23 September 2020: Articles 
Take Me Higher: A Case of Heart Failure at High Altitude Detected Using the CardioMEMS™ HF System
Unusual clinical course, Challenging differential diagnosis, Unusual setting of medical care
Marcel M. Letourneau1ABCDEF*, Daniel Brancheau2ABCDEFG, Jessica Estes3CD, Marcel Zughaib1ABCDEFGDOI: 10.12659/AJCR.922857
Am J Case Rep 2020; 21:e922857
Abstract
BACKGROUND: The heart failure patient population can be challenging to treat and monitor. This is especially true when they travel to high altitudes where changes in pressure can affect their clinical status. The CardioMEMS™ HF System (Abbott Cardiovascular, Abbott Park, IL, USA) is an implanted miniature wireless device located in the pulmonary artery that transmits data on pulmonary artery pressure and heart rate. This data can be used to detect this dramatic invasive pressure change.
CASE REPORT: We present the case of a 78-year-old man with an exacerbation of heart failure while traveling to high altitude. Elevation of his pulmonary artery (PA) pressures were detected by his implanted CardioMEMS device. Understanding the expected change in PA pressure recordings helped to identify a true exacerbation of heart failure in our patient. This led to a prompt change in medical therapy, which ultimately prevented hospitalization.
CONCLUSIONS: Increased elevation can lead to falsely elevated PA pressure readings by the CardioMEMS device. However, we present the case of a patient with a disproportionate elevation of his hemodynamic pressure measurements, indicating an exacerbation of heart failure. This case demonstrates the value of the CardioMEMS device in detecting PA pressure changes in these unique circumstances.
Keywords: arterial pressure, Atmospheric Pressure, Blood Pressure Monitors, Pulmonary Artery, Altitude, Blood Pressure Monitoring, Ambulatory, Hospitalization
Background
In an age where heart failure (HF) is endemic, technological and pharmacological advances have had a significant impact on the care of this patient population and their quality of life. One such technology is the implantable PA sensor CardioMEMS device. Under the appropriate indications, implantation of this device has led to targeted treatment of this complex patient population and has reduced hospitalization by 37–70% [1]. CardioMEMS gives healthcare providers the ability to accurately measure invasive hemodynamic pressures in the PA. Importantly, recorded pressures are not only dependent on clinical status, but may also be affected by the atmospheric pressure of their environment, a fact that is not widely appreciated by many health care providers. The CardioMEMS device is initially calibrated at the atmospheric pressure of implantation. Large changes in elevation lead to changes in atmospheric pressure, which will affect the accuracy of the CardioMEMS HF system by a factor of approximately 2 mmHg per 305 m (1000 ft) of elevation change [2]. CardioMEMS does not currently have an active “correction” of pressure change when patients travel to different altitudes, which health care providers must be aware of as they actively monitor their heart failure patients.
When HF patients with CardioMEMS implanted at low altitudes travel to higher altitudes, the physician must consider the expected variation in pressures while the patient is at that altitude. Higher altitudes have a lower barometric pressure and lower fraction of inspired oxygen (FiO2.) Reduction in barometric pressure leads to “hypobaric hypoxia” due to a decrease in alveolar O2 partial pressure [3]. This simulates a hypoxic state, which can be especially problematic for HF patients with sensitive clinical status. We present a case of a CardioMEMS-implanted patient who traveled to higher elevation and experienced worsening symptoms and changes in pulmonary hemodynamics.
Case Report
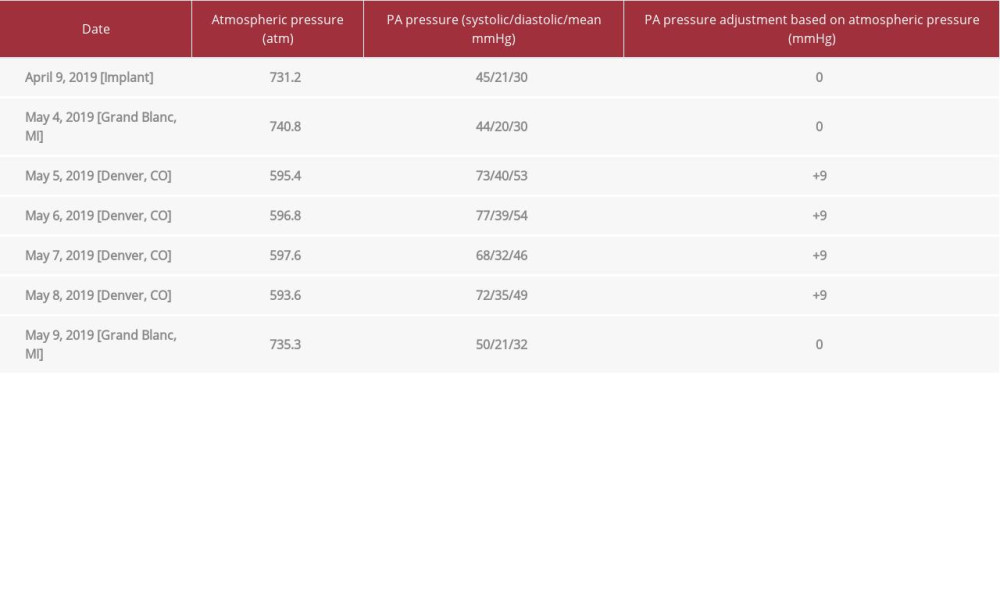
We present the case of a 78-year-old man with known history of chronic atrial fibrillation, hypertensive heart disease, and nonischemic cardiomyopathy. He had a global reduction in left ventricular ejection fraction of 40–45%, and his echo-cardiogram was without significant abnormality. The patient had been followed in the cardiac outpatient clinic, where he was treated for American College of Cardiology (ACC) stage C chronic heart failure with New York Heart Association (NYHA) class III symptoms. Despite several changes in his diuretics and attempts to control his fluid status, he had a 40-pound weight gain over a 3-month period, with significant increase in shortness of breath. As his decompensation of heart failure progressed, he was hospitalized for 8 days and treated with intravenous (IV) furosemide. Because of his NYHA classification and admission to the hospital for heart failure exacerbation, invasive hemodynamic monitoring with CardioMEMS implantation was indicated and performed. Implantation of his CardioMEMS was performed in Grand Blanc, Michigan at an altitude of 837 feet with an atmospheric pressure of 731.2 on April 9, 2019. Initial hemodynamic measurements from cardiac catheterization showed a PA systolic pressure of 45 mmHg, PA diastolic pressure of 16 mmHg, and a mean PA pressure of 30 mmHg. The right atrial pressure was 21 mmHg, right ventricular pressure was 44/17 mmHg, and the pulmonary wedge mean pressure was 24 mmHg. The procedure was completed without complications and the patient was discharged the same day.
After implantation of the CardioMEMS, the patient remained stable for 4 weeks without worsening symptoms of heart failure. He was compliant with his daily CardioMEMS readings with a PA mean ranging between 27 to 31 mmHg, and PA diastolic pressure 17 to 21 mmHg (Figure 1) These overall hemodynamic findings were stable compared to those at the time of implant.
The patient then visited Denver, Colorado for 4 days at an altitude of 5280 feet with an atmospheric pressure of 596.8 atm on May 5, 2019. Recordings from the first day of his visit showed a PA systolic pressure rise from 44 mmHg to 73 mmHg, PA mean pressure rise from 30mmHg to 53 mmHg, and PA diastolic pressure rise from 20 mmHg to 40 mmHg. Concomitantly, he noticed a significant increase in shortness of breath and lower-extremity swelling. He did not seek medical attention but instead contacted his primary cardiologist in Michigan. His baseline nasal canula oxygen was increased from 1 liter to 2 liters and his furosemide does was doubled from 40 mg daily to twice daily. Fortunately, this treatment improved the patient’s symptoms and prevented a hospital admission. Because hospital admission was avoided, laboratory values, diagnostic imaging, and clinical vital signs were not available.
Throughout his 4-day hospital stay, his invasive pressures remained high but slowly decreased and stabilized with a PA systolic of 72 mmHg, PA mean of 49 mmHg, and a PA diastolic of 35 mmHg on the day prior to returning to Michigan. On the fifth day, he returned to Michigan and his invasive pressure measurements normalized quickly, with a PA mean pressure of 29 mmHg and a PA diastolic pressure of 20 mmHg (Figure 2). He has continued to do well while in Michigan on continued maintenance diuretics and daily monitoring of PA pressures with his CardioMEMS device.
Discussion
Since CardioMEMS gained FDA approval in May 2014 for hemodynamic monitoring of patients who have been hospitalized at least once in the preceding 12 months with NYHA class III heart failure, the device has had an increasing role in treating patients with heart failure. Results of the CardioMEMS postapproval study were presented at ACC 2019 [4]. This study found that 1214 patients meeting CHAMPION trial enrollment criteria with CardioMEMS implantation were 58% less likely to have a heart failure-related hospitalization in the following year [4].
As the number of CardioMEMS implantation continues to grow, nuances related to accurate interpretation of the data need to be familiar to the treating health care provider. One such clinical scenario is related to the effect of elevation, and therefore atmospheric pressure, on patient data. This is especially true with modern travel options that allow even patients with significant disabilities and physical limitations to reach higher-altitude destinations.
To highlight this point, our patient traveled from 837 feet in Grand Blanc, Michigan to 5280 feet in Denver, Colorado, with an absolute elevation difference of 4443 feet. Based on this elevation change, the expected “usual” rise in CardioMEMS PA pressure measurement is approximately 9 mmHg (Table 1). Despite accounting for this expected “if adjusted” PA pressure based on the implantation elevation, the patient had an additional rise of 14 mmHg of his mean PA pressure. He also had elevation of PA diastolic pressure to 40 mmHg, demonstrating an exacerbation of heart failure. Although it is not possible to determine the exact cause of his heart failure decompensation, we believe it was most likely secondary to a decrease in PO2 with acute altitude sickness. It is also possible that contributing factors such as medical noncompliance during traveling, colder environment, or concomitant infection could have contributed to his decompensation.
As altitude increases, a series of physiological responses helps to acclimatize the patient so that tissue O2 delivery is adequate. Worsening pulmonary hypertension caused by the body’s physiological response in order to increase ventilation, cardiac output, and tissue oxygenation places further stress on the heart in patients with low cardiac reserve. Alveolar hypoxia activates peripheral chemoreceptors, leading to increased pulmonary vascular resistance and pulmonary artery pressure, either directly though induction of hypoxic pulmonary vasoconstriction (HPV) or through activation of the sympathetic nervous system [3]. HPV is essential in utero and also in lung disease, as it directs blood flow towards well-oxygenated areas of the lungs. However, when exposed to global hypoxia, this can lead to extensive HPV, which can quickly deteriorate the condition of a patient with low cardiac reserve. This forces an increase in cardiac output with submaximal workloads, especially if the right ventricle is unable to compensate [5].
Importantly, this case demonstrates real-time hemodynamic and physiologic changes in a HF patient at high altitude. Currently, high altitude physiologic changes have only been demonstrated in the laboratory setting, by monitoring PA pressure of patients undergoing VO2 testing with administration of lower concentrations of FiO2 corresponding to the environmental changes seen at an increased altitude [3,6]. A lack of clinical trials exploring this scenario further reinforces the need for additional research addressing exposure to high altitude in heart failure patients. The CardioMEMS implantable device is a valuable hemodynamic monitoring tool that can be used to facilitate research in patients with heart failure traveling to high altitude.
Conclusions
We presented a case of a 78-year-old man with an implanted CardioMEMS device traveling to high altitudes. This travel caused an exacerbation of heart failure, with increased recorded PA pressures higher than that expected after accounting for atmospheric pressure change. Currently, the CardioMEMS heart failure system does not have an automated compensatory program to correct for patient elevation, and it is important to realize that the CardioMEMS sensor is calibrated at implant atmospheric pressure. Changes to that atmospheric pressure, such as travel to high altitude, can cause a “false elevation” in measured PA pressures. The monitoring health care providers should be aware of these elevations, as patients can have exacerbation of heart failure while traveling to high altitudes, as we have shown here. Future refinements in the CardioMEMS technology and software may be able to readily autocorrect to atmospheric pressure. This will eliminate the need for “correction” of invasive pressure readings when traveling to different altitudes.
Figures
References:
1.. Givertz MM, Stevenson LW, Costanzo MR, Pulmonary artery pressure-guided management of patients with heart failure and reduced ejection fraction: J Am Coll Cardiol, 2017; 70(15); 1875-86
2.. , System PA Sensor and Delivery System. User’s Manual Accessed 07/2019
3.. Parati G, Agostoni P, Basnyat B, Clinical recommendations for high altitude exposure of individuals with pre-existing cardiovascular conditions: A joint statement by the European Society of Cardiology, the Council on Hypertension of the European Society of Cardiology, the European Society of Hypertension, the International Society of Mountain Medicine, the Italian Society of Hypertension and the Italian Society of Mountain Medicine: Eur Heart J, 2018; 39(17); 1546-54
4.. Shavelle D, Desai AS, Abraham WT, Pulmonary artery pressure-guided therapy for ambulatory heart failure patients in clinical practice: 1-year outcomes from the CardioMEMS post-approval study: Am Coll Cardiol Meet, 2019 Abstract
5.. Bärtsch P, Gibbs JS, Effect of altitude on the heart and the lungs: Circulation, 2007; 116(19); 2191-202
6.. Sutton JR, Houston CS, Mansell AL, Effect of acetazolamide on hypoxemia during sleep at high altitude: N Engl J Med, 1979; 301(24); 1329-31
Figures
In Press
04 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.941835
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943042
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942578
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943801
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250