20 October 2020: Articles 
Effectiveness of Levosimendan in an 84-Year-Old Patient with Takotsubo Syndrome Complicated by Acute Heart Failure
Unusual or unexpected effect of treatment
Małgorzata Zalewska-Adamiec1ABDEF*, Małgorzata Chlabicz12BE, Łukasz Kuźma1DF, Hanna Bachorzewska-Gajewska13DE, Sławomir Dobrzycki1DEDOI: 10.12659/AJCR.927081
Am J Case Rep 2020; 21:e927081
Abstract
BACKGROUND: Although takotsubo syndrome (TTS) is usually mild, severe complications such as acute heart failure may occur in the acute phase. Because of the etiology of TTS, typical catecholamines are not recommended; the use of inotropic drugs with a different mechanism of action is recommended, mainly levosimendan.
CASE REPORT: An 84-year-old patient with cardiovascular risk factors, hospitalized in a city hospital because of exacerbation of chronic obstructive pulmonary disease (COPD), was transferred to the clinic with suspected myocardial infarction. At the time of admission, the patient was hemodynamically stable. The coronarography indicated insignificant atherosclerotic lesions in the coronary arteries. The echocardiography revealed apical akinesis and hypokinesis of the apical and middle left ventricular segments (LV). The ejection fraction (EF) was 40%. TTS was diagnosed. After 12 h of hospitalization, the patient developed symptoms of acute heart failure, with deterioration of the LV systolic function (EF 30%). Levosimendan was included in the treatment, which led to an increased blood pressure and clinical improvement after several hours. Over the next few days, the patient’s condition improved and he was transferred to the referral center, from which he was discharged to home.
CONCLUSIONS: In patients with COPD, exacerbation of the disease may be a trigger for TTS. In acute heart failure complicating TTS, administration of levosimendan improves the clinical condition of patients.
Keywords: Pulmonary Disease, Chronic Obstructive, takotsubo cardiomyopathy, Aged, 80 and over, Echocardiography, Heart Ventricles, Simendan
Background
Takotsubo syndrome (TTS) is a stress-induced transient left ventricular (LV) contractility disorder. Usually it is mild, but during the acute period of the disease, serious complications may also occur, i.e., acute heart failure with pulmonary edema or cardiogenic shock, dangerous arrhythmias, and mechanical complications such as heart rupture. The remote prognosis of TTS patients is similar to that of patients with myocar-dial infarction [1,2].
The triggering stressor of TTS can be a mental or physical factor. The most common physical factors are another disease (for example, pheochromocytoma, cancer), a sudden illness (infections, injuries), or exacerbation of a chronic disease, a surgery, or another therapeutic method. Physically induced TTS usually appears to be worse, and severe complications are more common in the acute phase of the disease [1]. Patients with chronic obstructive pulmonary disease (COPD) are particularly susceptible to TTS. The most common stress factor is exacerbation of asthma or COPD, but TTS can also be caused by the constant use of β2-mimetic drugs [3,4].
As the pathomechanism of TTS is still not well known, its treatment, especially in the acute phase, is extremely difficult and the results are uncertain. In TTS, cardiomyocytes are damaged because of excessive activation of β-adrenergic receptors by catecholamines. The drugs recommended for such patients include noncatecholamine-positive inotropic drugs, mainly levosimendan, which not only reverses the negative inotropic adrenaline action but also accelerates the return of the LV systolic function [1].
We present a case of an 84-year-old patient with TTS caused by exacerbation of COPD, complicated by acute circulatory failure, but effectively treated with levosimendan.
Case Report
An 84-year-old smoker with hypertension, carotid and lower-limb atherosclerosis, and chronic kidney disease, hospitalized for a week in a city hospital because of exacerbation of COPD, with suspected myocardial infarction, was transferred to the clinic for diagnosis and invasive treatment. From the morning hours on the day of admission, the patient had sustained an-gina at rest with ischemic electrocardiographic (ECG) changes and a significant increase in troponin levels.
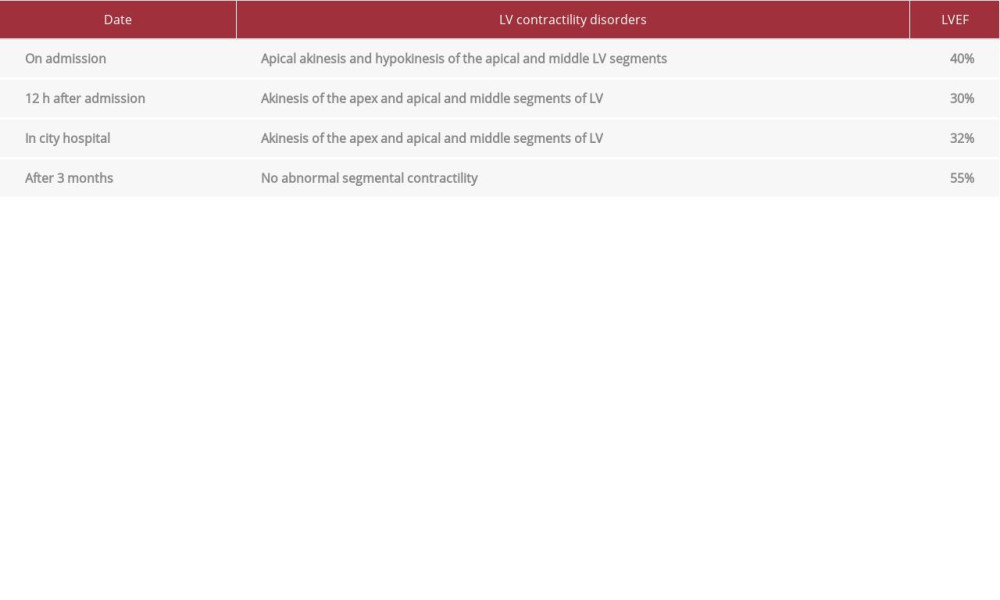
On admission to the clinic, the patient remained hemodynamically stable with chest discomfort; blood pressure (BP) 91/66 mmHg in the ECG recording; sinus rhythm 78/min; ST depression with negative T in leads II, III; aVF V4-V6; QTc 428 ms (Figure 1). Laboratory tests revealed increased values of cardiac enzymes (troponin I 4537.50 ng/L, norm <34.20 ng/L), N-terminal natriuretic peptide type B (17 085 pg/mL), and parameters of renal function (creatinine 1.44 mg/dL, estimated glomerular filtration rate [eGFR] 44.27 mL•min–1 [1.73 m2]–1). The echocardiography revealed apical akinesis and hypokinesis of the apical and middle LV segments, whereas the ejection fraction (EF) was 40% (Figures 2, 3, Table 1). The patient underwent coronarography, which indicated insignificant atherosclerotic lesions in the coronary arteries (Figures 4, 5). TTS was diagnosed.
After 12 h of hospitalization, the patient’s clinical condition suddenly deteriorated, with a decrease in BP (76/44 mmHg), limited contact, and significant deterioration of LV systolic function (akinesis of the apex and apical and middle segments of LV, EF ~30%). Levosimendan was included in the treatment (24-h infusion–initially 0.05 μg kg–1•min–1, then 0.075, and 0.1 μg kg–1•min–1), which resulted in an increased BP and clinical improvement after several hours. During the next few days of hospitalization, a gradual decrease in cardiac enzyme values was observed; electrocardiographic records continuously showed initial ST decreases with negative T-waves, prolonged QTc interval to 522 ms, and many ventricular excitations forming bigeminy (Figure 6). The patient’s condition was gradually improving. Apart from levosimendan, the following were used in the pharmacological treatment: enoxaparin 2×60 mg/day, acetylsalicylic acid 75 mg/day, esomeprazole 40 mg/day, bisoprolol 5 mg/day, ramipril 2.5 mg/day, rosuvastatin 20 mg/day, furosemide 20 mg/day, eplerenone 25 mg/day, and amiodarone (first 2 days of hospitalization). Previously used drugs such as umeclidinium bromide with vilanterol, fenoterol with bromide ipratropium and budesonide, and hydrocortisone were continued in the pharmacotherapy of COPD exacerbation, which was ultimately replaced with prednisone. Pharmacotherapy using amoxicillin with clavulanic acid (1000 mg+200 mg twice a day) was also continued. On the 6th day of hospitalization, the patient was transferred to the city hospital to continue the treatment.
Hospitalization in a city hospital was complicated by duodenal ulcer bleeding (4th day of hospitalization), which was treated with endoscopic adrenaline infiltration followed by intensification of heart failure symptoms, requiring several hours of noradrenaline infusion. The control echocardiography showed continuous LV contractility abnormalities with LVEF 32% (Table 1). Pharmacological treatment was slightly modified; furosemide was replaced with torasemide, and theophylline was added to COPD therapy. On day 10, the patient was discharged in good condition.
After 3 months, an outpatient echocardiographic examination showed that LV systolic function improved, with EF 55% (Table 1). After 1 year, the patient was contacted by phone. He reported that he felt quite good, and did not complain of any retrosternal pains; activity was limited by exercise dyspnea due to COPD. He still smokes.
Discussion
TTS, previously called takotsubo cardiomyopathy, has been known for about 30 years, but its etiology is still unclear. In most patients, its occurrence is preceded by a stress factor. As a result of the stressor, the concentration of catecholamines increases, and the β-adrenergic receptors are excessively activated in cardiomyocytes, which triggers apoptosis and results in myocardial cell damage.
Patients with chronic respiratory diseases constitute about 20% of the TTS population [5]. In patients with exacerbation of chronic respiratory diseases such as asthma or COPD, as well as those taking β-mimetic drugs, the sympathetic nervous system is automatically overactive, which may result in coronary microcirculation disorders. The resulting disturbances in myocardial perfusion mainly result in its stunning and slight damage. The treatment of takotsubo in patients with COPD is particularly difficult, as most of them require continuation of therapy with β-mimetic drugs.
Treatment of TTS complicated with acute heart failure has been a significant clinical problem for years. According to the position of the European Society of Cardiology from 2018, the use of catecholamines, especially dobutamine and dopamine, is not recommended because their administration may exacerbate the damage to cardiomyocytes and cause hemodynamic disorders. The recommended drugs in such patients are noncatecholamine-positive inotropic drugs, mainly levosimendan [6]. The studies conducted so far have shown that levosimendan reverses the negative inotropic effects of adrenaline, but also accelerates the recovery of LV systolic function [7]. The beneficial effect of levosimendan in the treatment of acute heart failure complicating TTS is due to a completely different mechanism of action from catecholamines. Levosimendan enhances the calcium sensitivity of cardiomyocytes, which improves myocardial contractility. It also has a vasodilatory effect [8]. Rapid clinical improvement was observed in the presented patient after infusion of levosimendan. However, during hospitalization, no significant improvement in LV systolic function was found, which most probably results from the patient’s needed use of β-mimetic drugs.
Chronic kidney disease is a limitation to the use of levosimendan. The drug and its metabolites are excreted mainly in urine; therefore, caution is advised when using the drug in patients with mild and moderate renal impairment. However, levosimendan is not recommended for patients with eGFR <30 mL•min–1 (1.73 m2)–1. In these patients, the use of classic catecholamines with an indication for norepinephrine remains. Chronic kidney disease in the presented patient was not a contraindication for the use of the drug. After its administration, an improvement of the clinical condition and temporary improvement of kidney function, previously observed in clinical trials, were observed [9].
Levosimendan, although a very effective drug, is not without side effects. The main side effects are cardiac arrhythmias, which were also observed in the present case. The most common findings were ventricular tachycardia, but also often atrial fibrillation or additional ventricular beats [10]. Our patient had numerous additional ventricular contractions in the form of ventricular bigeminy, which occurred during the levosimendan infusion and recurred throughout the entire hospitalization period. They did not resolve even after amiodarone administration, which was discontinued because of low efficacy and QTc prolongation.
The case of our patient is an example of the efficacy of levosimendan in the treatment of acute heart failure complicating TTS. The first observational and randomized studies with the use of levosimendan in TTS reported a faster improvement of the LV systolic function and better physical capacity determined by the New York Heart Association class in the group of patients treated with levosimendan [11,12]. These first reports indicate that levosimendan will probably be a necessary drug in the treatment of TTS complicated with acute heart failure.
Conclusions
In patients with COPD, exacerbation of the disease may be a trigger for TTS. In acute heart failure complicating TTS, administration of levosimendan improves the clinical condition of patients.
Figures
References:
1.. Ghadri JR, Wittstein IS, Prasad A, International expert consensus document on takotsubo syndrome (part I): Clinical characteristics, diagnostic criteria, and pathophysiology: Eur Heart J, 2018; 39(22); 2032-46
2.. Zalewska-Adamiec M, Bachorzewska-Gajewska H, Tomaszuk-Kazberuk A, Takotsubo cardiomyopathy: Serious early complications and two-year mortality – A 101 case study: Neth Heart J, 2016; 24(9); 511-19
3.. Patel B, Assad D, Wiemann C, Zughaib M, Repeated use of albuterol inhaler as a potential cause of Takotsubo cardiomyopathy: Am J Case Rep, 2014; 15; 221-25
4.. Kansara T, Dumancas C, Neri F, Rare association of takotsubo cardiomyopathy with right bundle branch block in the dual setting of asthma exacerbation and psychiatric illness: Am J Case Rep, 2020; 21; e920461
5.. Almendro-Delia M, Núñez-Gil IJ, Lobo M, Short- and long-term prognostic relevance of cardiogenic shock in takotsubo syndrome: Results from the RETAKO registry: JACC Heart Fail, 2018; 6(11); 928-36
6.. Ghadri JR, Wittstein IS, Prasad A, International expert consensus document on takotsubo syndrome (part II): Diagnostic workup, outcome, and management: Eur Heart J, 2018; 39; 2047-62
7.. Paur H, Wright PT, Markus B, High levels of circulating epinephrine trigger apical cardiodepression in a 2-adrenergic receptor/Gi-dependent manner; A new model of takotsubo cardiomyopathy: Circulation, 2012; 126; 697-706
8.. Papp Z, Édes I, Fruhwald S, Levosimendan: Molecular mechanisms and clinical implications: Consensus of experts on the mechanisms of action of levosimendan: Int J Cardiol, 2012; 159(2); 82-87
9.. Hou ZQ, Sun ZX, Su CY, Effect of levosimendan on estimated glomerular filtration rate in hospitalized patients with decompensated heart failure and renal dysfunction: Cardiovasc Ther, 2013; 31(2); 108-14
10.. Mebazaa A, Nieminen MS, Packer M: JAMA, 2007; 297(17); 1883-91
11.. Santoro F, Ieva R, Ferraretti A, Safety and feasibility of levosimendan administration in Takotsubo cardiomyopathy: A case series: Cardiovasc Ther, 2013; 31; e133-37
12.. Guo Y, Zhou C, Yang X, Efficacy and safety of levosimendan in Chinese elderly patients with takotsubo syndrome: Ann Transl Med, 2018; 6(22); 438
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250