20 November 2020: Articles 
A Case of Bacteremia and Prosthetic Valve Endocarditis in a 68-Year-Old Vietnamese Man
Management of emergency care, Rare disease
Pham Dang Hai1ABDEF, Pham Nguyen Son2AEF, Nguyen Thi Thu Huong3EF, Nguyen Thanh Binh1BF, Le Thi Viet Hoa4ABDEF*, Nguyen Manh Dung1EFDOI: 10.12659/AJCR.925752
Am J Case Rep 2020; 21:e925752
Abstract
BACKGROUND: Streptococcus thoraltensis is a rare cause of human disease. This report describes a patient with infective endocarditis caused by S. thoraltensis and complicated by ischemic stroke.
CASE REPORT: A 68-year-old man was admitted for a 12-day duration of fever. He had a history of severe aortic valve stenosis, for which he underwent prosthetic valve replacement, and type 2 diabetes mellitus. Echocardiography revealed vegetation attached to the right coronary cusp of the prosthetic aortic valve and rupture of the sinus of Valsalva into the right ventricle. Blood cultures were positive for S. thoraltensis. He experienced an ischemic stroke involving the vegetation of the aortic valve and died of acute heart failure.
CONCLUSIONS: S. thoraltensis may be considered an emerging pathogen in patients with infective endocarditis.
Keywords: Communicable Diseases, Emerging, Endocarditis, Sepsis, Asians, Bacteremia, Diabetes Mellitus, Type 2, Endocarditis, Bacterial, Heart Valve Prosthesis, Streptococcus
Background
Case Report
A 68-year-old man with a fever for 12 consecutive days and highest body temperature of 39.5°C was admitted to our hospital in Vietnam. He had a history of type 2 diabetes mellitus and aortic valve stenosis, for which he underwent prosthetic valve replacement 2 years earlier. He did not report chest pain, shortness of breath, weight loss, or joint pain. He had not been in recent contact with pigs or rabbits and had not undergone a dental procedure or surgical intervention within 6 months before admission.
On examination, the patient’s temperature was 38°C, his heart rate was 80/min, his respiratory rate was 18/min, his blood pressure was 120/70 mmHg, and his oxygen saturation was 92% in room air. A physical examination revealed normal lung sounds and a 3/6 pansystolic murmur at the lower left border of the sternum. The results of other clinical examination were unremarkable.
Initial laboratory analysis showed leukocytosis with a white blood cell (WBC) count of 13.9×109/L, including 92.7% neutrophils, a hemoglobin concentration of 129 g/L, thrombocytopenia with a platelet counts of 138×109/L, hyperglycemia with a glucose concentration of 19.1 mmol/L, and a procalcitonin concentration of 0.613 ng/ml.
Transthoracic and transesophageal echocardiography revealed a 12×8 mm vegetation attached to the right coronary cusp of the prosthetic aortic valve and rupture of the sinus of Valsalva into the right ventricle.
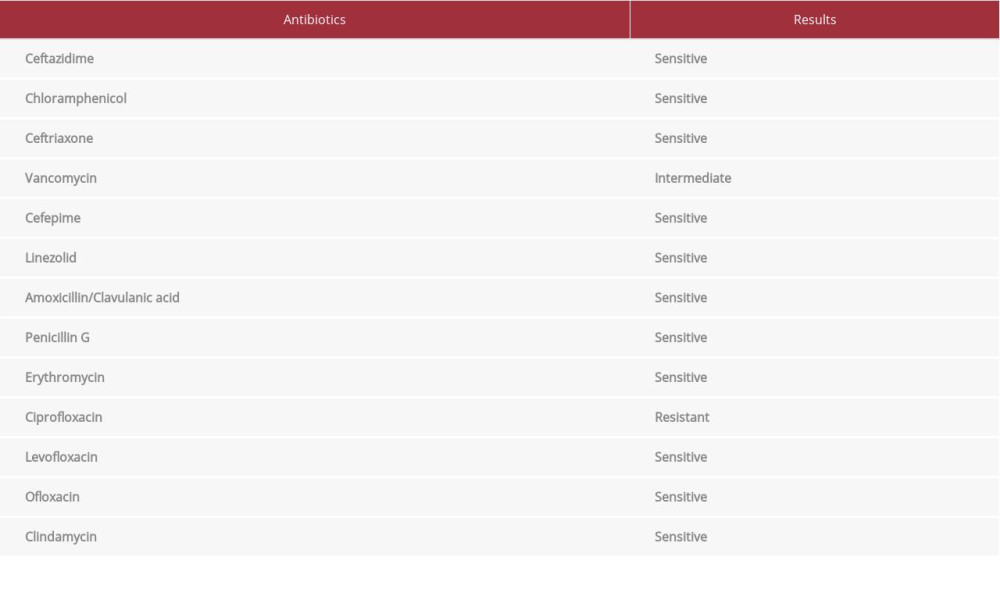
Blood was drawn for culturing 3 times every 12 hours and he was started on empirical antibiotic therapy with linezolid 600 mg twice daily plus levofloxacin 750 mg once daily. He was also administered insulin 30/70 of 30 UI daily for blood glucose control. The Vitek 2 automated system showed that 3 individual blood cultures were positive for
Seven day later, he experienced sudden left hemiparesis and left facial palsy, with a Glasgow score of 12. Urgent computed tomography of the brain revealed an acute ischemic stroke due to middle cerebral artery M1 occlusion. The patient underwent mechanical thrombectomy successfully. On day 15, he was no longer febrile, his WBC count was 9.9×109 L, with 75.9% neutrophils, and his blood culture was negative.
On day 27, he presented with severe dyspnea, tachycardia, and hypotension. Endotracheal intubation was performed, and he was treated with inotropic agents and diuretics. However, he experienced a sudden cardiac arrest and died on day 30.
Discussion
The first reported human infection with
The vegetation in the prosthetic aortic valve of our patient was large, measuring (12×8 mm). Vegetations larger than 10 mm have been reported to increase the risk of embolism, suggesting that a large vegetation is a risk factor for embolic events [7].
Conclusions
References:
1.. Devriese LA, Pot B, Vandamme P: Int J Syst Bacteriol, 1997; 47(4); 1073-77
2.. Vukonich M, Moline H, Chaussee M: S D Med, 2015; 68(7); 298-99
3.. Wazir M, Grewal M, Jain AG, Everett G: Cureus, 2019; 11(9); e5659
4.. Petridis N, Apsemidou A, Kalopitas G: Case Rep Infect Dis, 2018; 2018; 7956890
5.. AlWakeel SS, Microbiological and molecular identification of bacterial species isolated from nasal and oropharyngeal mucosa of fuel workers in Riyadh, Saudi Arabia: Saudi J Biol Sci, 2017; 24(6); 1281-87
6.. Al-Tamimi M, Himsawi N, Abu-Raideh J: Microb Drug Resist, 2019; 25(3); 421-26
7.. Mohananey D, Mohadjer A, Pettersson G, Association of vegetation size with embolic risk in patients with infective endocarditis: A systematic review and meta-analysis: JAMA Intern Med, 2018; 178(4); 502-10
8.. Dhotre S, Suryawanshi N, Nagoba B: Indian J Dent, 2014; 5(Suppl.); 140-41
9.. Bustami N, Mismar A, Obeidat F: J Clin Case Rep, 2019; 9(2); 1212
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943420
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942824
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250