
8.. Hamzaoui L, Bouassida M, Ben Mansour I, Balloon dilatation in patients with gastric outlet obstruction related to peptic ulcer disease: Arab J Gastroenterol, 2015; 16(3–4); 121-24
9.. Soomro MA, Aftab M, Hasan M, Arbab H, Heineke-Mikulicz pyloroplasty for isolated pyloric stricture caused by corrosive ingestion in children: Pak J Med Sci, 2020; 36(1); S87-S90
10.. Seleim HM, Wishahy AMK, Abouelfadl MH, Laparoscopic diamond antroduodenostomy for postcorrosive pyloric cicatrization: A novel approach: J Laparoendosc Adv Surg Tech A, 2019; 29(4); 538-41
11.. Luo W, Lu T, Li F, Surgical treatment of pyloric stenosis caused by glypho-sate poisoning: A case report: Medicine (Baltimore), 2019; 98(30); e16590
Figures
In Press
24 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943560
26 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943893
27 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942126
27 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943098
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250