30 July 2020: Articles 
Undersized Stentgraft Placement for Traumatic Descending Aorta Rupture, and What Is Next?
Unusual clinical course, Mistake in diagnosis, Diagnostic / therapeutic accidents, Management of emergency care, Educational Purpose (only if useful for a systematic review or synthesis)
Mirosław Dziekiewicz1ABDEF*, Grażyna Laska1BD, Karol Makowski2DEFDOI: 10.12659/AJCR.926299
Am J Case Rep 2020; 21:e926299
Abstract
BACKGROUND: Traumatic injury of the thoracic aorta is proving to be not only the most lethal of traumatic injuries, but also the most urgent reason for vascular intervention among all trauma patients. Endovascular aortic repair is used increasingly often to treat traumatic injuries. We report a case of endovascular treatment and its use as a delayed correction (two-stage treatment) for a traumatic aortic isthmus rupture.
CASE REPORT: A 20-year-old Asian male was admitted to our department after a car accident presenting symptoms of ischemic shock. Among multiple injuries, a traumatic descending aorta rupture was diagnosed. The patient was referred directly to the operating room for a thoracic endovascular aortic repair (TEVAR). The patient’s other trauma-related injuries required additional interventions in the following days. Thirty days after the emergent TEVAR operation, the patient required reintervention due to a major type-I endoleak. Computed tomography angiography revealed a failed stentgraft deployment. We removed the mismatched endovascular equipment and deployed an appropriately sized stentgraft during a hybrid procedure, excluding the ruptured aortic wall altogether.
CONCLUSIONS: Endovascular treatment of both children and small-framed adults remains a challenge for operating teams. First, no dedicated equipment can be found on the market. Second, measuring and fitting endovascular equipment constitutes a sore point in treatment, so in emergency situations, only off-the-shelf tools are accessible. We assert that, in such cases, the primary procedure should be understood as a lifesaving intervention, awaiting a final and long-lasting solution.
Keywords: Aorta, Thoracic, endovascular procedures, Vascular System Injuries, Accidents, Traffic, computed tomography angiography, Prosthesis Fitting, Rupture, Self Expandable Metallic Stents, young adult
Background
Road traffic accidents, crush injuries, falls from height, and other deceleration accidents that occur during sports such as skiing are the main causes of aortic trauma [1–4]. The patho-physiology of blunt thoracic aortic injury (BAI) is compounded by its anatomical position. Most thoracic aortic injuries clearly result from the aorta’s anatomical position right in the middle of the rib cage. The region of the isthmus is especially prone to injury. In adults, minimally invasive procedures are nowadays a largely accepted method of treatment [5–7]. For most pediatric patients, however, the current standard of care remains open surgical repair. A growing body, including the aorta, does not function well with stentgraft usage, causing problems in this cohort of patients.
The problem persists when we deal with undersized aortas in adults. No dedicated endovascular tools exist for these cases, which means we have to implement ad hoc solutions [8,9]. Measuring and fitting appropriate endovascular equipment in hemorrhagic young patients is yet another problem. Their aortas are able to shrink due to the autonomic reflex, making the computed tomography angiography (CTA) assessment far from perfect.
Case Report
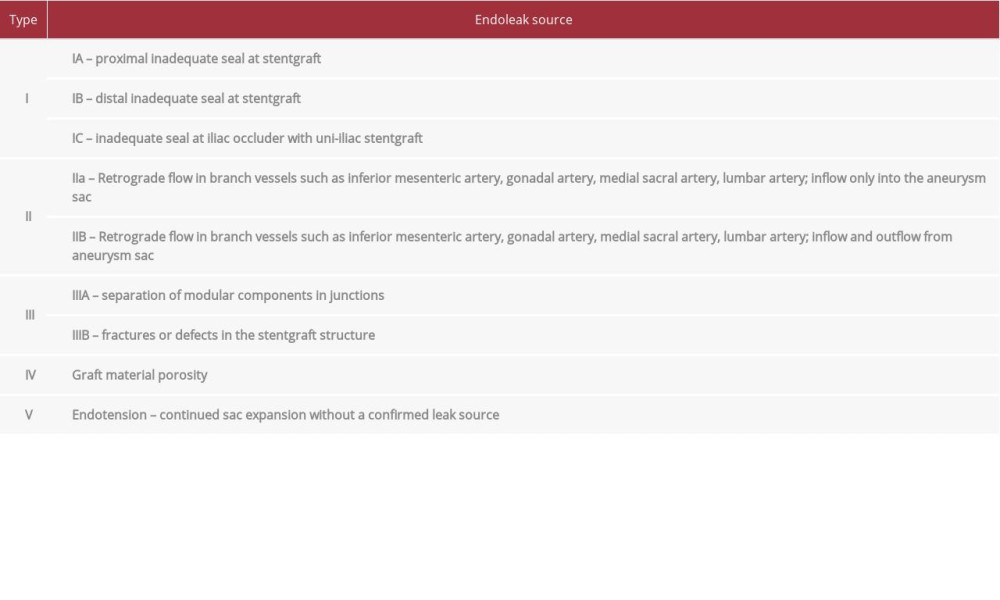
We present a case of a 153-cm tall, 55-kg Asian male taxi driver in his twenties, who was wounded in a traffic collision. He was diagnosed with trauma to the head with intracranial hematoma and maxillofacial fractures, lung and liver contusion, multiple fractures of the ribs, and left pneumothorax and pelvic fractures. The CTA revealed an aortic isthmus rupture as a major life-threatening bleeding source. This exam also revealed an aortic pseudoaneurysm with associated posterior mediastinal hematoma and multifocal pulmonary contusion. The patient was transferred to the Department of Vascular and Endovascular Surgery of the Trauma Centre (* Military Institute of Medicine, Warsaw). Preoperative analysis of the chest CTA indicated a 15×10-mm area of focal damage to the medial aspect of the descending aorta, located right underneath the isthmus, and an associated 60-mm pseudoaneurysm. The aortic arch was 12—12.5 mm in diameter, and located distally to the disruption (Figure 1). We focused on this aspect of the problem. Since an intracranial hemorrhage was detected, we evaluated standard systemic anticoagulation to be high risk for the patient. Hence, the whole procedure was performed without heparin administration. The available stentgraft sizes were approximately 30% larger than our patient’s aorta size so we had to come up with a different option on the spot. Autonomic vasoconstriction of the aorta caused by the hemorrhagic shock made our preoperative measuring of the main artery difficult. We decided to implant a balloon-expandable covered stent. We obtained the femoral access and put a pigtail catheter through the femoral artery, retrograde into the ascending aorta. This was followed by an angiogram. Using CTA and the intraoperative angiogram, we fitted a balloon-expandable covered stent (14/80 mm Fluency stentgraft; Bard, Murray Hill, USA). The stent was locked in place and the next angiogram indicated proper proximal and distal wall apposition at the height of the pseudoaneurysm. This is when we noticed a bird’s beak deformity and, trying to avoid stent-graft collapse, we added a Protégé GPS 14/16 mm self-expandable stent (Medtronic, Minneapolis, USA) to cover the distal part of the aortic arch and the proximal part of the implanted covered stent. However, the repair revealed a type-I endoleak. We quickly realized that the balloon-expandable covered stent could not fit into the curve of the distal segment of the aortic arch. Blindsided by the second failure and left with no alternatives, we decided on an iliac stentgraft (15/16×93 mm; Jotec, Evita, Hechingen, Germany), a contralateral limb standard for abdominal aortic aneurysm repair. This partially covered the left subclavian artery ostium. However, this required access via the iliac artery since the short shaft of this equipment was not tailored for this part of the arterial tree. Next, the right common iliac artery was exposed, and from this level it was possible to reach the aforementioned position, expand the stentgraft, and finally achieve the total exclusion of the aortic disruption (Figure 2). To finish our procedure, we did a bilateral chest drainage. After that, the patient was referred to the Department of General Surgery, where, due to liver injury, he underwent drainage laparotomy in two stages: first, liver packing as a damage-control surgery; and second, removal of gauze after 4 days. The pelvic fractures were managed conservatively. No neurosurgical intervention was needed. The patient spent 30 days in the Intensive Care Unit (ICU). After 30 days, prior to sending him to his country, the CTA was repeated. The results surprised us; they were far from an optimal result of BAI endovascular treatment. It was obvious that the diameters of the stents and stentgraft deployed were undersized. Fortunately, none of the elements migrated, but the diameter of the aorta was 20—22 mm, resulting in the occurrence of type-IA and -IB endoleaks (Table 1, Figure 3). We decided to remove the three stents (i.e., two stents and the stentgraft) via an endovascular approach, and to deploy a thoracic stentgraft in the same session. The left iliac artery was dissected retroperitoneally, and a 14F, 80-cm sheath (Cook Medical, Bloomington, USA) was deployed. An 18—30 mm endovascular loop (EN Snare Endovascular Snare System, Merit Medical, South Jordan, USA) permitted us to remove all the stents at the same time. We pulled them through to the region of aortic bifurcation. Then, after clamping of the aorta and common iliac arteries, it was possible to safely remove the stents through a 10-mm incision in the distal part of the abdominal aorta, just under the aortic bifurcation. We anastomosed an 8/150-mm Dacron conduit (Hemashield, Maquet, Rastatt, Germany) end-to-side to this incision with a Prolene 5/0 running suture. This artificial passageway enabled safe implantation of a 24/105-mm thoracic stentgraft (Cook Medical, Bloomington, USA). The final angiography confirmed a total exclusion of the pseudoaneurysm (Figure 4). The vascular conduit was cut, leaving a 1-cm stump which was ligated with Prolene 2/0 suture. Seven days after this procedure, the patient was ready to fly back to his country.
Discussion
The five main types of endoleaks (see Table 1) have different causes and require distinct treatments. In our case, massive type-IA and -IB endoleaks were identified (Figure 3). A Type-I endoleak develops when there is a mismatch between the stentgraft and the aorta wall at proximal or distal lending zones. The resulting gap lets blood through into an aneurysm sac, increasing the risk of aneurysm rupture. This type of endoleak is the most dangerous, and necessitates urgent attention due to its high risk of aneurysm rupture.
Endovascular treatment of both children and small-framed adults remains a challenge for vascular surgeons. Although small aortic diameter [10–12] is a feature connecting these two types of patients, this does not help with preoperative diagnostics and treatment. Hemorrhagic shock causes striking autonomic vasoconstriction of the main artery diameter in younger patients. This results in unique challenges in these patients, compared with larger-framed patients. First, no dedicated equipment can be found on the market. Available thoracic stentgrafts cover the range of 21–46 mm in diameter and are intended for thoracic aortic diameters between 16 and 42 mm. Therefore, in life-saving procedures, we can only adapt existing tools as non-standard solutions.
In the case of pediatric patients, open surgical repair prevails as the method of choice [10,13]. Endovascular stentgraft deployment is a universally accepted technique in the adult population, but its use in pediatric patients has been rarely documented, occurring in just a tiny fraction of their overall population. As mentioned, in both these groups of patients – small-framed young adults and children – the main problem for teams operating endovascularly is the small aortic diameter. There is a lack of dedicated stentgrafts for aortas in this size range, allowing only temporal stabilization of the growing subjects. The second obstacle is the small lumen in the femoral and external iliac arteries which, for proper implantation, require prior surgical exposure of the common iliac artery.
Therefore, an initially minimally invasive intervention transforms into a standard open procedure. The third obstacle is the challenge of a graft diameter-adjusting method that could take into account the patient’s somatic growth. In children, an enlarging aorta can be only temporarily sealed with a stentgraft – a balloon-expandable covered stent allowing redilation to match further aortic growth. However promising it may be as a bridge operation and life-saving procedure – and a solution for those awaiting their final surgical reconstruction [14,15] – this modality in children helps only to delay the need for surgical repair until the patient is stable [9,16]. In addition, even then, it has three main disadvantages. Firstly, there is a serious risk of aortic rupture with the balloon expansion. Secondly, the ability to adjust the diameter of the stent to the aorta is also limited. Finally, long-term results are yet to be researched.
With the exception of aortic enlargement over time in growing children, the challenges in small-frame adult patients are similar. In addition, in small-frame people, we face yet another dilemma which is worsened in the case of massive blood loss resulting in shock: we face a dearth of dedicated endovascular equipment, compared with what is offered to regular adult patients. This means that, in life-threatening situations, we have to perform bail-out operations, adopting any endovascular tools fitting the needs of the specific patient at the moment the need arises [6,17]. Trauma patients with hypotension have smaller aortic diameters, as measured by CTA, at admission, compared with those measured by CTA following surgery and hemodynamic stabilization [1,18,19]. Such differences in aortic measurements may be a result not only of hypovolemia or inadequate preoperative CTA evaluation, but also of an autonomic reaction affecting the aortic wall [12,20]. We can be sure that CTA may underestimate the size of large vessels due to hemorrhagic shock. Planning endovascular intervention in such a group of patients, we must take under consideration that our calculations may be about 25–30% overestimated. This is especially important with vessels in young people with no atherosclerosis signs [17], indicating their ability to constrict considerably.
Our patient presented with just such a vasospasm reaction, with a sudden drop in blood flow caused by an autoregulatory vegetative reflex. This phenomenon was responsible for the initial measurement of his aorta and possible miscalculation.
Conclusions
We present a clinical scenario of managing a young, small-framed, and hypovolemic patient. This patient category often proves to be especially challenging in cases of trauma repair. These patients usually present with a dramatic vasospasm reaction caused by hypovolemic shock, and our tools are barely suited to provide a sufficient match for their shrinking vessels. Thus, our experience justifies discussing possible solutions in a larger medical forum.
Figures
References:
1.. Mokrane FZ, Revel-Mouroz P, Saint Lebes B, Rousseau H, Traumatic injuries of the thoracic aorta: The role of imaging in diagnosis and treatment: Diagn Interv Imaging, 2015; 96(7–8); 693-706
2.. Spiliotopoulos K, Preventza O, Green SY, Open descending thoracic or thoracoabdominal aortic approaches for complications of endovascular aortic procedures: 19-year experience: J Thorac Cardiovasc Surg, 2018; 155(1); 10-18
3.. Serra R, de Franciscis S, Grande R, Endovascular repair for acute traumatic transection of the descending thoracic aorta: Experience of a single centre with a 12-years follow up: J Cardiothorac Surg, 2015; 10; 171
4.. Brüls S, Goffin P, Sakalihasan N, Rupture post-traumatique de l’isthme aortique: Perspectives modernes de prise en charge: Rev Med Liege, 2015; 70(9); 415-422 [in French]
5.. Canaud L, Marty-Ané C, Ziza V, Minimum 10-year follow-up of endovascular repair for acute traumatic transection of the thoracic aorta: J Thorac Cardiovasc Surg, 2015; 149(3); 825-29
6.. Wheatley GH, 3rd Burning bridges: Endovascular therapies for acute traumatic aortic transection: J Thorac Cardiovasc Surg, 2015; 149(3); 829-30
7.. Heal ME, Chowdhury SM, Bandisode VM, Traumatic rupture of the thoracic aorta: Ten years of delayed management: J Thorac Cardiovasc Surg; 2005(4); 1-84
8.. Heal ME, Chowdhury SM, Bandisode VM, Balloon-expandable covered stent implantation for treatment of traumatic aortic pseudoaneurysm in a pediatric patient: J Thorac Cardiovasc Surg, 2016; 152(5); 109-11
9.. Keyhani K, Estrera AL, Safi HJ, Azizzadeh A, Endovascular repair of traumatic aortic injury in a pediatric patient: J Vasc Surg, 2009; 50(3); 652-54
10.. Takach TJ, Anstadt MP, Moore HV, Pediatric aortic disruption: Tex Heart Inst J, 2005; 32(1); 16-20
11.. Lin PH, Bush RL, Zhou W, Endovascular treatment of traumatic thoracic aortic injury – should this be the new standard of treatment?: J Vasc Surg, 2006; 43(Suppl. A); 22-29
12.. Yasue H, Kugiyama K, Coronary spasm: Clinical features and pathogenesis: Intern Med, 1997; 36(11); 760-65
13.. Coselli JS, Spiliotopoulos K, Preventza O, Open aortic surgery after thoracic endovascular aortic repair: Gen Thorac Cardiovasc Surg, 2016; 64(8); 441-49
14.. Nano G, Mazzaccaro D, Malacrida G, Delayed endovascular treatment of descending aorta stent graft collapse in a patient treated for post- traumatic aortic rupture: A case report: J Cardiothorac Surg, 2011; 6; 76
15.. Kinlay S, Does this study make my aorta look fat?: Circulation, 2015; 132(17); 1600-1
16.. Branco BC, DuBose JJ, Zhan LX, Trends and outcomes of endovascular therapy in the management of civilian vascular injuries: J Vasc Surg, 2014; 60(5); 1297-307
17.. van Prehn J, van Herwaarden JA, Muhs BE, Difficulties with endograft sizing in a patient with traumatic rupture of the thoracic aorta: The possible influence of hypovolemic shock: J Vasc Surg, 2008; 47(6); 1333-36
18.. Jonker FH, Schlosser FJ, Geirsson A, Endograft collapse after thoracic endovascular aortic repair: J Endovasc Ther, 2010; 17(6); 725-34
19.. Jonker FH, Mojibian H, Schlösser FJ, The impact of hypovolaemic shock on the aortic diameter in a porcine model: Eur J Vasc Endovasc Surg, 2010; 40(5); 564-71
20.. Beltrame JF, Sasayama S, Maseri A, Racial heterogeneity in coronary artery vasomotor reactivity: Differences between Japanese and Caucasian patients: J Am Coll Cardiol, 1999; 33(6); 1442-52
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250