28 July 2020: Articles 
Essential Thrombocythemia Presenting with Recurrent Priapism: A Case Report and Review of Literature
Unusual clinical course
Shailendra Prasad Verma1E*, Nidhish Kumar1F, Mili Jain2C, Anil K. Tripathi1FDOI: 10.12659/AJCR.924455
Am J Case Rep 2020; 21:e924455
Abstract
BACKGROUND: Priapism is rarely reported as a complication in patients with essential thrombocythemia at presentation. We could find very few such cases of essential thrombocythemia while searching the literature. A combined modality of treatment is used in the form of chemotherapy and procedures like repeated aspiration and instillation of phenylephrine to treat essential thrombocythemia presenting with recurrent priapism.
CASE REPORT: A 31-year-old man presented to the Urology Department with priapism for the last 24 h. He had previously had multiple similar episodes in the last 20 days and 1 episode of prolonged penile erection 5 months ago. On examination, his penis was erect, swollen, and painful. There was no organomegaly. The priapism was managed with repeated aspiration and instillation of phenylephrine. Routine investigations showed marked thrombocytosis. Subsequent investigations done in the Clinical Hematology Department revealed increased megakaryocytes in bone marrow and presence of JAK2V617F mutation. After confirmation of diagnosis, cytoreductive therapy (hydroxyurea 500 mg twice a day) and acetyl salicylic acid 75 mg once a day was initiated. With this treatment, the platelet count normalized over a period of 2 months and no further episodes of priapism were noted; however, the patient developed erectile dysfunction.
CONCLUSIONS: Essential thrombocythemia can present with priapism as the first manifestation. Early suspicion, diagnosis, and management is needed to prevent erectile dysfunction. Erectile dysfunction is usually irreversible after long-standing priapism.
Keywords: Erectile Dysfunction, myeloproliferative disorders, Priapism, Thrombocythemia, Essential, Aspirin, Cytoreduction Surgical Procedures, Hydroxyurea, Platelet Aggregation Inhibitors, Recurrence
Background
Priapism is an unwanted prolonged penile erection without any sexual arousal. It has been reported in patients with various non-malignant and malignant hematological disorders, including myeloproliferative neoplasms. Chronic myeloid leukemia (CML) is the most common myeloproliferative neoplasm (MPN) associated with priapism [1–3]. It is rarely reported as a complication in patients with essential thrombocythemia. We could find only a few cases in the recent literature [4–7]. A combined modality treatment is being used in the form of chemotherapy and procedures like repeated aspiration and instillation of phenylephrine to treat essential thrombocytosis presenting with recurrent priapism [8,9].
Case Report
A previously healthy 31-year-old man was admitted to the Urology Department with a history of penile erection that began the previous day. His penis was erect, swollen, and painful. There was no history of any drug intake, sexual activity, masturbation, use of alcohol, or any illicit drug use. The patient gave a history of many similar previous episodes lasting for many hours with spontaneous recovery in the last 20 days. He also had a history of one such episode 5 months ago that was relieved by conservative management. He was referred to the Clinical Hematology Outpatient Department for evaluation of abnormal blood test results. The general examination was otherwise unremarkable; there were no pallor, lymphadenopathy, or hepatosplenomegaly.
Laboratory investigations showed hemoglobin 13 gm/dl, total leucocyte count 18.3×109/L, and platelet count 1424×109/L. A peripheral blood smear examination revealed thrombocytosis with giant platelets (Figure 1). Bone marrow aspirate and biopsy showed increased numbers of megakaryocytes, with giant and bizarre megakaryocytes present in nests (Figure 2). JAK2V617F mutation was detected and BCR-ABL by RT-PCR was negative. Serum biochemical test results were unremarkable.
This patient was managed conservatively by repeated aspiration of corpora cavernosa and instillation of phenylephrine in the Urology Department. With repeated aspiration and instillation of phenylephrine, the penis become flaccid. After the confirmation of diagnosis, the patient received hydroxyurea 500 mg twice a day, and acetyl salicylic acid 75 mg once a day was added when platelet count decreased below 1000×109/L. Subsequent to treatment with hydroxyurea and acetyl salicylic acid, no episode of priapism was noted. His platelet count decreased to below 400×109/L at the end of 2 months. As a consequence of prolonged priapism, he developed erectile dysfunction (ED), which did not improve, even at 6-month follow-up.
Discussion
Priapism is a sustained penile erection in the absence of sexual activity. It is generally defined as an unwanted erection lasting more than 4 h [10]. It can be high-flow or low-flow. High-flow priapism is due to increased blood influx into the cavernous bodies, usually due to an arteriocavernosal fistula. It is also called nonischemic, as cavernous blood gases are neither hypoxic nor acidotic. Low-flow priapism has a veno-occlusive origin and is known as ischemic priapism because diminished blood efflux from the cavernous bodies causes hypoxic and acidotic cavernous blood gases [6]. Ninety percent of men with ischemic priapism lasting more than 24 h develop erec-tile dysfunction. Ischemia persisting for more than 24–48 h causes endothelial damage and trabecular destruction leading to irreversible fibrosis and calcification, resulting in ED [11].
Priapism is a urological emergency. Hematological conditions may be associated with major episodes of priapism, as well as stuttering priapism (recurrent temporary episodes of priapism). Well-documented hematological conditions causing priapism are hemolytic disorders (e.g., homozygous sickle cell disease); myeloproliferative neoplasms (e.g., chronic myeloid leukemia [CML] and polycythemia vera [PV]); acute leukemia (e.g., acute myeloblastic leukemia [AML] and acute lymphoblastic leukemia [ALL] with high counts); plasma cell disorders (e.g., myeloma and amyloidosis); and hypercoagulable states. Sickle cell disease is the most common hematological disorder, while CML is the most common leukemia associated with priapism [3,12].
The pathophysiology of priapism in hematological conditions includes hyperleukocytosis leading to aggregates of leukemia cells in the corpora cavernosa in CML and acute leukemias, clogging by RBCs in sickle cell disease, and stasis of platelets in essential thrombocytosis leading to low-flow (ischemic) priapism [4,8,12].
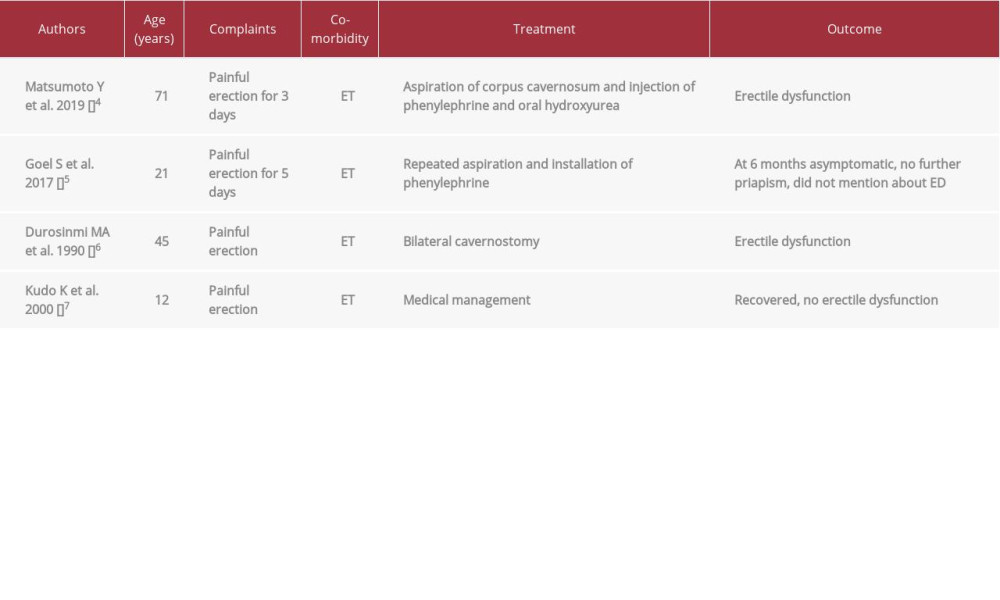
According to a 2016 WHO report, essential thrombocytosis (ET) is a chronic myeloproliferative neoplasm (MPN) that primarily involves the megakaryocytic lineage. It is characterized by sustained thrombocytosis ≥450×109/L in peripheral blood, increased numbers of large mature megakaryocytes in bone marrow, exclusion of CML, PV, and MDS, and presence of JAK-2, CALR, or MPL mutation. Other causes of thrombocytosis must be excluded, including other MPNs [13]. Clinically, ET is characterized by episodes of thrombosis and/or hemorrhage. In ET, priapism is a very rare complication and only a few cases are found in the literature. Table 1 shows the review of similar cases reported in the literature.
When priapism is associated with a hematological condition, adult guidelines recommend systemic treatment of the underlying disorder along with intra-cavernous treatment to minimize the duration of erection and the risk of consequent long-term ED [14,15]. Conservative approaches like apheresis and chemotherapy (e.g., steroids, hydroxyurea, and imatinib) can manage many patients, especially children [14]. Aspiration of corpora cavernosa and instillation of phenyl ephrin can be tried in adults with severe and prolonged symptoms for rapid response and flaccidity of the penis. If these procedures also do not work, surgical correction (e.g., cavernosa-corpus spongiosum shunt) can be tried [1,16,17].
Conclusions
Clinicians should consider essential thrombocythemia in patients presenting with recurrent priapism. It should be suspected early and investigated promptly. General measures, cytoreduction, and evacuation of the corpora cavernosa should be done early to avoid erectile dysfunction. Once the etiological diagnosis is confirmed, specific therapies targeting the underlying neoplasm can be started.
References:
1.. Qu M, Lu X, Wang L, Priapism secondary to chronic myeloid leukemia treated by a surgical cavernosa-corpus spongiosum shunt: Case report: Asian J Urol, 2019; 6(4); 373-76
2.. Kumar P, Rahman K, Kumari S, Priapism as a rare presentation of chronic myeloid leukemia: J Cancer Res Ther, 2018; 14(6); 1442-43
3.. Bacerra-Pedraza LC, Jimenez-Martinez LE, Pena Morfin I, Priapism as the initial sign in Hematologic disease: Case report and literature review: Int J Surg Case Rep, 2018; 43; 13-17
4.. Matsumoto Y, Amano T, Shimojima T, [Ischemic priapism associated with essential thrombocythaemia: A case report]: Hinyokika Kiyo, 2019; 65(7); 315-17 [in Japanese]
5.. Goel S, Sokal AS, Singh BP, Aggarwal A, Priapism due to essential thrombocythemia: a rare causation: BMJ Case Rep, 2017; 2017; bcr2017221116
6.. Durosinmi MA, Badejo OA, Ayoade BA, Odelana CO, Essential thrombocythemia associated with priapism: A case report: East Afr Med J, 1990; 67(8); 594-95
7.. Kudo K, Horibe K, Jwasw K, [Clinical features of essential thrombocythemia in three children]: Rinsho Ketsueki, 2000; 41(11); 1164-70 [in Japanese]
8.. Keoghane SR, Sullivan ME, Miller MA, The aetiology, pathogenesis and management of priapism: BJU Int, 2002; 90; 149-54
9.. Muneer A, Alnajjar HM, Ralph D, Recent advances in the management of priapism: F1000Res, 2018; 7; 37
10.. Bondil P, Carnicelli D, Priapism: Rev Prat, 2017; 67(6); 632-35
11.. Hudnall M, Reed-Maldonado AB, Lue TF, Advances in understanding of priapism: Transl Androl Urol, 2017; 6(2); 199-96
12.. Wang HH, Herbst KW, Rothman JA, Trends in sickle cell disease-related Priapism in U.S. Children’s hospitals: Urology, 2016; 89; 118-22
13.. Arber DA, Orazi A, Hasserjia R, The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia: Blood, 2016; 127; 2391-405
14.. Anele UA, Le BV, Resar LM, Burnett AL, How I treat priapism: Blood, 2015; 125(23); 3551-58
15.. Montague DK, Jarrow J, Broderick GA, American Urological Association Guideline on the management of priapism: J Urol, 2003; 170; 1318-24
16.. Rodgers R, Latif Z, Copland M, How I manage priapism in chronic myeloid leukemia patients: BMJ, 2012; 158; 155-54
17.. Castagnetti M, Sainate L, Giona F, Conservative management of priapism secondary to leukemia: Pediatr Blood Cancer, 2008; 51; 420-23
Figures
In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250